Chronic kidney disease has a high prevalence and economic impact, and an increased risk of hospitalization. Although there are public regional and country registries, we have not found references to estimate the impact of renal replacement therapy (RRT) on hospital admissions.
MethodsWe obtained authorization from the ethics committee and health authorities to integrate the REMER [Madrid Kidney Disease Registry] (2013-2014) and Minimum Basic Data Set (2013-2015) databases and to analyze the admissions during the first year of RRT.
Results767 patients started RRT in all the hospitals of our region across all RRT modalities. More than a third of the patients start dialysis during a hospital admission. This unplanned start, more common in HD than PD, shows relevant differences in patient profile or admission characteristics.
Without considering this initial episode, almost 60% of patients were admitted during their first year. The hospitalization rate was 1.2 admissions/patient, higher in HD than in TX or PD; the mean length of stay was 8.6 days.
The estimated cost of admissions during the first year is €12,006/patient. Our analysis ensures the exhaustive inclusion of all episodes and accurate estimation based on the discharge form.
ConclusionThe impact of RRT on hospitals has been underestimated and is very relevant when calculating the total cost of RRT. Results from other countries cannot be extrapolated due to differences in the health system and patient profile. The integration of clinical databases could open up an opportunity that needs only institutional support for its development.
y objetivos La enfermedad renal crónica tiene una alta prevalencia y coste, así como un mayor riesgo de ingreso. Disponemos de registros públicos y obligatorios, pero no hay referencias recientes para estimar el impacto que el tratamiento sustitutivo renal (TSR) tiene en la actividad hospitalaria.
MétodosTras las autorizaciones pertinentes, hemos integrado las bases de datos REMER (2013-2014) y CMBDH (2013-2015) para analizar la actividad hospitalaria durante el primer año de TSR.
ResultadosUn total de 767 pacientes iniciaron TSR en los 7 hospitales de tercer nivel de la Comunidad de Madrid. Más de una tercera parte lo hicieron de forma no programada durante un ingreso. Este inicio es más frecuente en HD que en DP, pero existen diferencias clínicas relevantes en edad y en comorbilidad. Descartando este primer episodio, casi el 60% de pacientes ingresan durante el primer año. La tasa de ingreso es de 1,2 ingresos/paciente, más alta en HD que en TX y DP; la estancia media es de 8,6 días. El coste agregado de los ingresos del primer año es de 12.006 €/paciente. Nuestro análisis asegura la inclusión exhaustiva de todos los episodios y la estimación precisa de costes.
ConclusionesEl impacto del TSR en la actividad hospitalaria ha sido infraestimado y es una parte importante del coste global del TSR. Los resultados de la literatura internacional no pueden extrapolarse a nuestro país por las diferencias en el modelo sanitario y perfil de paciente. La integración de bases de datos clínicas es técnicamente viable y podría abrir una vía inmensa de información que solo requiere apoyo institucional para su desarrollo.
Chronic kidney disease (CKD) is highly prevalent, with high mortality, an important impact in the patient, with a high organizational and economic cost 1. According to the study EPIRCE 2, 9.24% of the adult population in Spain has some degree of CKD and 6.83% would be in stages 3 to 5. Incidence rates of renal replacement therapy (RRT) in Spain are similar to the average of European countries, although Spain maintains a higher prevalence 3. In recent years, the incidence of RRT in the Community of Madrid (CM) has increased gradually, from 123.9 per million population (pmp) in 2013 to 129.1 in 2014 4, being even higher in the entire country, 133.6 pmp and 156.6 pmp in 2013 and 2014 respectively, in the adult population 5.
The health cost of CKD is high, it is estimated to be 2.5% of the National Health System budget and more than 4% of specialized care. This is about 800 million euros per year 1. Approximately 73% of the costs of the incident RRT are from hemodialysis (HD) patients, 21% from kidney transplant patients (TX) and only 6% is spent in patients on peritoneal dialysis (PD) 6. Some studies estimate lower costs for transplantation (TX) after the first year, since the first year includes the cost of surgery, hospital admissions and the initial immunosuppressive treatment 7.
As compared with other chronic diseases, dialysis patients have a high risk of hospital admission. The most frequent complications during the first year are those related to vascular access, infections and congestive heart failure 8,9.
The high rate of hospitalization due to infections or vascular access problems correlates with an increased risk of early mortality 8. In recent years, admission due to cardiovascular processes has increased between 20 and 30% during the first months on dialysis, while admissions from infection has increased by almost 200% during the first two months.
Most of the information available on hospitalization in RRT comes from other countries and cannot be extrapolated to our country because of differences in the health model, risk profile, relative prevalence of RRT techniques and even cultural factors.
In our country it is mandatory to have a registry of RRT in all the regions (autonomous communities), and the annual report is published assembled in the national registry (REER). In addition, the Minimum Basic Set of Hospitalization Data (CMBDH), promoted by the Interterritorial Council of the National Health System in 1987 (Agreement number 30) and mandatory since 1999 (Royal Decree 89/1999), collects demographic and clinical data of all admission in health institutions of the Spanish territory 10.
However, we have not found any recent reference, national or regional, sufficiently extensive and focused directly on analyzing the impact that the RRT has on the specialized activity of the hospitals.
The objective of this project is to integrate these databases, demonstrating their usefulness in estimating the impact that the first year has on RRT in all the third level hospitals of a given autonomous community. The main objective is to calculate the rate of admissions during the first year of RRT, describe the main characteristics and estimate the costs generated. By performing this analysis which includes official databases of mandatory implementation by all hospitals with full range of services, we can guarantee its completeness, accuracy and validity.
MethodsThis project has been favorably evaluated by the Reference Research Ethics Committee, it has been approved by the Technical Committee of the Madrid Registry of Renal Patients (REMER) and it has been authorized by the Ministry of Health of the Community of Madrid, who have considered that the analysis propose is aligned with the objectives established in by REMER 4. The report of the Security Office of Health Information Systems (OSSI) ensures that this study complies with the Organic Law on Data Protection (LOPD) by implementing a strict protocol that controls the location and access to databases and the anonymization of patient records through the irreversible dissociation of their personal and clinical data in a phase prior to any statistical analysis or treatment.
To ensure the inclusion of all the admissions of a given patient, the 7 hospitals of the Community of Madrid (CM) with a complete portfolio of services in RRT are analyzed. These 7 hospitals serve a health area that includes almost 3 million inhabitants 4 and the total of the TX carried out in the community. TXs performed on patients from other communities were excluded for analysis.
A cohort of all patients incident to RRT during the years 2013 and 2014 were selected. According to the REMER criteria, we define as incident patient the resident in the CM who begins his first RRT during the study period. No patient with early mortality is discarded. From this cohort we select, based on the CMBDH, the admissions that occurred during its first year of RRT regardless of the cause, the medical service that had admitted the patient and the duration of hospitalization. Therefore, we collected information of one-year follow-up period from the date that RRT was started, unless there has been a previous event (death or change of RRT technique).
