Introducción: La fibrosis retroperitoneal idiopática es una entidad clínica de presentación poco frecuente, que suele cursar con uropatía obstructiva por atrapamiento ureteral por el tejido fibroso e inflamatorio crónico, constituido por miofibroblastos de disposición perivascular. En los últimos años, el pronóstico parece haber mejorado con el tratamiento médico inmunosupresor y con las intervenciones urológicas de liberación de los uréteres. Hemos revisado los pacientes diagnosticados de fibrosis retroperitoneal idiopática en nuestro centro con el objetivo de revisar el motivo de presentación clínica, de afectación renal y extrarrenal, el tratamiento realizado y la evolución clínica seguida. Han sido nueve enfermos no neoplásicos, no tratados previamente con radioterapia y sin administración previa de gadolinio en presencia de insuficiencia renal avanzada. Seis de ellos tienen diagnóstico histológico y tres radiológico. Han sido tratados con prednisona, 1 mg/kg/día durante tres meses, y la posibilidad de colocación de catéteres endoluminales doble J. El 89% de estos pacientes ha seguido una buena evolución sin insuficiencia renal crónica progresiva. Las recidivas han sido frecuentes a lo largo de su seguimiento.
Idiopathic retroperitoneal fibrosis is a rare disease often causing obstructive uropathy because the fibrosis entraps the ureters. The retroperitoneal tissue is constituted by a fibrous component and a chronic inflammatory infiltrate with the former characterized by miofibroblasts. The infiltrate displayed perivascular. Last years, the immunosuppressive therapy and the decompression of obstructive renal failure have improved the prognostic. We reported 9 patients with Idiopathic retroperitoneal fibrosis in a Centre. We evaluate clinical symptoms at the presentation with the signs of renal and non-renal involvement. We evaluate the achieved therapy and the follow-up. All 9 patients had a radiological and/or histological diagnosis in the absence of malignancy, previous radiotherapy or gadolinium’s administration with severe renal failure. The patients were treated with 1 mg/kg/day of prednisone three months and possibly the insertion of ureteral catheters. 89% patients have a high rate of initial success without renal failure, despite frequent disease relapse. A patient developed progression of the fibrosis.
INTRODUCTION
Idiopathic retroperitoneal fibrosis (IRF) is an uncommon condition that usually presents obstructive uropathy. The fibrous tissue of IRF consists of an inflammatory infiltrate characterised by perivascular myofibroblasts that contain lymphocytes, macrophages, plasma cells and eosinophils.1,2 The ureter is often trapped in this fibrous tissue and this causes obstructive uropathy and consequently, chronic ascending pyelonephritis.3 The prognosis of this disease seems to have improved in the last decade as different treatments have been tested and urinary bypasses have been carried out.
We have retrospectively reviewed the cases of nine patients diagnosed with IRF in one centre, after excluding patients with retroperitoneal fibrosis associated with neoplasia, radiotherapy or previous administration of gandolinium derivatives when advanced kidney disease was present. We reviewed the symptoms that led to diagnosis, the treatment administered and the progress of the condition.
MATERIAL AND METHOD
We retrospectively reviewed cases of patients diagnosed with IRF during the last 16 years in Parc Taulí Health Corporation in Sabadell, which covers a health care area with 400,000 people. These patients were monitored until 31 December 2008. The objectives of this study were: 1) to review the clinical manifestations of IRF that lead to its diagnosis, as well as the age and sex of patients; 2) the effect on the kidneys if any; 3) extrarenal complications if any; 4) drug treatments administered and urological procedures carried out if applicable; 5) clinical progress: follow up time and complications.
All patients with a history of neoplasia or radiotherapy were excluded. Drug treatment prior to diagnosis has been taken into consideration, especially the use of ergotics, betablockers and gandolinium. A history of aortic aneurisms and retroperitoneal surgery was also taken into account.
