Renal transplantation is the treatment of choice in patients with advanced chronic kidney disease (CKD) as it improves the quality of life and survival of patients.1
Vascular complications of renal transplantation represent an important cause of morbidity and mortality, and frequently lead to early graft loss,2 which is around 5% in the most recent series.3 A 4–10% of patients who start dialysis have a non-functioning kidney graft, and up to 32% of cases require transplantectomy for various reasons.4 The mortality of these patients is greater than those with functional graft or in renal replacement therapy without previous transplantation.5 Current indications for transplantectomy include early graft loss, intolerance syndrome, severe proteinuria, recurrent pyelonephritis, neoplasia, and chronic inflammation syndrome.6 Early vascular complications of transplantation may cause the loss of the graft and the need for transplantectomy.
The performance of express transplant seeks to obtain the benefit of performing an inevitable transplantectomy with the implantation of another graft in the same surgical act. This improves both quality of life and survival of the patient,5 in addition to ameliorating the psychological problem of early graft loss.
In patients with terminal liver disease, re-transplantation after early graft loss is common otherwise the prognosis is very poor.7 In renal transplantation, such a degree of urgency does not exist due to the availability of other renal replacement techniques,1 thus re-transplantation is not performed early.
The term express used here as the definition made by the Royal Spanish Language Academy “with maximum speed”.8
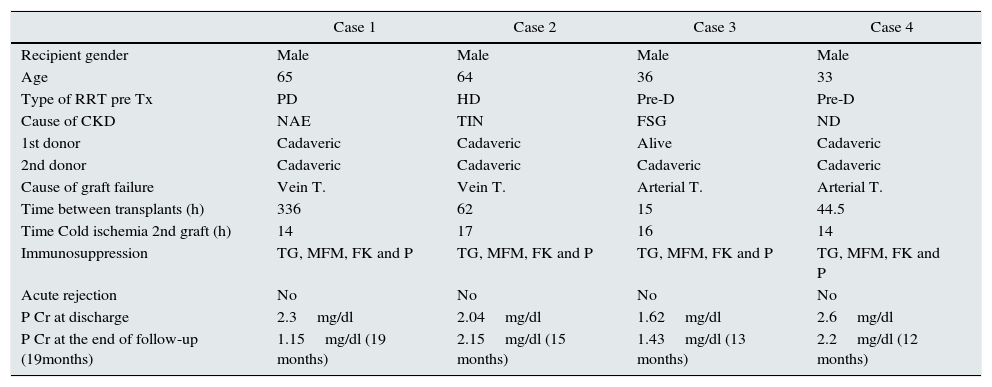
We have performed a total of 4 express transplants over a period of 2 years, describing their characteristics and evolution in Table 1.
Summary of case description of transplant “express”.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Recipient gender | Male | Male | Male | Male |
| Age | 65 | 64 | 36 | 33 |
| Type of RRT pre Tx | PD | HD | Pre-D | Pre-D |
| Cause of CKD | NAE | TIN | FSG | ND |
| 1st donor | Cadaveric | Cadaveric | Alive | Cadaveric |
| 2nd donor | Cadaveric | Cadaveric | Cadaveric | Cadaveric |
| Cause of graft failure | Vein T. | Vein T. | Arterial T. | Arterial T. |
| Time between transplants (h) | 336 | 62 | 15 | 44.5 |
| Time Cold ischemia 2nd graft (h) | 14 | 17 | 16 | 14 |
| Immunosuppression | TG, MFM, FK and P | TG, MFM, FK and P | TG, MFM, FK and P | TG, MFM, FK and P |
| Acute rejection | No | No | No | No |
| P Cr at discharge | 2.3mg/dl | 2.04mg/dl | 1.62mg/dl | 2.6mg/dl |
| P Cr at the end of follow-up (19months) | 1.15mg/dl (19 months) | 2.15mg/dl (15 months) | 1.43mg/dl (13 months) | 2.2mg/dl (12 months) |
P Cr: plasma creatinine; PD: peritoneal dialysis; CKD: chronic kidney disease; FSG: focal and segmental glomerulosclerosis; HD: hemodialysis; MFM: mycophenolate mofetil; NAE: nephroangiosclerosis; ND: diabetic nephropathy; TIN: tubulointerstitial nephritis; P: prednisone; Pre-D: predialysis; T: thrombosis; TG: thymoglobulin; RRT: renal replacement therapy; Tx: transplantation.
The immediate loss of the graft is included among the indications of transplantectomy and, in this case, it must be performed rapidly, since this almost immediate intervention can prevent foreseeable complications such as graft intolerance, rupture of the graft, infections and formation of antibodies ensuing hyperimmunization of the patient.6,9
Performance of express transplant has several advantages: it avoids the morbimortality of the transplantectomy as a necessary but isolated act, since in the same act another transplant is carried out, immunosuppression is maintained which prevents the formation of antibodies and the hyperimmunization of the patient and finally it avoids the negative psychological impact of graft loss and preserves the confidence of patient on the actual medical care.
Prior to the procedure, it is important to rule out other causes of early graft loss, such as hyperacute rejection,10 or problems with hypercoagulability9 since both situations would contraindicate express transplantation. In our cases, the immunological study carried out after graft loss, the histological absence of acute rejection and the lack of history of thrombotic events in the recipients, reasonably ruled out these causes.
This type of transplantation requires a potent immunosuppression together with strict immunological study of the donor and recipient to reduce compatibility requirements given the time constraint to perform the transplant within the immediate postoperative period. The immunological study should include the detection of specific donor antibodies that could have been generated with the first transplantation and its characterization, since the presence of an infarcted graft stimulates the production of these antibodies.10
All our recipients of express transplant received immunosuppression with thymoglobulin. Phelan et al.9 have reported a series cases with similar characteristics as ours, there were 9 cases collected over a period of 20 years. These patients had early graft loss due to vascular complications and were re-implanted in the subsequent days. Our series include cases in which transplantation was completed in a much shorter period of time, which provides more homogeneity than the Phelan series. In Phelan series the transplantectomy was not performed in the same surgical procedure as the re-transplantation, which undermines the effectiveness of the strategy. In addition, the aforementioned series differs from ours in that the immunosuppression used in the second transplant only included induction with antibodies in 2 out of the 9 cases. This resulted in an acute rejection of 30% in the total serie and in almost half (42.8%) of the patients without induction; thus the cause of graft loss. This experience reaffirms the strategy of administration a powerful immunosuppression to our patients, with a 0% rate of acute rejection and graft loss due to this cause.
The strategy of express transplantation depends on the availability of renal grafts in sufficient quantity and frequency in order to perform the re-transplantation within the immediate postoperative period. These conditions are fulfilled in our environment.11
Our experience has been positive and lead us to the individualized but systematic evaluation of all recipients with early graft failure secondary to vascular complications as potential candidates to undergo express transplantation
Please cite this article as: Franco A, Rodriguez Santarelli D, Sanz J, Muñoz C, Garcia Tabar P, Pérez Contreras J. Trasplante exprés: un tratamiento audaz en el fallo técnico precoz del injerto. Nefrologia. 2017;37:655–657.