If dialysis (HD / DP) is started on an unscheduled basis during hospitalization, such admission is analyzed independently and is not included in the rate or aggregate cost calculations, since it is an admission prior to the first outpatient dialysis. The admission to receive a renal TX is also not included in these calculations.
The CMBDH is a clinical-administrative database that register all hospital discharges. For analysis, only admissions of one or more days are taken into account. Emergency room visits without admission were not computed.
All CMBDH diagnoses and procedures are coded according to the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-MC). All episodes have been grouped with version 32.0 of the APR-GRD patient classification system ( all patients refined- Diagnosis-Related Groups [GRD]). The Change of the coding system (ICD-10 version) the January 1st, 2016 contributes to justify the closing time limit.
The REMER selected variables are: demographic information, hospital information, the etiology and the starting modality of RRT. From the CMBDH database, by default, it is integrated all the data associated with the admission episodes (date of admission and discharge, admission / discharge medical service, main diagnosis, secondary diagnoses, procedures, major diagnostic category [CDM], GRD, degree of severity and risk of mortality at the admission and the diagnoses Present on Admission (POA), that establishes whether or not a diagnosis was present in the patient upon admission to the hospital. If the patient is transferred to another medical service, we consider that the reference service is the one that dictates the patient´s Hospital discharge.
The degree of severity and mortality risk is calculated from the classification and grouping of patients by APR-GRD. This novel classification allows to compare the risk of expected death (by severity) with the actual mortality rate. This type of analysis is being progressively implemented as another element in the control of healthcare quality.
The Charlson index at the time of admission has been calculated from the CMBDH. We use the Deyo modification on the diagnoses collected in the CMBDH and the demographic data; a program routine is applied in Stata (charlson.ado) designed for medical records based on ICD-9-MC 11. Since the REMER database does not include the Charlson index, so we cannot make comparisons with patients that have not been admitted.
To estimate the admission rate due to previous cardiovascular disease, we have considered the POA diagnoses grouped under the following ICD-9 codes: Ischemic heart disease (410-414), Other forms of heart disease (420-429), Cerebrovascular disease (430- 438) and Diseases of the arteries, arterioles and capillaries (440-449).
StatisticsQuantitative variables, are expressed as mean and standard deviation (SD) or median and interquartile ranges (ICR) in the case that the variable does not follow a normal distribution. Categorical variables are presented as percentages. Comparisons between quantitative variables are analyzed using Student's t if the data follows a normal distribution or with Mann Whitney's U if the distribution is not normal. Differences between categorical variables are compared using a χ2 (chi-square). The follow-up time has been calculated as the difference between the starting date and the end date of treatment (or 31 Dec. 2015 if the data is censored). In the case of a transplanted patients, the date of initiation of RRT is considered the day of discharge after the kidney transplant surgery. The admission rate has been estimated as the number of admissions per patient, and the admission rate for cardiovascular reasons, as the number of admissions per patient and year.
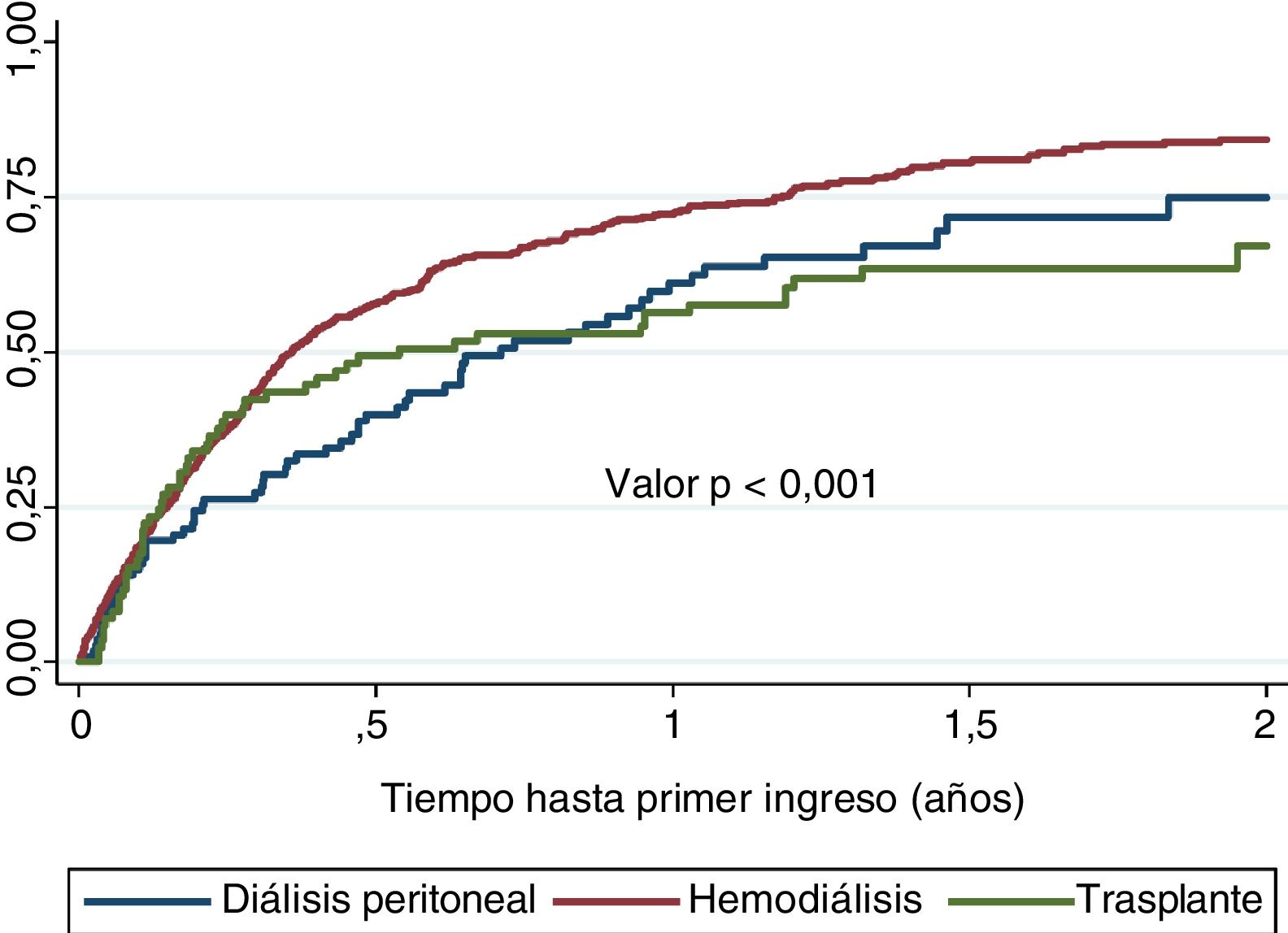
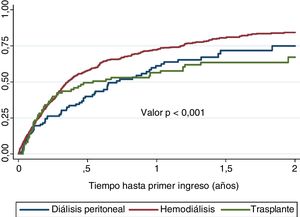
The time until the first admission has been estimated using Kaplan-Meier, and the differences between modalities have been established with the log-rank test.
