Contents
To the Editor,
Drug-induced lupus is a syndrome that shares clinical and analytical characteristics with idiopathic systemic lupus erythematosus and which appears after exposure to certain drugs that induce autoantibody formation.
In 1945, Hoffman described the first case of drug-induced lupus, which involved the antibiotic sulfadiazine as the agent responsible for the condition. Eight years later, in 1953, Morrow et al. published a new case relating to the use of hydralazine1. Since then, the list of associated drugs has continued to increase and in recent years, biological therapies, such as tumour necrosis factors (TNF) and interferons (IFN), have joined with classic agents, such as procainamide, the aforementioned hydralazine, isoniazid or minocylcine2,3,4.
The mechanism causing this condition has not been fully defined; immunogenetic (certain HLA alleles) and pharmacogenetic (slow acetylator phenotype) factors appear to play an important role in its aethiopathogeny1,5.
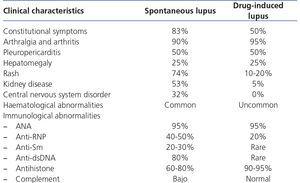
In terms of clinical presentation, the most common symptoms are fever, general malaise, muscle pain, joints pain, arthritis, rash and serositis. Unlike idiopathic lupus, kidney, haematologic and nervous system disorders are uncommon6. Antihistone antibodies are typical laboratory findings. Hypocomplementaemia and anti-double-stranded DNA, characteristics of idiopathic lupus, tend to be absent, although the latter can test positive in cases of anti-TNF- or IFN-induced lupus (Table 2).
The interval of time between starting the drug and the condition appearing is highly variable, being between 2 weeks and 7 years in the case of IFN-α; a case developing two months after the drug’s suspension has been described7.
This condition’s prognosis is favourable, such that discontinuation of the responsible drug is followed by recovery in the majority of cases, in a time frame that can stretch from weeks to months. Until then, non-steroidal anti-inflammatory drugs (NSAID), hydroxychloroquine and low-dose systemic corticosteroids can be used temporarily to control symptoms.
CASE
We present a 51-year-old male, with chronic kidney failure secondary to IgA glomerulonephritis, on a periodic haemodialysis programme, hypertensive, an ex-user of cocaine by inhalation and with chronic hepatitis C virus (HCV) disease, for which reason he was treated with ribavirin and pegylated IFN-α (180μg per week) for 49 weeks, obtaining a sustained viral response. Two weeks after finishing this treatment, he sought consultation due to asthenia and generalised joint pain of 10-15 days evolution, also experiencing in the last 48 hours 38 ºC fever and increased right hip pain. In the physical examination he presented pain on moving the aforementioned joint, with neither functional weakness nor inflammatory signs at this level nor in other joints. The increase of acute-phase reactants (C reactive protein was 9, ESR 120 and neutrophilia) stood out in the laboratory analysis. Blood cultures were taken (which were sterile) and, in order to rule out septic arthritis, an ultrasound of the joint was requested, which did not show signs of arthritis nor joint fluid on being drained and analysed. An echocardiogram ruled out endocarditis. In the study undertaken to rule out tumours/inflammation (bone scan, body gallium scan and chest/abdominal/pelvic CT scan), degenerative changes were only observed in the scapulohumeral, glenohumeral and coxofemoral joints, with no other significant findings. The autoimmunity test was positive for ANA (IIF) at titres of 1:80 and anti-chromatin (antihistone), with negative anti-dsDNA and normal complement levels. Other findings were rheumatoid factor 29 and positive cryoglobulins (but with only 0.33% cryocrit). It must be mentioned that one year before, prior to starting treatment with pegylated IFN, autoimmunity was negative and by contrast, cryoglobulins were positive with 4.4% cryocrit. Given these results suggesting drug-induced lupus (related to the pegylated IFN-α that the patient had been receiving until two weeks before due to his HCV), treatment with NSAID, low dose corticosteroids and hydroxychloroquine was started, with significant improvement of symptoms.
Lymphocyte populations were also counted before and during IFN-α therapy, showing significant lymphopenia, with a decrease of both T cells (CD4+ and CD8+) and B cells during treatment (Figure 1).
DISCUSSION
Drug-induced lupus is a condition without established diagnostic criteria. It should be considered in those patients who have received one of the implied drugs for longer than one month and who have compatible symptoms and autoimmunity test. The growing appearance of new pharmacological therapies, as well as the important pharmacosurveillance of their adverse effects, make the list of agents associated with this condition increasingly comprehensive. For this reason, high clinical suspicion is key, and therefore timing is of great importance.
For our patient, significant lymphocyte depletion induced by IFN-α should also be noted. Although T cell lymphopenia is an effect already described with the use of IFN-α due to thymus’ function alteration, this situation, together with the patient’s significant B lymphopenia, would mean a dysregulation of the immune response which could be involved in autoimmunity.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Medicines associated with drug-induced lupus (4)
Table 2. Characteristics of spontaneous and drug-induced lupus (6)
Figure 1. Evolution of lymphocyte populations following treatment with interferon alpha