Observational retrospective study with consecutive patients with CKD to assess the degree of accomplishment of the therapeutic objectives in hypertension and dyslipidaemia recommended by JNC 8 and KDIGO-2013 CKD guidelines the impact of their implementation compared with previous guidelines.
Results618 patients were included, mean age 67±15 years, 61.33% male. Mean eGFR was 45.99±18.94ml/min, with median albumin/creatinine 26 (0–151)mg/g. A total of 87.6% received antihypertensive treatment and 50.2% received statins. According to KDIGO guidelines, 520 patients (84.14%) should receive statins, but only 304 (58.46%) were receiving them. Patients on statin treatment had more diabetes and hypertension, and a greater cardiovascular history and lower levels of total and LDL-cholesterol.
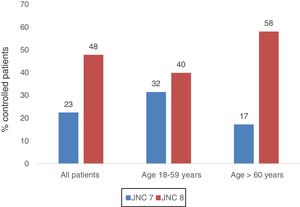
A total of 97.7% of patients were under 60 years of age or had eGFR<60ml/min/1.73m2 or were diabetic, so according to the JNC 8 report, they should have a target blood pressure<140/90mmHg. A total of 289 patients did (47.85%). According to the JNC 7 report, this group had a tighter target blood pressure<130/90mmHg, reducing the number of patients who fulfilled the target: 136 (22.52%). Patients reclassified were older, had a greater cardiovascular history and less DM.
ConclusionThe new KDIGO guidelines for dyslipidaemia treatment increase the indication of statin therapy, especially in patients at high cardiovascular risk. The JNC 8 guidelines improve the percentage of patients with controlled blood pressure, especially the elderly and patients with increased cardiovascular risk, in whom the target blood pressure is currently controversial.
Estudio observacional retrospectivo con pacientes consecutivos con ERC para valorar el grado de cumplimiento de los objetivos terapéuticos en hipertensión arterial y dislipidemia recomendados por las guías JNC 8 y KDIGO-2013 ERC, y el impacto de su aplicación con respecto a las guías previas.
ResultadosSe recogieron 618 pacientes, edad media 67±15 años, el 61,33% varones. El FGe medio era 45,99±18,94ml/min, la mediana de albúmina/creatinina 26 (0-151)mg/g. Un 87,6% recibían tratamiento antihipertensivo y un 50,2% estatinas. Según las guías KDIGO, 520 pacientes (84,14%) deberían recibir estatinas, pero solo 304 (58,46%) las recibían. Los pacientes en tratamiento con estatinas tenían más DM e hipertensión arterial, más antecedentes cardiovasculares y menor nivel de colesterol total y colesterol-LDL.
El 97,7% de los pacientes eran menores de 60 años o tenían FGe<60ml/min/1,73m2 o diabéticos, grupo que según el informe JNC 8 tiene objetivo de presión arterial<140/90mmHg. Cumplían dicho objetivo 289 pacientes (47,85%). Según el JNC 7, estos pacientes tenían un objetivo más exigente, <130/90mmHg, lo que reduciría el número de pacientes cumplidores a 136 (22,52%). Los pacientes reclasificados eran mayores, tenían más antecedentes cardiovasculares y menos DM.
ConclusiónLas nuevas guías KDIGO de tratamiento de la dislipidemia suponen un incremento en la indicación del tratamiento con estatinas, sobre todo en pacientes con elevado riesgo cardiovascular. Las guías JNC 8 mejoran el porcentaje de pacientes con la presión arterial controlada, sobre todo a expensas de los pacientes más mayores y con mayor riesgo cardiovascular, en los que en la actualidad las cifras objetivo de la presión arterial son controvertidas.
In 2013, the Kidney Disease: Improving Global Outcomes (KDIGO) foundation published its clinical practice guideline for lipid management in chronic kidney disease (CKD).1 This guideline modified the previous recommendations, widening the indications for statin therapy to improve the prevention of cardiovascular (CV) disease in patients with CKD. Statin therapy was recommended to all patients over 50 years of age with CKD and to certain subgroups of patients between 18 and 49 years of age with CKD (Table 1). Lipid profile assessment was also recommended in all adults with newly identified CKD, but without specifying new follow-up measures in most patients.