The CMBDH database allocates a cost for each GRD on discharge. This cost is the approximate average value considering all the elements of: hospitalization, personnel, drugs, procedures, dialysis in the hospital and other interventions. From here we estimate the average cost per admission, and during the first year of follow-up in a patient incident on RRT. The cost for the first year is calculated by dividing the cost of all admissions by the number of patients who have initiated RRT, independently of whether they have be admitted to the hospital or have died before completion of one year follow-up.
All analyzes have been performed with Stata14 (StataCorp2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.X).
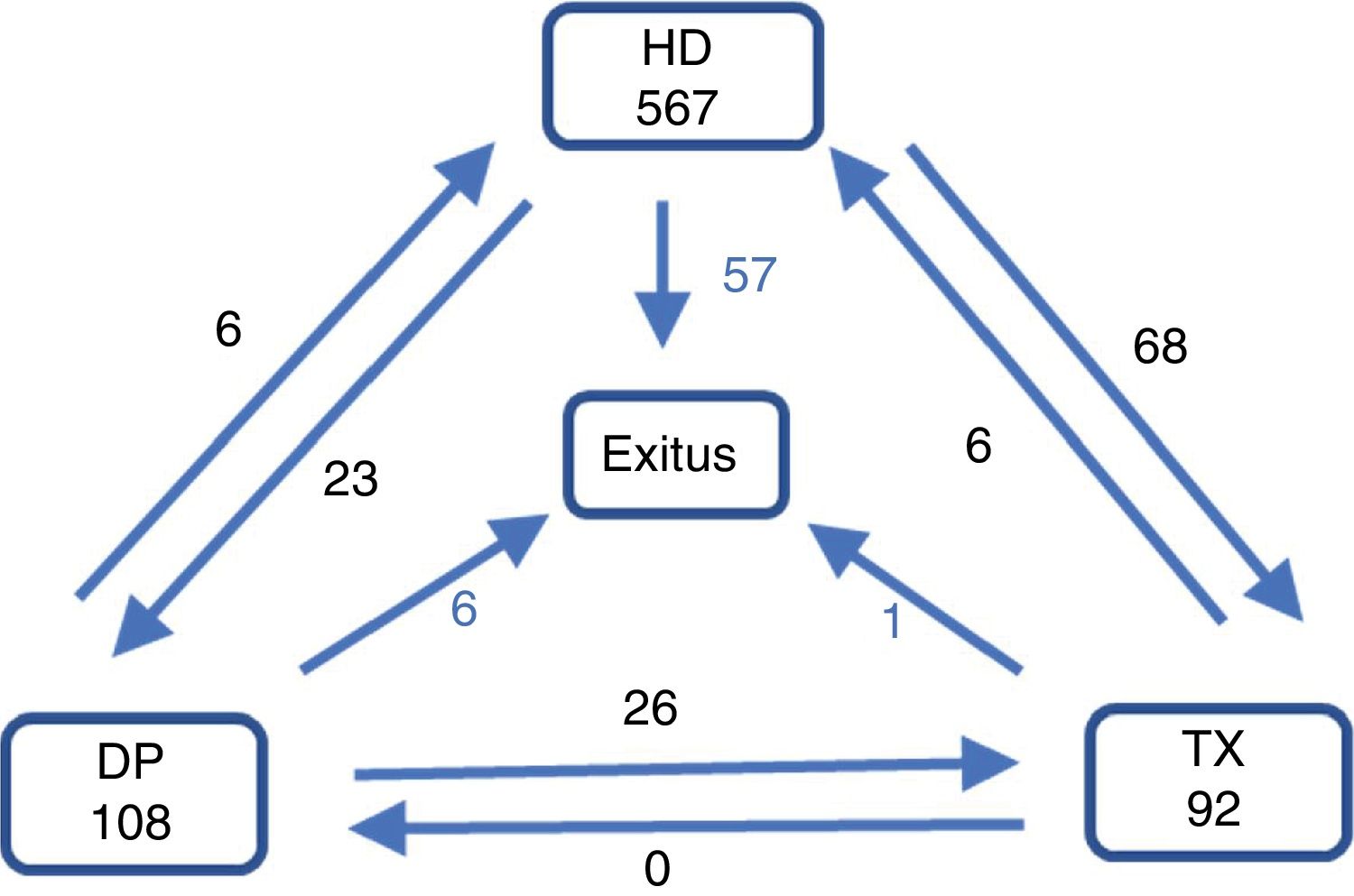
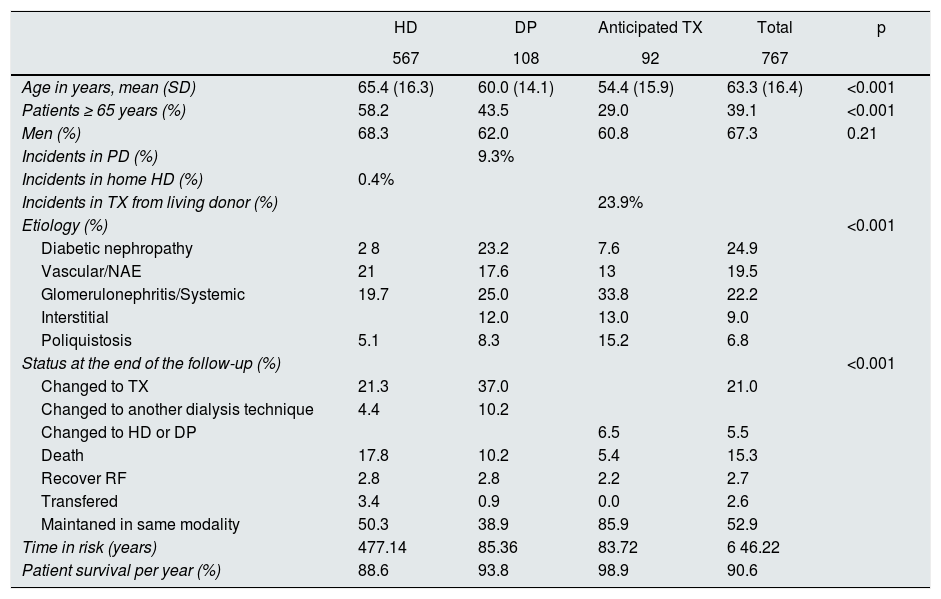
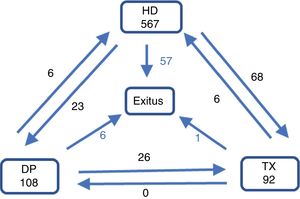
ResultsDescription of patients cohortDuring the 2013-14 period, a total of 767 patients started RRT; 108 in PD (14.1%), 567 in HD (73.9%) and 92 were TX (12.0%). Mean age was 63.3 (SD: 16.4). Patients receiving a kidney graft before starting dialysis were younger than those initiating PD or HD (54.4 vs 60.0 and 65.4 years respectively, p < 0.001, Table 1). The main cause of CKD was diabetes mellitus (24.9%), followed by nephroangiosclerosis (NAE)/vascular disease (19.5%) and glomerulonephritis (16.7%).
