Metabolic syndrome is defined as the presence of three of the following five criteria: 1) waist circumference ≥102 cm (males) and ≥88 cm (females); 2) hypertriglyceridaemia (≥150 mg/dl); 3) HDL cholesterol <40 mg/dl (males) and <50 mg/dl (females); 4) blood pressure ≥130/85 mmHg or being on antihypertensives; and 5) fasting blood glucose ≥110 mg/dl or being on hypoglycaemic agents.1,2 A large number of studies link hyperuricaemia with metabolic syndrome, specifically with arterial hypertension and insulin resistance.3–6
Uric acid is the end product of purine degradation. It is eliminated by the kidneys, a process that involves reabsorption in the first segments of the proximal convoluted tubule (presecretory reabsorption), posterior tubular secretion and a second reabsorption in the final segments of the proximal convoluted tubule (postsecretory reabsorption). The result is a 10% of the filtered uric acid is excreted in the urine.1
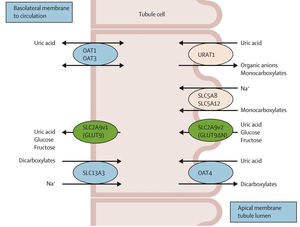
Several transporters involved in the renal management of uric acid have been identified thanks to the advances in molecular biology in recent years (Fig. 1). One of these is URAT1, encoded by the SLC22A12 gene and located in the apical membrane of proximal convoluted tubule cells that urate in exchange for a secreted anion. A Na+-monocarboxylate cotransporter (encoded by the SLC5A8 gene) acts synergistically, reabsorbing both anions and sodium at the same time. The hyperinsulinaemia which characterises the patient with metabolic syndrome increases sodium reabsorption through the above cotransporter, and this also increases urate reabsorption by promoting URAT1 activity and anion exchange with the filtered urate; this explains the association between hyperuricaemia, insulin resistance and hypertension. The reabsorption of urate into the peritubular space is carried out by another transporter, GLUT9, located in the basolateral membrane and also responsible of hexose transport. It also has an apical isoform (GLUT9S) along with URAT1, so urate reabsorption through this transporter happens twice. The hyperinsulinaemia, a characteristic of metabolic syndrome, promotes the activity of GLUT9, increasing the reabsorption of uric acid and glucose.1,4–6
Renal tubular transport of uric acid. The URAT1 transporter, located on the apical membrane of the proximal convoluted tubule, reabsorbs filtered urate in exchange for anions transported into the tubular lumen. The Na+-monocarboxylate transporter then reabsorbs these anions along with sodium. Lastly, GLUT9, located both apically and basolaterally, reabsorbs urate along with glucose and fructose.
From Esparza Martin and García Nieto,1 Perez-Ruiz et al.,4 Durá Travé et al.5 and López-Jiménez et al.6
With the increasing incidence of metabolic syndrome in recent years and its implication as a cardiovascular risk factor, clinicians have begun to focus more on the diagnosis of hyperuricaemia and its treatment. Although hypouricaemia (urate <2 mg/dl) is a rare finding in the population (0.2%), we have to be aware that it may occur and it is the expression of abnormality in the renal tubular transport of uric acid. The differential diagnosis (Table 1) is made based on fractional excretion of urate (FEUa), distinguishing between hypouricaemia with low FEUa (xanthinuria, liver disease, drugs) and high FEUa (hereditary renal tubular hypouricaemia and Fanconi syndrome for example).1
Differential diagnosis of hypouricaemia according to the FEUa.
| Reduced FEUa | Elevated FEUa (>10%) |
|---|---|
| Drugs: allopurinol, rasburicase | Primary/secondary Fanconi syndrome. Drugs: salicylates, losartan, oestrogens, dicoumarol, trimethoprim-sulfamethoxazole |
| Cancers | Intravenous contrasts |
| Impaired liver function | Total parenteral nutrition |
| Xanthinuria (xanthine oxidase deficiency) | Hodgkin’s lymphoma/other cancers |
| Wilson’s disease/hyperbilirubinaemia/cirrhosis | |
| SIADH/thiazide-related hyponatraemia | |
| Diabetes mellitus | |
| Hyperparathyroidism |
FEUa: fractional excretion of uric acid; SIADH: syndrome of inappropriate antidiuretic hormone secretion.
We present below a case report of a patient with metabolic syndrome in whom we should expect to have hyperuricaemia, but we underline the importance of the analytical finding of hypouricaemia to establish the differential diagnosis of associated tubular disease.
He was a 51-year-old male with hypertension on two drugs, type 2 diabetes on insulin, dyslipidaemia and obesity. He had been under follow-up since 2004 for proteinuria probably related to hyperfiltration due to obesity. Kidney function was normal.
His uric acid levels had been around 1.1 mg/dl since his first visit. As this analytical finding is unexpected in a patient with his previous history, a targeted medical history was obtained, orientating towards the differential diagnosis of hypouricaemia.
The patient had six siblings: three had hypouricaemia; one on haemodialysis due to obstructive CKD (renal lithiasis). Four cousins also had low urate, two of them with CKD in pre-dialysis and one on haemodialysis.
The patient reported previous episodes of renal colic. In 2011, he had haematuria and analysis showed urate crystals.
A 24-h urine showed high uricosuria, 1604.1 mg/day (normal values: 275–750). Fractional excretion of urate was elevated, 52% (>10%, which would indicate hypouricaemia of renal tubule origin). Calcium, phosphate, oxalate and citrate were normal in 24-h urine. No glycosuria. Abdominal ultrasound showed normal-sized kidneys. Lithiasis 3–4 mm in the right kidney and 7 mm in the left kidney, with no dilation of the urinary tract.
After ruling out other causes of hypouricaemia with elevated fractional excretion of uric acid, and in view of the family history of hypouricaemia, a genetic study was requested, finding a mutation in the SLC22A12 gene, which encodes the URAT1 transporter, and so confirming the diagnosis of hereditary renal tubular hypouricaemia.
In summary, the association of metabolic syndrome and hyperuricaemia has been well known for many years, even before the appearance of renal tubule uric acid transporters.1,4–6 However, hypouricaemia, often being a fortuitous laboratory finding, often goes unnoticed. We wish to highlight the importance of the differential diagnosis, in view of its possible association with hereditary tubular disease and the inherent clinical repercussions (for example, renal lithiasis and obstructive end-stage CKD).
Conflicts of interestDr Ana Noelia Hernández González declares that she has no conflicts of interest.