Dear Editor:
Tuberculosis is associated with a variety of glomerular manifestations. However, association with immunotactoid glomerulopathy has never been reported. We encountered a case of 37-year-old gentleman with such a novel presentation.
A 37-year-old gentleman presented with swelling all over the body for 6 weeks. His past history revealed recent history of pulmonary tuberculosis 9 weeks back. He was presently on 2 drug anti-tubercular treatment (ATT) (isoniazid and rifampicin) after first 8 weeks of 4 drugs, which additionally included pyrazinamide and ethambutol. At the time of diagnosis of tuberculosis, he was also found to have stage 1 hypertension and was started on hydrochlorthiazide 12.5 mg daily. There was no history of hematuria, past renal disease or any other systemic disorder. Physical examination revealed pitting edema and no other notable findings.
Laboratory data showed hemoglobin 10.1 g/dl, white cell counts of 6800, blood urea 68 mg/dl, serum creatinine 1.4 mg/dl, eGFR by MDRD formula 59 ml/min/1.73 m², protein 4.5 g/dl, albumin 1.7 g/dl, cholesterol 356 mg/dl, Hepatitis- B and C and HIV- 1 and 2 negative, ANA and cryoglobulins negative, normocomplementemia, urine – protein 3+, RBC 4-6 and WBC 1-2/hpf, casts-nil and 24-hr urine protein 4.8 g (non-selective). Liver functions tests were within normal limits. An ultrasound guided renal biopsy was performed.
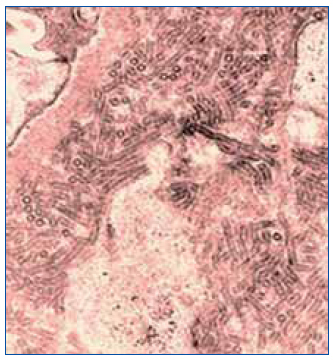
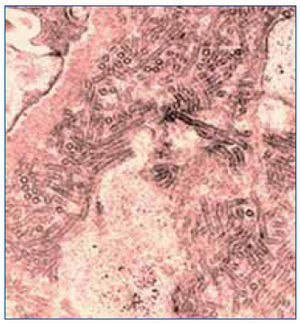
On light microscopy, glomeruli exhibited varying degrees of mesangial expansion, negative silver staining and congo red staining and some thickening of peripheral capillary walls. Immunoflourescence was positive only for IgG in mesangium and peripheral capillary walls. Electron microscopy showed microtubules >30 nm arranged focally in parallel in mesangium suggesting immunotactoid glomerulopathy (ITG) (figure 1). Further work-up showed a negative serum and 24-hr urine immuno-fixation electrophoresis. Imaging studies done for lymphoproliferative disease as an etiology were negative too.
He was treated with ATT for a total of 6 months. His blood pressures were kept under control with ramipril 10 mg daily. His proteinuria decreased to 1.1g/day at 6 months. At 2 years of follow-up, his serum creatinine is 3 mg/dl with eGFR of 23. We offered a repeat renal biopsy during this period which the patent did not consent.
ITG is distinct rare morphologic entity characterized by microtubular glomerular deposits often ranging from 34 to 49 nm in diameter organized in parallel arrays. It usually occurs in older individuals presenting with nephrotic syndrome, hematuria and renal insufficiency. The term was introduced by Schwartz et al in 1980's, where they described this disease as a glomerular disease characterized by highly organized crystalline structure of immune deposits in absence of systemic diseases such as amyloidosis, cryoglobulinemia, paraproteinemia, and systemic lupus erythematosus1. In most instances, an underlying lymphoproliferative disorder is found. Association with HIV, sickle cell disease, hypereosinophilic syndrome and recurrence in transplanted kidneys has been reported2-5.
Our case showed a temporal association with tuberculosis. Though tuberculosis or its treatment is shown to be linked to a variety of glomerular diseases such as amyloidosis, minimal change disease, IgA nephropathy, and collapsing glomerulopathy6-9 but as causality with ITG has never been reported. It is difficult to prove whether tuberculosis per se caused ITG, however treatment of tuberculosis resulted in partial remission.
The exact pathogenesis of ITG remains to be elucidated. Like lymphoproliferative diseases, tuberculosis is also an inflammatory disorder. It might be possible that immune dysregulation in tuberculosis or systemic inflammatory mediators cause defects in critical podocyte cellular functions involved in clearance of filtered and retained immunoglobulins. This would end up in formation of immunotactoids.
The treatment strategies for ITG have been variable, though there has been a case of ITG exhibiting nephrotic syndrome successfully treated with corticosteroids and antihypertensive therapy10. We did not subject our patient to steroids as there was a potential risk of flaring tuberculosis with high doses of corticosteroids. However, we did not try rituximab as data for this agent is limited at present5.
Our patient was relatively young as compared to most other cases and progressed to chronic kidney disease stage 4 over a span of 2 years. The natural course of the disease is progression to end-stage renal disease (ESRD) within 7 months to 10 years. However, in a recent report a patient with a diagnosis of ITG developed acute kidney injury (AKI) and ESRD within 1 week of initial presentation11.
To conclude, to the best of our knowledge, our case is the first report of an association of ITG with tuberculosis. There could be a possible causal relationship between mycobacterial infections and ITG. In addition to search for lymphoproliferative disorder and HIV, tuberculosis as an etiology should be kept in mind in a case of ITG.
Figure 1. Microtubular deposits of >30 nm seen in mesangium (on electron microscopy magnification x15000).