Acute kidney injury (AKI) in association with rhabdomyolysis is quite common. Depending on the patient’s comorbidity, an association of up to 30% has been reported between cases of rhabdomyolysis and AKI.1,2 We distinguish between traumatic and non-traumatic causes of rhabdomyolysis and it is notable that an increasing percentage of cases are now due to non-traumatic causes associated with commonly used drugs. In addition, associated risk factors have been described, such as advanced age, chronic kidney disease, diabetes, hypothyroidism, inflammatory or metabolic myopathies and trauma. In a population that is becoming progressively older and with polypharmacy, there is an ever-greater risk of drug interactions. We report a representative case.
This was an 89-year-old male, former smoker with hypertension, moderate aortic stenosis, hypothyroidism, dyslipidaemia, stage G3bA1 chronic kidney disease (basal creatinine: 1.9 mg/dl; glomerular filtration rate [GFR] CKD-EPI: 32ml/min/1.73m2) and sleep apnoea, who was admitted to hospital with severe rhabdomyolysis. He had suffered a lacunar stroke 10 years earlier with residual ataxia-hemiparesia and had grade iv bladder cancer in situ, treated by transurethral resection (TUR). Twelve years before he had been diagnosed with grade iv prostate adenocarcinoma, treated by radiotherapy combined with hormone therapy. Five years earlier he had received a second treatment with radiotherapy and twice-yearly triptorelin, due to biochemical progression with the development of bone metastases.
One year earlier, he had suffered an episode of severe rhabdomyolysis (creatine phosphokinase [CPK] 13,000IU/l), secondary to an accidental fall with trauma, which was accompanied by non-oliguric AKI stage 3 and a good response to conservative treatment. At that time, he was being treated with levothyroxine, candesartan, hydrochlorothiazide, acetylsalicylic acid, rosuvastatin, triptorelin and omeprazole. One month earlier, due to the progression of the prostate disease (pulmonary nodules, retrocrural and retroperitoneal lymphadenopathy), a new line of treatment was started with oral abiraterone 1000mg/24h and prednisone. In addition to the treatment described, he was taking the following drugs: calcifediol, calcium carbonate, bisoprolol, cetirizine and denosumab.
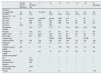
A year later, he was admitted to hospital after an accidental fall with a low-back contusion. The patient was also found to have AKI and severe rhabdomyolysis (Table 1). Obstructive uropathy was ruled out by renal ultrasound. Support treatment was started, with little response and progressive development of congestive heart failure, requiring acute haemodialysis and ultrafiltration from day three of admission. His CPK returned to normal on day ten after admission. Despite clinical recovery, the patient remains dependent on haemodialysis.
Changes over time in laboratory parameters.
| 23 days prior to admission | On admission day | + 1 | + 3 | + 8 | + 11 | + 14 | + 16 | At discharge | |
|---|---|---|---|---|---|---|---|---|---|
| Analyses | |||||||||
| Cr (mg/dl)/CKD-EPI GFR (ml/min/1.73m2) | 1.9 (29) | 9.5 (4.0) | 10.3 (4.0) | 9.8 (4.0) | 7 (6.0) | 5.3 (9.0) | 4.6 (10.0) | 4.3 (12) | 4.6 (17) |
| CPK (IU/l) | 32 | 91,012 | >100,000 | 28,193 | 4530 | 415 | – | 96 | – |
| AST (U/l) | 592 | 550 | 422 | 229 | 81 | 48 | 35 | 18 | |
| ALT (U/l) | 12 | 189 | 179 | 190 | 230 | 145 | 86 | 58 | 24 |
| LDH (U/l) | 198 | – | 1115 | 873 | |||||
| Bicarbonate (mmol/l) | – | 15.8 | 17.3 | 17.3 | 27 | 21.6 | 22.6 | 23.2 | 22.9 |
| Hb (g/dl) | 11 | 10.2 | 9.3 | 9.1 | 8.9 | 8.4 | 10.1 | 9 | 9.6 |
| WBC (10³/μl) | 7.5 | 11.9 | 8.24 | 9.21 | 10.2 | 8.3 | 8.8 | 8.3 | 9.9 |
| CRP (mg/l) | – | 67.7 | 83.7 | 196 | 112 | 85 | 71 | 72 | 17 |
| D-dimer (μg/l) | – | – | – | 25,600 | 9320 | 22,060 | – | 20,450 | – |
| Sodium (mmol/l) | 139 | 123 | 126 | 132 | 139 | 139 | 137 | 140 | 142 |
