A few months ago, we published a case report of asymptomatic severe hypocalcaemia following a dose of denosumab in a patient with advanced chronic kidney disease.1 We now report a new case, this time one that was life-threatening for the patient. We thought that it important to report this new case due to its severity and, to show that it does no longer seems to be so rare.
We present the case of a 62-year-old woman whose medical history included slight intellectual disability, diabetes mellitus, long-standing dyslipidaemia and hypertension; and colon neoplasm 3 years earlier. She had been diagnosed of chronic kidney disease likely related to nephroangiosclerosis secondary to hypertension, currently in stage 4. Her regular treatment consisted of olmesartan, repaglinide, insulin glargine, atorvastatin, escitalopram, bromazepam, quetiapine and pantoprazole. Six months earlier, she suffered a hip fracture following an accidental fall and underwent implantation of a total hip prosthesis. The Traumatologists started treatment with denosumab 60mg every 6 months and 1500mg of calcium carbonate with 1000IU of cholecalciferol daily to treat osteoporosis. After 10 days of administering denosumab, the patient visited the Emergency Department due to signs and symptoms of general malaise, as well as neck and leg muscle contracture. The testing performed revealed severe hypocalcaemia—5.2mg/dl. Following fluid and electrolyte replacement therapy, her laboratory parameters returned to normal and her signs and symptoms disappeared in 3 days. After a week, the patient visited the Emergency Department again due to new signs and symptoms of anorexia, watery diarrhoea, general malaise, muscle stiffness and hypotension. She had severe hypocalcaemia, hypomagnesaemia, metabolic acidosis and worsening of kidney function. She required admission to the Intensive Care Unit for intravenously managed fluid and electrolyte replacement therapy. She experienced clinical and laboratory improvement. When she was discharged from hospital, treatment was maintained with calcium carbonate, magnesium lactate and calcitriol (Table 1).
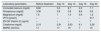
Laboratory data at baseline and over time.
| Laboratory parameters | Before treatment | Day 10 | Day 13 | Day 18 | Day 30 |
|---|---|---|---|---|---|
| Corrected calcium (mg/dl) | 8.62 | 5.2 | 8.7 | 4.5 | 7.1 |
| Phosphorus (mg/dl) | 3.36 | 3.9 | 3.8 | 8.8 | 2.6 |
| Magnesium (mg/dl) | 1.5 | 1 | 1.4 | 0.9 | 1.2 |
| iPTH (pmol/l) | – | – | – | – | 317 |
| 25-OH Vitamin D (ng/ml) | – | – | – | – | 7 |
| Creatinine (mg/dl) | 2.19 | 2.91 | 2.63 | 6.1 | 3.26 |
| MDRD (ml/min) | 17 | 17 | 19 | 7 | 15 |
The patient was a woman with osteoporosis. However, in addition, she had advanced chronic kidney disease. In such a situation, osteomineral metabolism abnormality has some distinct, more complex features, with abnormalities in both remodelling and mineralisation rate, with different combinations of these, leading to different patterns of osteomineral abnormality (fibrous osteitis, adynamic bone disease, osteomalacia).2,3 A few months ago, we published a similar case of severe hypocalcaemia, although that time it was asymptomatic. The use of a powerful antiresorptive agent such as denosumab1 interferes with these mechanisms. This may lead to hungry bone syndrome by inhibiting osteoclast activity and causing severe hypocalcaemia. We believe that the use of denosumab in patients with advanced chronic kidney disease requires from clinicians to weigh up the risk/benefit ratio and, should they need to administer it, perform a tight follow-up of their patients’ signs and symptoms as well as laboratory values.
Please cite this article as: Monge Rafael P, Martin de Francisco ÁL, Fernández-Fresnedo G. Denosumab y enfermedad renal crónica avanzada: hipocalcemia severa con riesgo vital. Nefrologia. 2018;38:97–98.
Denosumab is a human monoclonal antibody (IgG2) that binds with great affinity and specificity to RANKL and blocks activation of RANK, its receptor, on the surfaces of osteoclasts and their precursors. This reduces their activity and causes a decrease in bone resorption in trabecular and cortical bone. It is used to treat osteoporosis and administered every 6 months. It is not necessary to adjust the dose in renal failure, but there is an increased risk of hypocalcaemia.4,5