Recommendations for statin therapy according to the 2013 KDIGO guideline for lipid management in CKD.
| Adults>50 years of age with CKD and eGFR<60ml/min/1.73m2(categories G3a–G5) | Statin therapy or statin/ezetimibe combination therapy is recommended (1A) |
| Adults>50 years of age with CKD and eGFR > 60 ml/min/1.73m2(categories G1–G2) | Statin therapy is recommended (1B) |
| Adults aged 18–49 with CKD and one of: | Statin therapy is suggested (2A) |
| -Known coronary heart disease | |
| -Diabetes mellitus | |
| -History of ischaemic stroke | |
| -10-Year risk of coronary mortality or non-fatal myocardial infarction >10% |
CKD: chronic kidney disease; eGFR: estimated glomerular filtration rate; KDIGO: Kidney Disease: Improving Global Outcomes.
In 2014, the panel of members of the Eighth Joint National Committee (JNC 8) published the evidence-based guideline for the management of high blood pressure (HTN) in adults.2 This guideline differed notably on the point of HTN management compared to the previous report by the Seventh Joint National Committee (JNC 7).3 The new guideline changed the target blood pressure (BP), making them less stringent. In adult patients <60 years of age, with an estimated glomerular filtration rate (eGFR)<60ml/min and/or diabetes, the target BP was changed from <130/80mmHg to <140/90mmHg, and in patients >60 years, the target BP was changed from <140/90mmHg to 150/90mmHg.
In a nephrology outpatient clinic, we monitored incident and prevalent patients with CKD, in whom it is important to study the various CV risk factors and risk factors for CKD progression. Taking into account these recent updates on lipid and high blood pressure management, we designed this study to assess the suitability of the various clinical practice guidelines in a sample of patients from our outpatient practice, as well as the impact of the changes to guideline targets in our population.
Material and methodsStudy designA retrospective, descriptive, cross-sectional study was conducted on 652 consecutive, non-screened patients from the nephrology outpatient clinic when they attended a clinical revision at the nephrology outpatient clinic of the Hospital General Universitario Gregorio Marañón between June and December 2012.
PatientsThe patients were men and women between 17 and 90 years of age with stage 1–5 CKD and at least 6 months’ previous follow-up by the nephrology clinic. Patients treated with renal replacement therapy or kidney transplant were excluded.
VariablesDemographic variables were collected, as well as any history of diabetes mellitus (DM) and CV disease: history of congestive heart failure, coronary heart disease, stroke or peripheral vascular disease.
A physical examination including blood pressure was performed on each patient during the visit. BP was measured according to the guidelines of the European Society of Hypertension4: two BP measurements were taken while seated, after a 5min resting period of, using a calibrated mercury sphygmomanometer or a validated oscillometric device. The reference value was the average of the two measurements.
The analytical variables obtained included serum creatinine (using a Hitachi autoanalyser), 24-h urine with albuminuria measurements, and blood lipid levels: total cholesterol, low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C). eGFR was calculated using the abbreviated MDRD equation.5
Finally, data on treatment with lipid-lowering agents and antihypertensives were also collected during the consultation.
ObjectivesThe study's primary objective was to assess the degree of compliance with the therapeutic targets for HTN and dyslipidaemia recommended by the JNC 8 guideline and KDIGO-2013 lipid management guideline, respectively, in patients with stage 1–5 CKD (not receiving renal replacement therapy) in a nephrology outpatient clinic and to assess the impact of the implementation of these new guidelines on patient management compared to previous guidelines.
The secondary objective was to study the characteristics of the population reclassified according to the modifications in the current guidelines.
Data analysisThe qualitative variables were expressed as distribution frequencies, using the chi-square test or Fisher's exact test to compare the proportions. The quantitative variables were expressed as mean±standard deviation, using Student's t-test and the analysis of variance to compare the means. All of the statistical tests were two-tailed and a p-value<0.05 was deemed to indicate statistical significance. The software application SPSS for Windows version 20 was used for the statistical analysis.
ResultsGeneral dataAs many as 618 patients were recruited, with a mean age of 67±15 years. Three hundred and seventy-nine (379) patients (61.33%) were male. 136 patients (20.8%) had DM and 213 (22.01%) had a CV history. The mean eGFR was 45.99±18.94ml/min/1.73m2, with a median albumin/creatinine ratio of 26 (0–151)mg/g. Of the patients studied, 522 (84.47%) had an eGFR<60ml/min and/or albuminuria >30mg/day. Patients on antihypertensive treatment were 87.6% and 50.2% received statins. Table 2 summarises the general characteristics of the sample.