| Potassium (mmol/l) | 4.4 | 5.1 | 4.9 | 4.3 | 4.6 | 3.6 | 3.2 | 3 | 3.4 |
| Corrected calcium (mg/dl) | 8.9 | – | 7.9 | 9 | 10.5 | 10.5 | 9.9 | 10.1 | 9.2 |
| Phosphorus (mg/dl) | 2.9 | – | 6.6 | 7.5 | 4.3 | 2.7 | 2.8 | 2.7 | 3.8 |
| Simple urine sample | |||||||||
| pH | 5.5 | – | – | – | – | – | – | – | |
| Density (g/l) | 1020 | – | – | – | – | – | – | – | |
| Red blood cells (cells/μl) | 200 | – | – | – | – | – | – | – | |
| Proteinuria by test strip (mg/dl) | >300 | – | – | – | – | – | – | – | |
| P/C (g) | 6.2 | 13 | – | – | – | 1.75 | |||
ALT: alanine aminotransferase; AST: aspartate aminotransferase; CPK: creatine phosphokinase; Cr: plasma creatinine; CRP: C-reactive protein; GFR: glomerular filtration rate; GFR CKD-EPI: glomerular filtration rate estimated by CKD-EPI; Hb: haemoglobin; LDH: lactate dehydrogenase; P/C: urine protein/creatine ratio; WBC: white blood cells.
Abiraterone is a CYP17A1 inhibitor approved by the Food and Drug Administration in 2011 for metastatic prostate cancer. It blocks the synthesis of androgens in the prostate, testicles and adrenal glands, causing an increase in the synthesis of ACTH and mineralocorticoids by inhibiting the enzyme 17α hydroxylase. This can induce hypokalaemia, diarrhoea, elevated blood pressure, oedema and impaired liver function. It does not interact directly with the metabolism of statins, but it does inhibit a transporter, hepatic organic anion transporting polypeptide 1B1 (OATP1B1), dependent on the SLCO1B1 gene, which is a substrate for rosuvastatin. This can reduce the uptake of abiraterone by the liver resulting an increase in its levels. In addition, we know that in certain polymorphic variants in which the transport activity is genetically reduced,3,4 it can induce an increase in the concentration of rosuvastatin, with the risk of toxicity and rhabdomyolysis. It is rapidly absorbed orally and is metabolised almost exclusively in the liver, being 99% bound to plasma proteins and reaching a maximum plasma concentration at two hours. Its metabolism in the liver uses two enzymatic pathways: cytochrome p450 (CYP) 3A4; and sulfotransferase (SULT) 2A1. It is excreted mainly through the faeces, with less than 5% being excreted through the urine.5 Marbury et al.5 studied the metabolism of abiraterone in severe renal failure and concluded that there are no clinically appreciable pharmacokinetic differences between patients with preserved renal function and renal failure.
A few cases have been described in the literature in which abiraterone was used in patients with advanced AKI and on haemodialysis. However, although anecdotal, this would support its safety.6,7
Three cases of rhabdomyolysis induced by abiraterone in combination with rosuvastatin have been published to date.1,2,8 In two of these cases, in addition to rosuvastatin, there was a third drug associated: denosumab. In our case, the patient scored seven points on the Horn Drug Interaction Probability Scale and six on the Naranjo Adverse Drug Reaction Probability Scale,9,10 which meets criteria for significant probability.
The patient began with severe rhabdomyolysis which induced AKI, requiring haemodialysis. It could be hypothesised that the abiraterone triggered liver failure leading to increased concentrations of rosuvastatin and abiraterone itself. In an older adult patient with hypothyroidism, previous renal failure, treatment with angiotensin-converting enzyme inhibitors and diuretics, dehydration, prolonged immobility due to his neurological sequelae, and polypharmacy (13 drugs), the chance of interactions is very high.11 This case illustrates the importance of close follow-up in patients with polypharmacy and high levels
FundingThe authors declare that they did not receive any type of funding for conducting the study.
Conflicts of interestThe authors have no conflicts of interest to declare.