Description of patients incident to renal replacement therapy.
| HD | DP | Anticipated TX | Total | p | |
|---|---|---|---|---|---|
| 567 | 108 | 92 | 767 | ||
| Age in years, mean (SD) | 65.4 (16.3) | 60.0 (14.1) | 54.4 (15.9) | 63.3 (16.4) | <0.001 |
| Patients ≥ 65 years (%) | 58.2 | 43.5 | 29.0 | 39.1 | <0.001 |
| Men (%) | 68.3 | 62.0 | 60.8 | 67.3 | 0.21 |
| Incidents in PD (%) | 9.3% | ||||
| Incidents in home HD (%) | 0.4% | ||||
| Incidents in TX from living donor (%) | 23.9% | ||||
| Etiology (%) | <0.001 | ||||
| Diabetic nephropathy | 2 8 | 23.2 | 7.6 | 24.9 | |
| Vascular/NAE | 21 | 17.6 | 13 | 19.5 | |
| Glomerulonephritis/Systemic | 19.7 | 25.0 | 33.8 | 22.2 | |
| Interstitial | 12.0 | 13.0 | 9.0 | ||
| Poliquistosis | 5.1 | 8.3 | 15.2 | 6.8 | |
| Status at the end of the follow-up (%) | <0.001 | ||||
| Changed to TX | 21.3 | 37.0 | 21.0 | ||
| Changed to another dialysis technique | 4.4 | 10.2 | |||
| Changed to HD or DP | 6.5 | 5.5 | |||
| Death | 17.8 | 10.2 | 5.4 | 15.3 | |
| Recover RF | 2.8 | 2.8 | 2.2 | 2.7 | |
| Transfered | 3.4 | 0.9 | 0.0 | 2.6 | |
| Maintaned in same modality | 50.3 | 38.9 | 85.9 | 52.9 | |
| Time in risk (years) | 477.14 | 85.36 | 83.72 | 6 46.22 | |
| Patient survival per year (%) | 88.6 | 93.8 | 98.9 | 90.6 |
SD: standard deviation; PD: peritoneal dialysis; APD: peritoneal dialysis with cycler; RF: renal function; HD: hemodialysis; NAE: nephroangiosclerosis; TX: kidney transplant.
At the end of the first year, 71.1% remain in the same modality of treatment, 16.8% had changed (12.3% have been transplanted, 8.3% have died, 2.2% have recovered renal function and in 1.6 % the follow-up was lost (Fig. 1). The cumulative follow up was 646.22 years (0.8 year / patient).
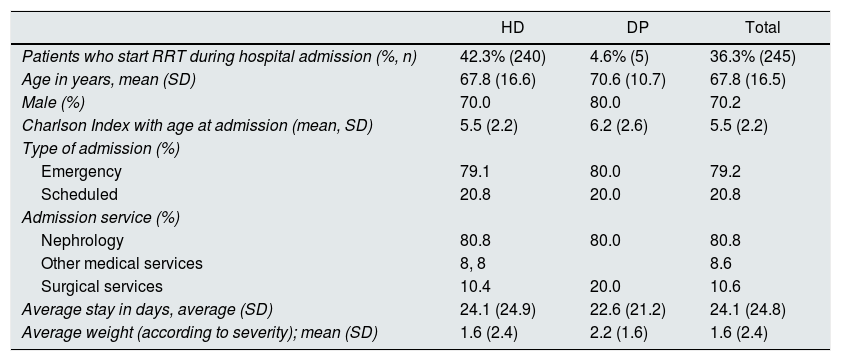
Admissions to initiate dialysisA 36.3% of patients incidents in dialysis initiate their RRT during a hospital admission. These patients were older and with more comorbidity, especially in those that were started on PD. As compared with the cohort of incident patients there was a lower percentage of patients with polycystic kidney disease (1.6 vs. 6.8%) and more patients with NAE / vascular disease (24.1 vs. 19.5%). A 37.6% had DM and 60% had a previous diagnosis of cardiovascular disease (Table 2).
Description of the characteristics of the patients who begin dialysis during a hospital admission.
| HD | DP | Total | |
|---|---|---|---|
| Patients who start RRT during hospital admission (%, n) | 42.3% (240) | 4.6% (5) | 36.3% (245) |
| Age in years, mean (SD) | 67.8 (16.6) | 70.6 (10.7) | 67.8 (16.5) |
| Male (%) | 70.0 | 80.0 | 70.2 |
| Charlson Index with age at admission (mean, SD) | 5.5 (2.2) | 6.2 (2.6) | 5.5 (2.2) |
| Type of admission (%) | |||
| Emergency | 79.1 | 80.0 | 79.2 |
| Scheduled | 20.8 | 20.0 | 20.8 |
| Admission service (%) | |||
| Nephrology | 80.8 | 80.0 | 80.8 |
| Other medical services | 8, 8 | 8.6 | |
| Surgical services | 10.4 | 20.0 | 10.6 |
| Average stay in days, average (SD) | 24.1 (24.9) | 22.6 (21.2) | 24.1 (24.8) |
| Average weight (according to severity); mean (SD) | 1.6 (2.4) | 2.2 (1.6) | 1.6 (2.4) |
SD: standard deviation; PD: peritoneal dialysis; HD: hemodialysis
The average period (AP) of the first admission was 24.1days (SD 24.8) and AP adjusted for dialysis technique was 19.1 days (11.7), with no difference between DP and HD (p = 0.6). The calculated complexity of the admission is 1.65 (SD: 2.39); it was higher in PD than in HD (2.15 vs. 1.64), and more than two thirds of the admissions were for severe or very severe clinical problems.
Most of the admission to initiate RRT are recommended by the emergency room doctors (79.2%) and only 20.8% had been programmed, with very similar percentages in both techniques (HD / DP). Most patients were discharged by the nephrology service (80.8%) and the reason for admission were related to diseases of the cardiovascular (38.8%) or genitourinary system (33.9%).
A 13.5% of patients who initiate RRT during a Hospital admission die during the first year of treatment. The main cause of mortality was infection (42.4%), followed by cardiovascular causes (27.3%) and cancer (12.2%).