General characteristics of the patients studied.
| Age in years, mean (standard deviation) | 67 (15) |
| Gender, male n (%) | 379 (61) |
| DM (%) | 136 (21) |
| CV history (%) | 213 (22) |
| eGFR, ml/min/1.73m2; mean (standard deviation) | 46 (19) |
| ACR in urine, mg/g, median (range) | 26 (0–151) |
| SBP, mmHg, median (range) | 142 (122–162) |
| DBP, mmHg, median (range) | 78 (66–90) |
| Treated HTN | 571 (88) |
| Number of antihypertensives (drugs/pt), median (range) | 1.97 (0.66–3.28) |
| Statin therapy (%) | 327 (50) |
| Total cholesterol, mg/dl, median (range) | 13 (141–225) |
| LDL-C, mg/dl, median (range) | 104 (71–137) |
| HDL-C, mg/dl, median (range) | 55 (38–72) |
ACR: albumin/creatinine ratio in urine; CV: cardiovascular; DBP: diastolic blood pressure; DM: diabetes mellitus; drugs/pt: drugs per patient; eGFR: estimated glomerular filtration rate, MDRD equation; HDL-C: high-density lipoprotein cholesterol; HTN: hypertension; LDL-C: low-density lipoprotein cholesterol; mg/dl: milligrams per decilitre; SBP: systolic blood pressure.
All values are expressed as median (range) unless otherwise indicated, e.g. by the % symbol or mean (standard deviation) as applicable.
The mean total cholesterol, LDL-C and HDL-C levels in the patients studied were 182.99±42.48; 104.22±33.09 and 54.69±16.97mg/dl, respectively. In our sample. 44.66% of patients had LDL-C levels<100mg/dl; and 12.30%<70mg/dl.
According to the KDIGO guideline, 520 patients from our clinic (84.14%) should have been receiving statins. However, of these patients, only 304 (58.46%) of them were doing so.
We divided the total sample into three groups: patients being treated with statins in whom statins were indicated: 327 (50.20%); patients not being treated with statins in whom statins were indicated; 215 (33.00%); and patients not being treated with statins in whom statins were not indicated: 76 (11.70%).
The characteristics of these three groups of patients were analysed and it was found that among patients in whom statins were indicated who were actually being treated with statins, there was a higher proportion of patients with DM and HTN, with more CV disease and, in relation to statin therapy, they had lower levels of total cholesterol and LDL-C. Table 3 shows the data and the comparison between these groups.
Characteristics of patients with and without statin therapy.
| Statins | No statins but indicated | No statins and not indicated | p | |
|---|---|---|---|---|
| Patients | 327 (50)* | 215 (33)* | 76 (12)* | |
| Age (years) | 70.8 (59.0–82.6)** | 72.1 (61.1–83.1)** | 38.2 (28.3–48.1)** | <0.001 |
| Gender (male) | 205 (63)* | 133 (62)* | 38 (50)* | 0.116 |
| CV history | 169 (52)* | 41 (19)* | 3 (4)* | <0.001 |
| DM | 102 (31)* | 29 (13)* | 5 (7)* | <0.001 |
| Treated HTN | 312 (95)* | 178 (83)* | 47 (62)* | <0.001 |
| Total cholesterol (mg/dl) | 173 (132–215)*** | 194 (152–235)*** | 195 (150–241)*** | <0.001 |
| LDL cholesterol (mg/dl) | 94 (62–125)*** | 117 (88–145)*** | 114 (77–150)*** | <0.001 |
| HDL cholesterol (mg/dl) | 53 (38–69)*** | 56 (38–73)*** | 57 (37–77)*** | 0.130 |
CV: cardiovascular; DM: diabetes mellitus; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol.
The values shown are cases (percentage of total) unless otherwise indicated.
Out of the total number of patients studied, 571 (87.60%) had hypertension and were receiving antihypertensive treatment. The mean number of antihypertensive medications per patient was 1.97±1.31. A 22.23% of them met the criteria for refractory HTN (high BP values >140/90mmHg in spite of treatment with three antihypertensive agents at full doses, at least one of these being a diuretic, or the need for treatment with four antihypertensive medications).