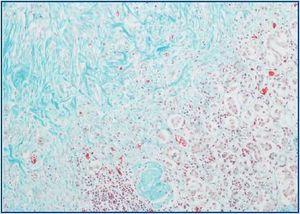
The diagnostic criteria were based on the histology: the biopsied tissue had to present fibrosis with inflammatory infiltrate containing lymphoplasmacytic cells and macrophages; it should be predominantly perivascular and contain irregular bands of collagen (figure 1). In the case of a radiological diagnosis, a fibrotic band around the aorta or iliac vessels would confirm IRF. In both cases, patients with infectious diseases (especially tuberculosis in this context), neoplasia(especially lymphoproliferative syndromes), sarcoidosis and autoimmune diseases were ruled out in accordance with the clinical and analytical criteria.
Kidney function was measured at the time of diagnosis and during the final check-up with the study deadline being 31 December 2008. Therefore, plasma creatinine was measured in mg/dl at both times. The existence of obstructive uropathy was determined using ultrasound or an abdominal scanner.
At the time of diagnosis, any non-nephrourological damage to theabdomen was established, paying particular attention to the possibility of vascular (aorta or iliac) and digestive (bile duct and alimentary canal) problems, using ultrasound or abdominal scanner, as well as the relevant tests associated with the symptoms present.
The progress of the condition was evaluated during weekly check-ups which included GSV testing, a haemogram, kidney function testing (creatinine and glomerular filtration) and liver function testing (GOT, GPT, gamma GT, alkaline phosphatase), cholesterol, triglycerides, total proteins and PCR, and the following was tested in urine: proteinuria and sediment. Even though there was no deterioration in kidney function, abdominal check-ups using a scanner were carried out annually.
There was a particular focus on the possibility of complications occurring, especially vascular complications (arterial ischemia or vein thrombosis in the lower limbs), urological complications (the emergence or worsening of hydronephrosis if already present, urinary infections, hydrocele, varicocele) and digestive complications (hepatobiliar or pancreatic damage).
RESULTS
From 1 October 1991 to 31 December 2008 nine patients were diagnosed with IRF in our centre. In six cases the diagnosis was made on the basis of the histology and in three cases it was diagnosed radiologically using a scanner and MR. In all cases, especially in the three cases diagnosed radiologically, other possible diagnoses of secondary IRF were ruled out. Table 1 shows that the cases reviewed involved eight men and one woman with an average age of 47.7 (28-60) at the time of diagnosis. One patient diagnosed in 1982 who suffered a subsequent relapse in 1995 and one case with a history of an aortobifemoral graft were included.
All patients with a history of neoplasia or concomitant conditions were excluded.
The most common symptom was abdominal or lumbar pain, which was the reason for seeking medical advice in 67% of cases. At the time of diagnosis, 33% of patients presented kidney failure, 33% were experiencing unilateral obstructive kidney damage and 44% were experiencing bilateral obstructive kidney damage; there was no initial kidney affectation in 22% of cases. A third of male patients (33%) initially presented unilateral or bilateral hydrocele, and 22% presented deep vein thrombosis in the legs.
One mg/kg/day of Prednisone was administered for three months, with this amount being reduced later on in eight of the nine cases. Double-J catheters were inserted in the ureters of the seven patients that presented hydronephrosis; a nephrostomy was initially carried out on one of them.
The average follow-up time for patients was 89.4 months (26-156). Two patients did not experience recurring symptoms, although the fibrotic band was still present (smaller) in the radiological exams using an abdominal scanner throughout the follow up period, which lasted 40 and 156 months respectively for these patients. The three patients diagnosed radiologically were monitored for 69, 110 and 156 months respectively. The patient with a history of vascular surgery was monitored for 110 months.
A third patient, who was the only one not treated with prednisone and who had a history of vascular surgery, did not experience recurring symptoms although the periaortic band was still present in the radiological exam.
