Potassium, the primary intracellular cation, is essential in physiological processes such as cell membrane excitability, as well as solute and ion transport. Maintenance of potassium homeostasis is an essential physiological function. Under normal conditions, 90% of dietary potassium intake is absorbed in the small intestine, and an amount equivalent to that absorbed is excreted in the distal tubules of the kidney. The colon's contribution to potassium absorption and excretion is insignificant. The amount of potassium that is excreted in the faeces of a healthy person is close to 10mmol per day.1 Multiple studies, the oldest of which were published in the 1960s, demonstrate the importance of maintaining potassium homeostasis through the gastrointestinal tract in patients with end stage renal disease.2
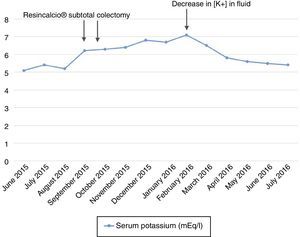
We present the case of a 74-year-old patient with end stage renal disease failure since 1999 likely secondary to a glomerular disease which was not biopsied with a decrease in kidney mass (right nephrectomy due to type I clear-cell papillary renal carcinoma in 2011), who started haemodialysis in November 2011. In 2014, the patient was diagnosed with attenuated familial adenomatous polyposis and underwent endoscopic resection of several polyps. Later on, in September 2015, a subtotal colectomy was performed, due to his high risk of developing colorectal cancer. A resection of the ileum up to the sigmoid colon–rectum and a termino-terminal anastomosis were performed without complications. The patient was discharged a week after surgery. Two weeks after discharge, the patient showed a gradual increase in plasma potassium, with a peak level of 7.1mEq/l in February 2016 (Fig. 1). A review of the patient's prior venous blood gases revealed that he had never had metabolic acidosis, that could potentially explain his hyperkalaemia. Moreover, his dialysis suitability parameters were correct and had not changed in the last 6 months (online haemodiafiltration, with convective volumes of 28–30l/session, Kt/V of 1.6–1.8 and Kts of 56–61).
An interview of the patient about his diet confirmed that he followed a suitable low-potassium diet with an estimated potassium intake of around 30–40mEq/day. Particular emphasis was placed on an ongoing basis on the importance of maintaining a low-potassium diet. Even so, it was necessary to start treatment with calcium polystyrene sulphonate at a dose of one sachet (15g) per day, initially on alternating days, then every 24h. Despite these measures, the patient's potassium levels remained high. Consequently, the level of potassium in his dialysis fluid was also lowered (from 2 to 1mmol/l). After this, his potassium levels remained below 6mEq/l.
A progressive decline in or maintenance of kidney function is associated with an increase in capacity for potassium secretion in the colon. The mechanism through which colon secretion of potassium is increased in these patients is complex and depends on several factors. On one hand, there is an increase in Na+/K+–ATPase pump activity in the basolateral membrane of the intestinal cell. This leads to an increase in intracellular potassium levels as well as an increase in potassium conductivity in apical cells. Colon secretion of potassium is also increased by aldosterone. Although its mechanism has not yet been fully reported, it appears to be related to an increase in expression of large-conductance potassium channels (BK channels) in the apical membrane of the intestinal cell.3
Konowa et al. published a case4 in 2013 on a patient with end stage renal disease undergoing haemodialysis who underwent surgical resection of the ileocaecal junction and a temporary ileostomy. After this, the patient developed hyperkalaemia, which resolved following reanastomosis of the colon. Various in vitro and in vivo studies have used immunohistochemistry techniques to show that there is greater BK channel expression in patients with end stage renal disease than in those with normal kidney function, in whom small- or intermediate-conductance potassium channel expression predominates.
In summary, potassium secretion in the gastrointestinal tract is a complex and essential mechanism for maintaining its homeostasis in patients with terminal end stage renal disease. Our case demonstrated the importance of potassium secretion in the colon in patients with end stage renal disease.
Please cite this article as: Rodríguez P, Mérida E, Hernández E, Milla M, Praga M. Hiperpotasemia de causa no renal en paciente en hemodiálisis. Nefrologia. 2018;38:96–97.