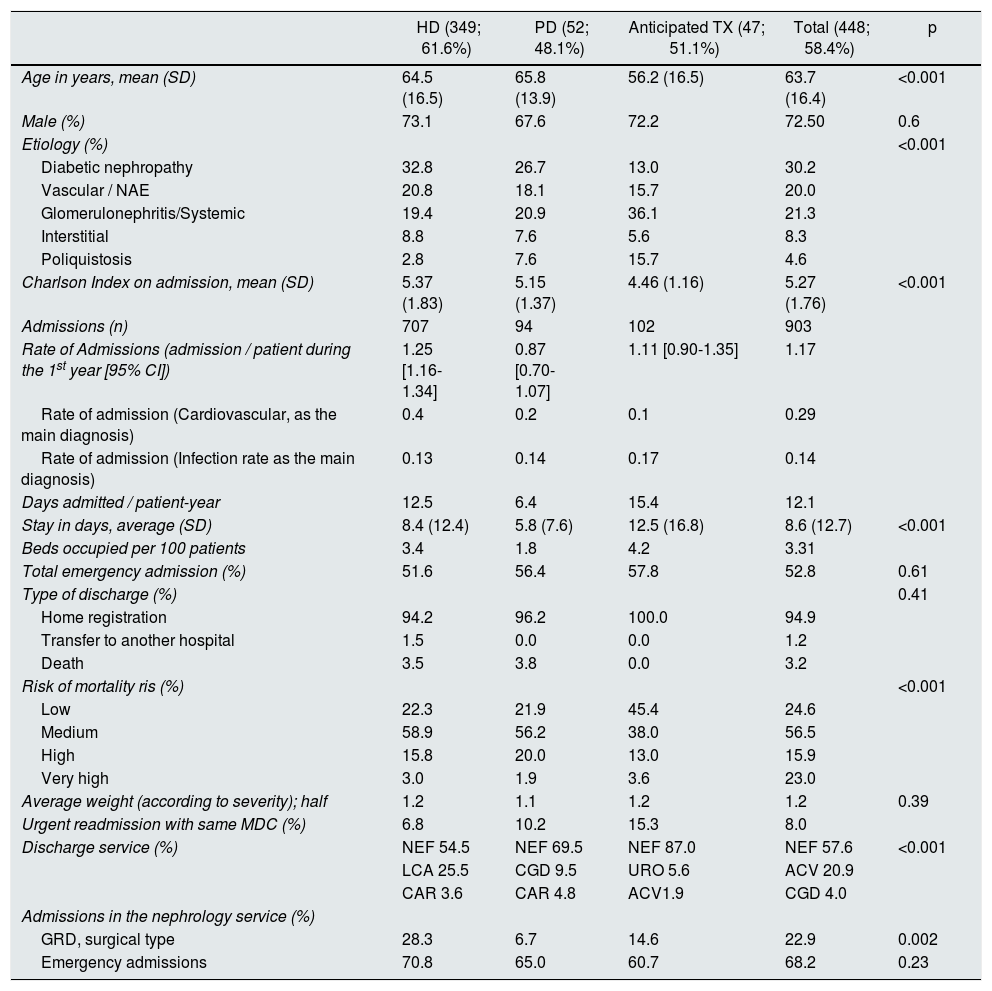
Admissions during the first year in renal replacement therapyApart from the initial admission to start RRT and the admission to receive a renal TX, a 58.4% of patients are admitted to the hospital during the first year of RRT. A total of 903 admissions were recorded: 10.0% were PD patients, 78.0% HD and 11.0% TX. The admission rate during the first year was 1.18 admissions per patient, and the average number of days staying in the hospital per patient during the year of follow-up, was 12.05 days. The number of days in the hospital was 8.6 days (SD: 12.7) shorter in PD patients. Almost half of the admission were due to an emergency and only 3.2% die during an admission (Table 3).
Characteristics of hospital admission during the first year in patients on renal replacement therapy (RRT). Hospital admission to initiate RRT are excluded.
| HD (349; 61.6%) | PD (52; 48.1%) | Anticipated TX (47; 51.1%) | Total (448; 58.4%) | p | |
|---|---|---|---|---|---|
| Age in years, mean (SD) | 64.5 (16.5) | 65.8 (13.9) | 56.2 (16.5) | 63.7 (16.4) | <0.001 |
| Male (%) | 73.1 | 67.6 | 72.2 | 72.50 | 0.6 |
| Etiology (%) | <0.001 | ||||
| Diabetic nephropathy | 32.8 | 26.7 | 13.0 | 30.2 | |
| Vascular / NAE | 20.8 | 18.1 | 15.7 | 20.0 | |
| Glomerulonephritis/Systemic | 19.4 | 20.9 | 36.1 | 21.3 | |
| Interstitial | 8.8 | 7.6 | 5.6 | 8.3 | |
| Poliquistosis | 2.8 | 7.6 | 15.7 | 4.6 | |
| Charlson Index on admission, mean (SD) | 5.37 (1.83) | 5.15 (1.37) | 4.46 (1.16) | 5.27 (1.76) | <0.001 |
| Admissions (n) | 707 | 94 | 102 | 903 | |
| Rate of Admissions (admission / patient during the 1st year [95% CI]) | 1.25 [1.16-1.34] | 0.87 [0.70-1.07] | 1.11 [0.90-1.35] | 1.17 | |
| Rate of admission (Cardiovascular, as the main diagnosis) | 0.4 | 0.2 | 0.1 | 0.29 | |
| Rate of admission (Infection rate as the main diagnosis) | 0.13 | 0.14 | 0.17 | 0.14 | |
| Days admitted / patient-year | 12.5 | 6.4 | 15.4 | 12.1 | |
| Stay in days, average (SD) | 8.4 (12.4) | 5.8 (7.6) | 12.5 (16.8) | 8.6 (12.7) | <0.001 |
| Beds occupied per 100 patients | 3.4 | 1.8 | 4.2 | 3.31 | |
| Total emergency admission (%) | 51.6 | 56.4 | 57.8 | 52.8 | 0.61 |
| Type of discharge (%) | 0.41 | ||||
| Home registration | 94.2 | 96.2 | 100.0 | 94.9 | |
| Transfer to another hospital | 1.5 | 0.0 | 0.0 | 1.2 | |
| Death | 3.5 | 3.8 | 0.0 | 3.2 | |
| Risk of mortality ris (%) | <0.001 | ||||
| Low | 22.3 | 21.9 | 45.4 | 24.6 | |
| Medium | 58.9 | 56.2 | 38.0 | 56.5 | |
| High | 15.8 | 20.0 | 13.0 | 15.9 | |
| Very high | 3.0 | 1.9 | 3.6 | 23.0 | |
| Average weight (according to severity); half | 1.2 | 1.1 | 1.2 | 1.2 | 0.39 |
| Urgent readmission with same MDC (%) | 6.8 | 10.2 | 15.3 | 8.0 | |
| Discharge service (%) | NEF 54.5 | NEF 69.5 | NEF 87.0 | NEF 57.6 | <0.001 |
| LCA 25.5 | CGD 9.5 | URO 5.6 | ACV 20.9 | ||
| CAR 3.6 | CAR 4.8 | ACV1.9 | CGD 4.0 | ||
| Admissions in the nephrology service (%) | |||||
| GRD, surgical type | 28.3 | 6.7 | 14.6 | 22.9 | 0.002 |
| Emergency admissions | 70.8 | 65.0 | 60.7 | 68.2 | 0.23 |
MCD: major diagnostic category; SD: standard deviation; PD: peritoneal dialysis; DRG: groups related by diagnosis; HD: hemodialysis; IC: confidence interval; NAE: nephroangiosclerosis; RRT: renal replacement therapy; TX: kidney transplant.
The average age of admitted patients was 63.7 years (16.4), with a Charlson index of 5.3 (SD 1.8). The transplanted patients were younger than those who started dialysis (p < 0.001) and have a lower Charlson Index (Table 3). One third of the admissions were patients with DM (30.2%), followed by those with NAE/vascular disease (20%) and with glomerulonephritis (15.3%).