Five patients treated with prednisone have become dependent on corticoids since they regularly relapsed. One patient began haemodialysis 48 months after he was diagnosed with IRF and presented frequent outbreaks and relapses. He died 10 years later on dialysis because of cardiovascular complications. A kidney transplant was never performed since the possibility of a bypass graft was rejected. There were no other complications associated with the IRF while the patient was in dialysis. In total, 62.5% of patients were dependent on corticoids.
With the exception of the patient with the poor prognosis who started haemodialysis, the other eight patients presented complications shown in table 2. One patient who presented peribiliary fibrosis also presented choledocholithiasis as a complication during the follow up period. Another patient also presented sclerosing cholangitis lesions and bridging hepatic fibrosis in the liver biopsy carried out because of dissociated cholestasis, however cirrhosis was not confirmed. Six years before being diagnosed with IRF, this patient also presented an episode of acute pancreatitis and cutaneous panniculitis, and for that reason a differential diagnosis including vasculitis and sarcoidosis was insisted upon.
The two patients with right renal atrophy already presented atrophy at the time of diagnosis. One of them presented contralateral hydronephrosis and for that reason the left ureter was catheterized. The other patient was unaffected. Two patients presented iliac artery obstruction, and one of them significant arteriosclerosis. One patient presented femoropopliteal vein thrombosis during the follow up period. In addition to this, one patient presented obesity, Cushing’s syndrome and obstructive sleep apnoea in response to prednisone rather than as a result of IRF.
DISCUSSION
The term “retroperitoneal fibrosis” is used to describe different physiopathological conditions that all generate fibrosis in the retroperitoneal space. They cause obstructive kidney failure by affecting the ureter unilaterally or bilaterally. This can potentially be reversed as long as all other obstructive uropathies are taken into consideration in the differential diagnosis.
The anatomopathological substratum of the illness is the chronic, non-specific inflammatory process, with an abundance of macrophages2 and perivascular distribution, which in general is periaortic.1
In most cases, retroperitoneal fibrosis is idiopathic, however 30% of cases are associated with other factors such as drugs (ergotics and betablockers are most commonly cited), neoplasia, aortic aneurisms, collagenopathies and vasculitis.4-8 Eight out of nine patients in our study presented idiopathic etroperitoneal fibrosis. One patient underwent aortoiliac surgery three years before, however this was considered an unlikely cause of retroperitoneal fibrosis and the case was recorded as idiopathic.
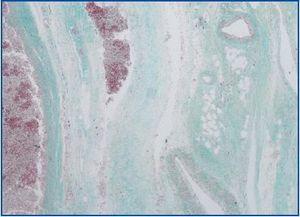
Fifteen percent of patients also presented extra-retroperitoneal fibrosis9 (figure 2). Thus, all the organs in the abdominal cavity can be enveloped by fibrosis (sclerosing cholangitis, pancreas and pelvic organs are most commonly described). Cases of mediastinal fibrosis, Riedel thyroiditis, orbital pseudotumours nd fibrosis of the maxillary sinus have also been described outside the abdomen; all are examples of multifocal fibrosclerosis syndromes.10-12
The case of the patient who was administered gandolinium, which caused systemic fibrosis and symptoms that have been described in recent years as those of nephrogenic systemic fibrosis, was excluded.13-15
Six of our cases were diagnosed on the basis of the histology and three radiologically, and all patients presenting neoplasia (lymphoma, sarcoma) and infections (tuberculosis) were excluded. We excluded patients with concomitant neoplasia (transitional cell carcinoma of the urinary tract was the most common) and those undergoing radiotherapy. The abdominal scan, in particular the MR scan, are the techniques of choice used to confirm a diagnosis of IRF.3,16
The age of onset and sex of IRF patients (mostly male) coincidewith other studies3,16: The average age was 47.7 years in our study compared with 56 years in others, and the percentage of males affected was 89% in our study compared with 86% and 63% respectively in others.3,16
Abdominal or lumbar pain was the most common symptom (67%). This also coincides with the findings of other authors. In general, pain was accompanied by other non-specific symptoms like weakness, loss of appetite, weight loss and fever. With these symptoms and the imaging findings, a differential diagnosis is made that includes other processes like lymphoproliferative syndromes, sarcomas, sarcoidosis and vasculitis. Therefore, the histological diagnosis is often indispensable. In this study, the last four patients described were effectively diagnosed using an MR-guided biopsy. This could be the method of choice in the future. Corradi et al.3 obtained histological samples from laparotomies or laparoscopies, taking advantage of ureterolysis in 24 patients. Van Bommel et al., who also included 24 patients in their study, only carried out biopsies on two of them, since the diagnosis in most cases was made radiologically.16 Moroni et al. confirmed the diagnosis histologically in 8 of their 17 patients by using biopsies obtained from laparotomies and, in one case, from a laparoscopy.17
The percentage of patients who presented obstructive uropathy was 77.8%. Initially, 33% of males also presented hydrocele.