In our sample, 604 patients (97.7%) were under 60 years of age and had an eGFR<60ml/min or an albumin/creatinine ratio (ACR) >30mg/g or the diagnosis of DM. According to the JNC 8 report, this group of patients should have a target BP of <140/90mmHg; 289 patients (47.85%) met this target, with a mean BP of 125.39/72.92 (±11.37/9.33)mmHg. We analysed the characteristics of patients with controlled and uncontrolled BP according to the JNC 8. The patients with controlled BP (BP<140/90mmHg) were younger, had a better eGFR and had less proteinuria. The characteristics of both groups are shown in Table 4.
Characteristics of patients <60 years of age with either eGFR<60ml/min/1.73m2, ACR>30mg/g or diagnosis of DM, with well- and poorly-controlled BP according to the JNC 8.
| BP<140/80mmHg | BP≥140/80mmHg | p | |
|---|---|---|---|
| Prevalence | 289 (48) | 315 (52) | |
| Age in years; mean (standard deviation) | 64 (47–81) | 70.0 (56.0–84.0) | 0.000 |
| Males (%) | 58 | 63 | 0.308 |
| ACR, mg/g; mean (standard deviation) | 20.5 (0–6126) | 39.5 (0–5850) | 0.013 |
| DM (%) | 20 | 22 | 0.116 |
| CV history (%) | 36 | 25 | 0.608 |
| eGFR, ml/min/1.73m2; mean (standard deviation) | 48 (28–68) | 44 (27–61) | 0.013 |
| Drugs, drugs/pt; mean (standard deviation) | 1.8 (0.5–3.1) | 2.2 (0.9–3.4) | 0.000 |
ACR: albumin/creatinine ratio in urine; BP: blood pressure; CV: cardiovascular; DM: diabetes mellitus; Drugs: mean number of antihypertensives; drugs/pt: drugs per patient; eGFR: estimated glomerular filtration rate, MDRD equation.
The values expressed are mean (standard deviation) unless otherwise indicated, e.g. by the % symbol. There are more values expressed as mean (standard deviation) than percentages.
Previously, under the JNC 7 report, this same group of patients (under 60 years of age, with an eGFR<60ml/min or ACR>30mg/g or DM) had a more stringent target BP of <130/90mmHg. According to this recommendation, the number of patients meeting the target would fall to only 136 patients (22.52%).
Then, characteristics of the reclassified patients were analysed; those who would not have achieved the therapeutic targets in the JNC 7 but did achieve the BP control target in the JNC 8. There were 153 of these patients (25.3%). Table 5 shows the comparative characteristics of the patients with controlled BP according to the JNC 7 and according to the JNC 8, as well as the characteristics of this group of reclassified patients. The group of reclassified patients was older, had a more florid history of CV and fewer patients had DM.
Characteristics of patients with controlled BP according to JNC 7, according to JNC 8, and reclassified patients.
| Controlled according to JNC 7 | Controlled according to JNC 8 | Reclassifieda | p | |
|---|---|---|---|---|
| N | 136 (23) | 289 (48) | 153 (27) | <0.001 |
| Age, years (range) | 60.9 (41.9–79.9) | 64.0 (57.0–81.0) | 65.6 (50.0–81.1) | <0.001 |
| Gender (male) | 93 (68) | 169 (58) | 86 (56) | 0.115 |
| eGFR (ml/min/1.73m2) | 55 (25–85) | 53 (26–80) | 51 (29–74) | 0.105 |
| DM | 35 (26) | 57 (20) | 25 (16) | <0.001 |
| CV history | 60 (44) | 103 (36) | 104 (68) | <0.001 |
| Antihypertensives, mean (standard deviation) | 1.7 (0.3–3.1) | 1.8 (0.5–3.1) | 1.8 (0.5–3.1) | 0.074 |
CV: cardiovascular; DM: diabetes mellitus; eGFR: estimated glomerular filtration rate, MDRD equation; JNC 7: Seventh Joint National Committee; JNC 8: Eighth Joint National Committee.
The values shown are cases (percentage of total) unless otherwise indicated.
Finally, only 11 patients (6.14%) in our sample were in the subgroup of patients over 60 years of age with an eGFR>60ml/min. The target BP for this subgroup according to the JNC 8 is <150/90mmHg, which was met by five patients (45.45%). According to the JNC 7, their target would be <140/90mmHg, which was met by only one patient (9.09%).
Table 6 summarises all the percentages of patients with controlled BP according to previous and current guidelines in the various patient groups.