The admission rate due cardiovascular causes was 0.29 admissions / patient-year, and it was lower in renal TX patients than in dialysis patients (HD / DP). The admission rate due to infection of any origin was 0.14 admissions / patient-year and admission due to peritoneal infection in PD was 0.13 admissions / patient-year. The 11 cases admitted because peritonitis had an average hospital stay of 4.6 days (3.2), ranging from1 to 10 days, all with severity 3-4, but no deaths. In HD patients, the admission rate for infection was 0.14 admissions / patient-year; The causes were: 28.3% respiratory infection, 19.8% vascular access infection and 10.4% urinary infection; none of them was a cause of death.
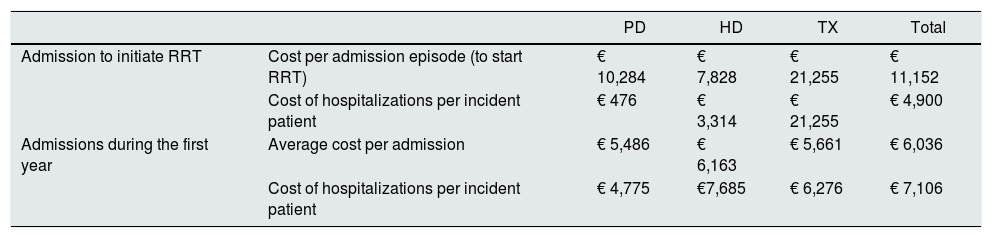
The average cost of admissions during the first year (Table 4 ), estimated by incident patient and according to the GRD and the degree of severity is 5,251€ for PD patient, 10,999 € for HD patients and 27,531€ for TX patients ( including the cost of the transplant procedure: 21,255 €).
Cost of hospital admissions during the first year.
| PD | HD | TX | Total | ||
|---|---|---|---|---|---|
| Admission to initiate RRT | Cost per admission episode (to start RRT) | € 10,284 | € 7,828 | € 21,255 | € 11,152 |
| Cost of hospitalizations per incident patient | € 476 | € 3,314 | € 21,255 | € 4,900 | |
| Admissions during the first year | Average cost per admission | € 5,486 | € 6,163 | € 5,661 | € 6,036 |
| Cost of hospitalizations per incident patient | € 4,775 | €7,685 | € 6,276 | € 7,106 |
PD: peritoneal dialysis; HD: hemodialysis; TX: kidney transplant.
Cost per admission is the total cost divided by the number of admissions. Cost per incident patient is the total cost divided by the number of incidents patients, whether they were admited or not.
The urgent readmission for the same diagnostic category only represents 8% of the admissions (6.8% in HD, 10.2% in PD, 15.3% in TX). The most frequent DRGs in readmissions were "malfunction, reaction or complication of device, graft or genitourinary transplant" (10.0%) and "renal failure" (9.1%).
By Kaplan-Meier it was estimated that the time elapsed from the initiation of RRT to the first admission was 147 days (95% CI: 128-176). According to modalities of RRT, HD had the earliest admissions : 131 days HD (95% CI: 116-151), 260 days for DP ( 95% CI: 177-363) and 197 days for TX ( 95 % CI: 88-435) (log-rank 14.57; p < 0.001) (Fig. 2).
DiscussiónThe present work analyzes, for the first time, to the impact of the first year of RRT on third level hospitals within an entire region in Spain or autonomous community. All admissions were analyzed together, regardless of the indication, hospital service, or hospital. The analysis was performed putting together all public databases that are mandatory to implement in a country where the RRT is covered almost 100% by the public healthcare. We have obtained accurate and up to date estimates of admission rates, their characteristics and costs, which could be of great value in planning decisions, allocation of resources and development of clinical strategies and positions for quality plans. With the methodology used, it is not possible to know the care / economic burden generated by the emergencies, or the attention in consultations of other specialties, since this information is not included in the CMBDH.
Since in patients on RRT the risk of admission is not constant over time on therapy, we have focused on the first year after initiation of RRT. In our study, more than half of the patients were admitted during their first year in RRT, with a rate of more than 1.5 admissions / patient (0.36 admitted for the initiation of RRT and 1.17 for admissions during the first year ) generating an annual cost of more than 12,000 € per patient. The incident patients on HD are admitted more often and mostly due to emergencies, likely due the older age and comorbidity.
The admission rate described is higher than that average estimated by the Dialysis Outcomes and Practice Patterns Study (DOPPS) for Spain and Europe 12. However, we must consider that the study design is different, since DOPPS is not a mandatory registry and only collects data from prevalent patients in HD and from the perspective of the nephrologist, with admissions in their own nephrology service. The same applies to publications in which the information has been collected from private HD centers that have an agreement with public health system to dialyze patients, where there may be a positive selection of less comorbid patients and possibly a partial registration of admissions 13. We must not forget that studies on prevalent patients always have a favorable survival bias of those with lower risk that made them to survive early stages of treatment.
By contrast, the CMBDH data include total admissions of any cause and in any service (more than 40% outside of nephrology), so we consider that the above mentioned publications underestimate the rate of hospitalizations 14,15.
We focused on the first year of RRT, when the admission rate is likely increased 14,16,17, mainly in the first 3 months 9. In fact, some countries exclude from their RRT records patients who die within the first 3 months (i.e, United States of America: USRD) 17. Patients that are transferred to other techniques or die in this initial phase may be older and with greater comorbidity and with more frequent admissions. These circumstances are not contemplated in other registries 17. It is also known that a late referral to nephrology, as well as the non-programmed initiation of HD without definitive vascular access, increased the risk of hospitalization during the first 3 months after the starting RRT 16. Although our data does not go beyond the first year, the domiciliary techniques (DP and TX) are the ones with the lowest rate of admission.