After kidney complications, vascular complications were the most common finding at the time of diagnosis (22%) and throughout the follow up period (33%). Artery complications caused by extravascular fibrosis was slightly more common than vein complications.
One patient presented sclerosing cholangitis at the time of diagnosis and another presented it during the follow up (22% in total). The latter patient required a special differential diagnosis which included vasculitis, sarcoidosis and the aftereffects of pancreatitis because he had suffered from acute pancreatitis and panicullitis six years earlier.
Other studies describe vascular, artery or vein complications as being more common,17 although they refer to radiological (65% of cases) not clinical effects like the ones described in our study (44%), which takes into account the findings both at the time of diagnosis and during the follow-up. In most of the cases in this study, the fibrotic band surrounded the large abdominal vessels, the aorta or the inferior vena cava. Corradi et al.3 described how 17% of cases presented vascular complications. In the study by Van Bommel et al.16 25% initially presented vascular complications, however only 8.3% of cases presented any clinical damage. In these studies, the effects on the bile ducts, gallbladder, liver and pancreas have not been described.
The treatment administered in this centre was prednisone and ureterolysis in cases of ureteral compression.17 These studies are retrospective like ours and include a population that is too small to draw significant conclusions, however, it seems that immunosuppression and urological procedures are the treatment of choice. Immunosuppression involves corticotherapy, although in some cases it is administered along with azathioprine, cyclophosphamide or tamoxifen,17,18 despite the fact that there is no evidence to suggest that these immunosuppressants improve patient prognosis during follow up. Marcolongo et al.,18 in a series of 26 patients, obtained good results administering prednisone and azathioprine. In the future, treatments that inhibit the proliferation of fibroblasts or their apoptosis, like interferon, may be preferable.
The average follow up time for our patients of 89.4 months was significant even though the duration of the study was short. This made it possible to recommend conservative treatment for patients by administering prednisone and carrying out urological procedures using double-J catheters, which were generally inserted at the site of previous nephrostomies or via an ascending route. This long follow up period also rules out the possibility of retroperitoneal fibrosis which is often secondary to lymphoproliferative processes and low grade lymphomas. Oshiro et al.19 in particular insist on this possibility.
We can conclude that IRF is an uncommon clinical condition that mainly affects males of around 50 years of age. This condition can be diagnosed histologically through biopsies and monitored using abdominal imaging techniques. Because of its pathogenic nature, the treatment of this condition currently involves administering corticotherapy. Urological procedures should be undertaken with care and should be as non-invasive as possible, like double-J catheters. Relapses are common and should be treated once again with prednisone and possibly endoureteral catheterization. The current prognosis using these measures is satisfactory.
Figure 1.
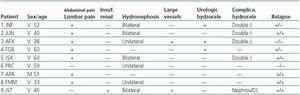
Table 1. Characteristics of patients at the time of diagnosis of idiopathic retroperitoneal fibrosis
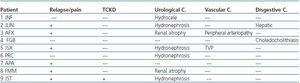
Table 2. Progress of patients diagnosed with idiopathic retroperitoneal fibrosis
Figure 2.