Differences in meeting the JNC 7 and JNC 8 HTN guidelines in patients with CKD.
| JNC 7 | JNC 8 | |
|---|---|---|
| >60 years and eGFR>60ml/min/1.73m2 or ACR>30mg/g or DM | <130/80mmHg | <140/90mmHg |
| 23% controlled | 48% controlled | |
| >60 years and eGFR>60ml/min/1.73m2 | <140/90mmHg | <150/90mmHg |
| 50% controlled | 66% controlled |
ACR: albumin/creatinine ratio in urine; CKD: chronic kidney disease; eGFR: estimated glomerular filtration rate, MDRD equation; HTN: hypertension; JNC 7: Seventh Joint National Committee; JNC 8: Eighth Joint National Committee.
Fig. 1 shows the percentage of patients with controlled BP in total and by age group according to the JNC 8 and JNC 7. It can be seen that the improvement in the percentage of patients with controlled BP under the JNC 8 guideline is primarily a result of better control in patients >60 years of age.
DiscussionThe new guidelines for HTN treatment and lipid management in patients with CKD have a significant impact on the management of our patients in routine clinical practice.
Both dyslipidaemia and HTN are independent CV risk factors and are highly prevalent in patients being followed in nephrology clinics. Adequate control of these factors is a challenge in patients with CKD.
The JNC 8 guideline published in 2014 for the management of HTN is more flexible with BP targets, thereby improving BP control in our patients, especially older patients. In contrast, the KDIGO lipid management guideline published in 2013 has widened the indication of statin therapy in our patients, meaning that the treatment of patients with CKD being followed up in our clinic is now inadequate.
Firstly, the KDIGO foundation's clinical practice guideline for lipid management was published in 2013. This guideline widens the indication of dyslipidaemia treatment in patients with CKD based on coronary artery disease and age, and does not recommend the use of LDL-C as a guide to identify those patients who should be treated with statins, nor as a treatment target. This guideline has been extensively analysed by other groups such as the Kidney Disease Outcomes Quality Initiative (KDOQI), showing support the majority of the recommendations, but they highlight some areas as too strict or requiring clarification.6 In our sample, it is worth noting that 87.21% of patients met the requirements to start statin therapy according to the new KDIGO guideline, but only 58.10% of those who met the requirements actually received the medication. Attention has also been drawn to a very significant increase in the statin prescription rate required by the implementation of the KDIGO guideline by other groups such as Schneider et al., who studied a population of 5217 German adults with CKD and observed a need to increase prescription of statins from 47% to 88%7; this is in line with our data. In our population, a comparison of the subgroup of patients receiving statin therapy with those not receiving it but in whom it is indicated found that these were patients with more profuse history of CV disease, DM and HTN. They had lower rates of total cholesterol and HDL-C, associated with this treatment. In a study conducted in the United States of America with data from the NHANES registry, published in 2014, which studied the impact of the application of the guidelines for the treatment of cholesterol published in 2013 by the American College of Cardiology, observed similar findings. The application of this new guideline means an increase in the indication of statins of >50%, affecting over 12.8 million people and above all increasing the indication in older patients and those with increased CV risk.8
In the future, it will be necessary to assess the impact of the application of this guideline, which increases the indication of the prescription of statins, especially in the high-CV risk population, on the prevention of CV events and mortality.