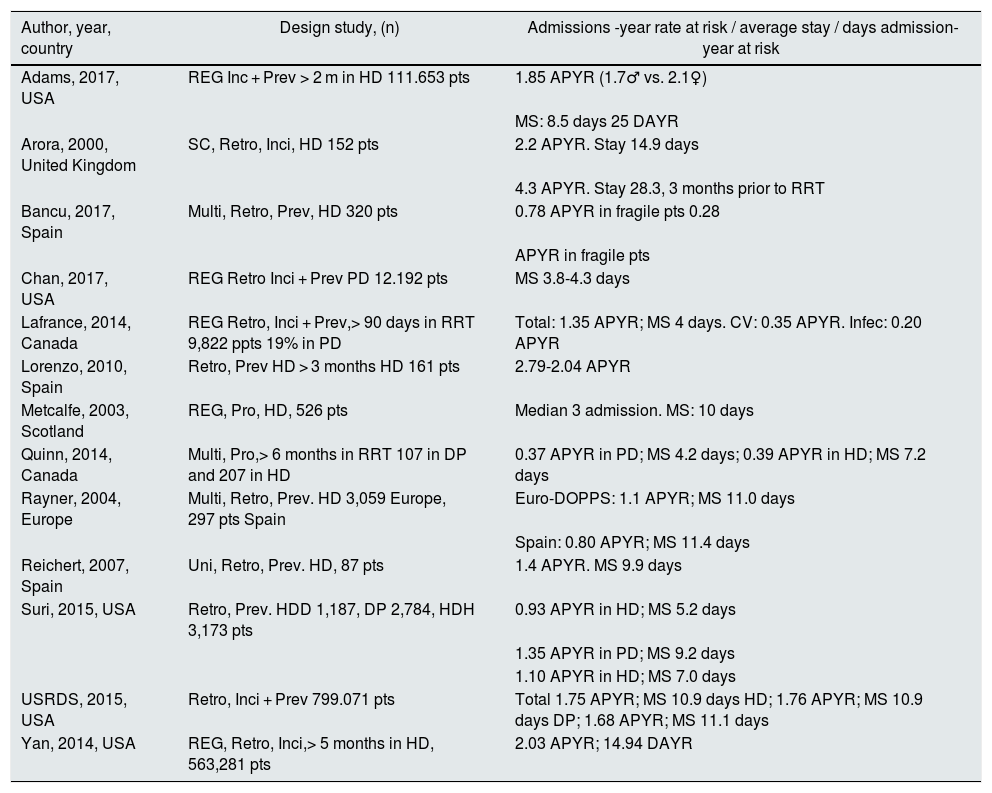
Table 5 contains a summary of the main published references on hospital admissions associated with RRT. It includes the type of study, country, year and sample size, aspects that are very relevant when making comparisons. To understand the tremendous variation in rates, days of admission and overall results, at least, the following methodological aspects must be considered:
- 1
The health model of the country of reference with the different accessibility to RRT techniques and the payer of the treatment.
- 2
The dialysis techniques being considered.
- 3
The hospital, center, or territorial registration reference.
- 4
The profile and inclusion criteria of patients.
- 5
The time of follow-up (first year or prevalent).
- 6
The approach from nephrology service vs. global.
- 7
The voluntary or obligatory completion of records, as well as the clinical or administrative profile of the personnel in charge of the collection of the variables.
Principal studies to estimate admission rates of patients on RRT from 2000 to 2017.
| Author, year, country | Design study, (n) | Admissions -year rate at risk / average stay / days admission-year at risk |
|---|---|---|
| Adams, 2017, USA | REG Inc + Prev > 2 m in HD 111.653 pts | 1.85 APYR (1.7♂ vs. 2.1♀) |
| MS: 8.5 days 25 DAYR | ||
| Arora, 2000, United Kingdom | SC, Retro, Inci, HD 152 pts | 2.2 APYR. Stay 14.9 days |
| 4.3 APYR. Stay 28.3, 3 months prior to RRT | ||
| Bancu, 2017, Spain | Multi, Retro, Prev, HD 320 pts | 0.78 APYR in fragile pts 0.28 |
| APYR in fragile pts | ||
| Chan, 2017, USA | REG Retro Inci + Prev PD 12.192 pts | MS 3.8-4.3 days |
| Lafrance, 2014, Canada | REG Retro, Inci + Prev,> 90 days in RRT 9,822 ppts 19% in PD | Total: 1.35 APYR; MS 4 days. CV: 0.35 APYR. Infec: 0.20 APYR |
| Lorenzo, 2010, Spain | Retro, Prev HD > 3 months HD 161 pts | 2.79-2.04 APYR |
| Metcalfe, 2003, Scotland | REG, Pro, HD, 526 pts | Median 3 admission. MS: 10 days |
| Quinn, 2014, Canada | Multi, Pro,> 6 months in RRT 107 in DP and 207 in HD | 0.37 APYR in PD; MS 4.2 days; 0.39 APYR in HD; MS 7.2 days |
| Rayner, 2004, Europe | Multi, Retro, Prev. HD 3,059 Europe, 297 pts Spain | Euro-DOPPS: 1.1 APYR; MS 11.0 days |
| Spain: 0.80 APYR; MS 11.4 days | ||
| Reichert, 2007, Spain | Uni, Retro, Prev. HD, 87 pts | 1.4 APYR. MS 9.9 days |
| Suri, 2015, USA | Retro, Prev. HDD 1,187, DP 2,784, HDH 3,173 pts | 0.93 APYR in HD; MS 5.2 days |
| 1.35 APYR in PD; MS 9.2 days | ||
| 1.10 APYR in HD; MS 7.0 days | ||
| USRDS, 2015, USA | Retro, Inci + Prev 799.071 pts | Total 1.75 APYR; MS 10.9 days HD; 1.76 APYR; MS 10.9 days DP; 1.68 APYR; MS 11.1 days |
| Yan, 2014, USA | REG, Retro, Inci,> 5 months in HD, 563,281 pts | 2.03 APYR; 14.94 DAYR |
CV: cardiovascular; DAYR: days admitted / year at risk; PD: peritoneal dialysis; MS: average stay; HD: hemodialysis; APYR: admissions per patient and year at risk; Inci: incidents; Multi: multi-center; pac: patients; Prev: prevalence; Pro: prospective; REG: registration; Retro: retrospective; SC: a single center; pts: patients.
Only a few publications analyze this issue based on the reality of the Spanish sytem, almost always with partial areas of concern. The classic studies of Górriz et al. 18 and Gallego et al. 19 in the early years of this century were focused on the impact of the follow-up of advanced chronic kidney disease (ACKD) on the programed initiation of HD, and the study by Remón et al. 20 is limited to peritoneal infection in PD. None of these allow to estimate annual admissions rates in incident RRT patients. The interesting studies of Reichert 21 and Lorenzo et al. 22 were focused on HD, and being from single center, they are hardly generalizable. The study by Conde et al. 23 is a pioneer in estimating the impact of hospitalization on the cost of RRT, but once again it cannot be generalized because it only includes patients from a single center.
Description of admissions during the first year on renal replacement therapyAs in other registries 4, the average age of incident patients in RRT, is increasing progressively, being even higher than the reference published by the PD center group (DPCG) 24. The etiology of renal disease is similar to that described by the REER at the national level 5, with a high prevalence of DM. However, a higher percentage of glomerulonephritis and PKD in both PD and TX stands out. PKD patients have an earlier diagnosis and are frequently followed in advanced CKD clinics, so it is easier for them to start on PD or be transplanted without going through dialysis 25.
Number of days per admission is lower in incidents patients in PD than HD and the TX spent the longest period of admission. As compared with reports from North America the admission are longer in PD and much shorter in the transplant patient. The explanation could be the differences of the health model, in Spain transplant recipients are older with more comorbidity, a majority of donors with expanded criteria versus more living donors more favorable selection profile of donor and recipient in the United States model 17. Data from American show a shorter admission period as compared with Spain, but it should be taken into consideration that the data from America do not include prevalent patients who die within the first 3 months.
Many regional registries do not collect information about admission on RRT (for example, REMER), and if they do, they do not publish the analysis of data in this field. Only the registry from the Basque Country communicates data on hospital admissions, showing an average admission period of 11 days for PD, 13 days for TX and 14.5 days for HD this is information from 2008 from a concerted center 26.