In relation to BP, the majority of our patients (97.7%) were in the group of patients under 60 years of age with either an eGFR<60ml/min, ACR>30mg/g or a diagnosis of DM. Analysing the general differences between patients with controlled and uncontrolled BP according to the new JNC 8 guidelines, patients who achieve the target BP are younger, with better kidney function and less proteinuria. Although the percentage of patients with controlled BP in our sample according to the current guidelines has improved, it remains insufficient at only 47.85%, reflecting a need to increase BP control efforts in our population. Two other studies presented by our group also evaluated the suitability of the guidelines at that time: in 2003 we presented a study of 1004 patients, 24% of whom achieved BP values <130/85mmHg,9 and in 2007 we presented 600 patients, 35% of whom achieved BP levels <130/80mmHg.10
The new JNC 8 clinical practice guidelines for the management of HTN is more flexible with BP targets, with the result that in our sample of patients with an eGFR<60ml/min or ACR>30mg/g, with DM or <60 years of age, the percentage of patients with controlled BP has increased from 22.4% to 47.5% as compared with the targets indicated in the preceding JNC 7 guidelines. When drafting the JNC 8 guidelines, the investigators included randomised, controlled clinical trials that indicated that there was no benefit in tighter BP control (below 140/90mmHg) in this group of patients. However, the results of the studies on which those guidelines were based were disputed and did not have a high level of evidence. The most relevant of them, the ACCORD study conducted on more than 4000 patients, did not find a significant difference in the frequency of CV events in patients with tight BP control (SBP<120 vs. <140mmHg), but only diabetic patients were included.11 The SPS3 trial studied patients with a history of lacunar stroke, and although it did not observe a decrease in the rate of recurrence of infarction in patients with tight BP control (SBP<130mmHg), it did find a significant decrease in the rate of intracranial haemorrhage.12 The Cardio-Sis study did observe a lower incidence of left ventricular hypertrophy and compound CV events in the group with tighter BP control (SBP<130 vs 140mmHg).13 Finally, the Japanese JATOS study also failed to find significant differences in the end-points studied between BP control groups, but did warn of probable age-related interferences that may have obscured the results.14 In light of the above, the JNC 8 recommendations have been extensively re-evaluated by various societies and research groups, generating controversy around the new BP control targets,15,16 and it would at least seem to be widely accepted that these recommendations are no alternative for clinical judgement, and that decisions on medical care must be tailored to each patient.17,18 The recent publication of the results of the SPRINT study19 has further entrenched the debate around the BP control values proposed by the JNC 8. This randomised clinical trial included more than 8000 non-diabetic patients with increased CV risk, with a mean age of 67.9 years, who were randomised to two SBP control targets using the same values as the ACCORD study: strict control (<120mmHg) or standard control (<140mmHg), finding a significant reduction in the appearance of the primary end-point (combination of any CV event or CV mortality), as well as secondary end-points such as all-cause mortality among patients with strict SBP control, leading to the early termination of the study in spite of not having demonstrated effects on kidney disease progression. The meta-analysis of 123 studies conducted by Ettehad et al. and published recently in the Lancet corroborated these results, finding a reduction in CV risk with BP values below 130mmHg.20
When we analyse the reclassified patients in our study, who achieved the target BP according to the 2014 guidelines, but not according to the earlier guidelines, we observed that these patients were older, had a greater CV history and fewer had diabetes. We also observed that the improvement in the proportion of patients with controlled BP was due mainly to an increase in the number of controlled patients >60 years of age, from 17.2% to 58.1%, while in those under 60 the increase was much smaller, from 31.5% to 40%. An American study published in 2014 found similar data on the impact of the application of the JNC 8 guidelines, with an improvement of around 20% in the number of patients with controlled BP, but fundamentally an improvement in BP control in older patients.21 This group of subjects reclassified under the 2014 guidelines is similar to that studied in the SPRINT trial, which demonstrated a significant reduction in the risk of CV events, CV mortality and all-cause mortality, with tighter BP control in older, non-diabetic, high-CV risk patients with a mean age of 67.9 years.17
In any event, in view of the data from the SPRINT study, there is reason to doubt the benefits of relaxing BP targets in the at-risk population (older and with increased CV risk) on CV events and mortality. It would also seem reasonable to review the current clinical practice guidelines on BP control in patients with CKD.
Our study is not without limitations, as it is a single-centre observational study based on a single lab test and BP reading taken during a medical consultation, but it does highlight the important impact of the implementation of the new guidelines for HTN and dyslipidaemia treatment in our patients.
ConclusionThe amended lipid metabolism and HTN treatment recommendations has had a significant impact on the clinical management of our patients. In our population of patients with CKD, the new KDIGO guideline for dyslipidaemia treatment has meant an increase in the indication of statin therapy, especially in patients with increased CV risk. In contrast, the JNC 8 guidelines have increased the percentage of patients with controlled BP, especially in older patients and those with increased CV risk. Nevertheless, in view of the latest research, less stringent control of BP may lead to an increased risk of CV events and mortality in these patients and may require the BP recommendations to be updated, at least for patients with CKD.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Galán I, Verdalles Ú, García de Vinuesa M, Quiroga B, Goicoechea M, Pérez A, Verde E, et al. Impacto de la aplicación del 8.o JNC y de las guías KDIGO-2013 en el control de la hipertensión arterial y los lípidos en una consulta de Nefrología. Nefrologia. 2018;38:373–379.