Most patients are admitted in the nephrology service, even in cases where the records indicates a DRG from surgery. Possibly this is due to the complexity of managing our patients and the dependence on their nephrology doctors, thus for the surgeon it is easier to attend the patient while admitted in the nephrology service.
The Department of Health of the Community of Madrid considers inadequate an early discharge with urgent readmissions (within 30 days), due to the same diagnostic category. In our study these readmissions represent less than 10% of the admissions, and the percent is higher in TX than in PD or HD, possibly because part of the clinical incidences of PD and HD can be treated / followed within the HD unit, as an informal model of post-discharge continual medical care. This data is better than in Canadian studies (17.2% in HD) 27 or in North American studies (34% overall, 37% in HD) 17. Another study including only PD patients 28 estimated 14.6% of readmissions at 30 days; the most relevant reasons for admission were myocardial infarction, complications with the procedure and DM; in our series reasons for admission were problems with the device, graft or transplant.
A recent feature of the analysis allows estimating the risks of complications and/or mortality based on the diagnoses present at the admission for a given DRG, classifying them into 4 categories. The comparison with the real mortality in each category provides us with a tool to analyze the quality of care during admission 10 ; In our study, for each DRG the mortality obtained that was lower than expected. We have not found any publication that analyzes this aspect in patients with CKD and / or RRT.
Initiation of RRT during Hospital admissionA primary objective of the Nephrology Strategic Plan of our community of Madrid is a programmed initiation of the RRT after a regular follow up in the advanced chronic kidney failure (ACKD) out patients clinic29. However, more than a third of patients initiate RRT during a Hospital admission which is not considered optimal. Starting RRT while in a hospital admission is considered as a suboptimal situation 18,19. In older series Initiation of RRT during Hospital admission was as high as 50% 18,30 or even 75% of the cases when ACKD clinics were not fully stablished.
Although other countries have published experiences of using PD as an emergency to initiate RRT31, the unscheduled start of RRT is almost always performed by HD in our country, which explains the different rates found in our study for both techniques. If the patient had chosen PD, an early transfer to PD can be proposed after stabilizing their situation with an urgent onset in HD 18. Patients starting dialysis during a hospital admission are older than the rest of the incident cohort, especially in PD, where the difference in age is almost 10 years. Unfortunately, we cannot analyze the impact of comorbidity on the rate of admissions, because we only have that information in those patients that have been admitted.
In our study, the admission for initiation of dialysis entails a duration of more than 2 weeks which is in contrast to the rest of subsequent admissions; this is similar to what was observed in the previously referenced study on initiation of unscheduled dialysis 19.
A non-programed initiation of HD determines a more frequent use of vascular catheters 19 which is associated with a higher rate of hospitalization due to infections 8 and, therefore, at a higher cost 18, in addition to the reduction of patient survival during the first year of RRT 8,18. A13.5% of the patients who started dialysis during a hospital admission died within the first year; this is almost twice than those who did not initate RRT during a hospital admission, which is consistent with studies previously published 18,19.
CostsThe main objective of this study was not an analysis of resources consumption, but it is a great opportunity to estimate cost, which is often undervalued. In fact, the cost of the dialysis technique, pharmacy and even transportation has been estimated quite accurately in our country and has served to define a strategy to support the development of home techniques 7,32. The annual cost is considered 45,170€ for a HD center, 61,280 € for hospital HD, 33,255 € for the PD and 11,766 for TX, averaging the impact of the first year on the half-life of graft and patient 6. However, in these studies the budget of hospitalized care is not considered, or if they do, it is applied a standard cost 33 instead of using the costs associated with GRD 22,23.
Our calculations are very accurate, since we used the cost per GRD rather than a fixed price per day of admission and the estimates average admission days. To the cost of RRT should add more than 7,000€ per incident patient the first year, plus another almost 5,000 € if the initiation of dialysis is performed during admission. In the results section it is described the costs for each of the RRT techniques and the extra cost of initiating non programed RRT while in the hospital admission. These references are of great value for planning and the development of predictive models of the economic impact of interventions that enhance household techniques 34 or the programed start of dialysis with the creation of ERCA consultations and the application of quality models.
But while we wait for the expected revolution of real clinical management and health policy planning based on costs and results of interventions a, we can estimate that, today and in our setting, between 9 and 17% of the cost of TSR corresponds to hospital expenses 14,23,33.
We must not forget that our study focuses on the first year of RRT. Admissions may decrease during the following years and this would explain why admissions are lower in other studies on prevalent patients 23.
Limitations and strengthsIn order to guarantee the inclusion of all hospital admissions of a given patient and analyze the integrated treatment, only the hospitals from the Community of Madrid with a complete portfolio of services have been included in the study. The inclusion of less complex hospitals, without transplant patients or on call services, would increase the statistical power but would make difficult the analysis of cross-hospital admissions. This aspect should be considered in the extrapolation of results to hospitals of a lower level of complexity or with a partial service portfolio. To consider the impact of RRT at the hospital level in a comprehensive manner, the emergency episodes should be included, which cannot be extracted from the MBDS. But one of the advantages of this analysis is that by its nature it encompasses 100% of patients incident to RRT, as well as all their admissions in the Community of Madrid.
Missed opportunity for management analysisOur article evaluates available information that allows the generation of hypotheses with the corresponding new area of research. So far the limitations have been organizational and never technical.
In recent years, health-related data has increased exponentially with an associated increase in medical publications including the term "big data". However, before analyzing the unstructured information and "diving in a sea of data ", we should take advantage of the already available structured databases to obtain relevant information on the real effect of our health interventions. We have databases of public domain, of mandatory implementation, legally protected and often dependent on the same service within the department of Health. By integrating national, regional, hospital records, including clinical, laboratory, etc. databases, and analyzing them together, the information available will increase enormously. The information obtained from structured data will provide the knowledge to design and deploy integrated health care plans and monitor the effects on our population health to ultimately improve management, results and care of our patients.
ConclusionsWe have made accurate estimates of the rates, characteristics and costs of the hospital admissions during the first year of the RRT. The internal validity is ensured by the method of analysis and the origin of the data and they can provide support to the local hospital management and may help to generate strategic plans at regional and national level. The impact of RRT on hospital activity was underestimated; the hospital costs are very relevant for estimating the overall cost of RRT. The results published from other countries cannot be extrapolated to the reality of our country or autonomy due to differences in health model, inclusion criteria, patient profile or various methodological aspects.
The integration of clinical databases is technically feasible, could open an immense path of fluent information and only requires institutional support for its development.
Conflict of interestNone.
We would like to thank the support by the Boards of Directors of the Madrid Society of Nephrology (SOMANE) 2012-2018, of the chiefs of medical service of the hospitals involved and of all the staff that with their daily work contributes to the generation and conservation of REMER records and CMBDH in central services of the Department of Health, as well as the clinical and admission services of the different hospitals.
Please cite this article as: Lopez-Sanchez P, Portolés J, Rodríguez LM, Tornero F, Martin-Vegue AJR, Herrero JA, et al. Impacto del primer año de tratamiento sustitutivo renal en la hospitalización de una comunidad autónoma. Nefrologia. 2019;39:653–663.