Postural balance is the result of a complex interaction of sensory input which keeps us upright. Haemodialysis patients have alterations which can lead to postural instability and a risk of falls. Our objective was to analyse postural stability and its relationship with the risk of falls in haemodialysis patients using a force platform.
Material and methodsThis was a prospective cross-sectional study. Postural balance was recorded using a force platform in prevalent haemodialysis patients. We collected epidemiological, dialysis, analytical and treatment data. The incidence of falls was recorded over the six months following the tests. The postural stability analysis was performed with a portable strain gauge platform (AMTI AccuGait®) and a specific software unit for stabilometry (Balance Trainer® program). We measured 31 balance parameters; the balance variables used were: Area95; Area effect; VyMax; Xrange and Yrange. The stabilometry studies were performed in three situations: with eyes open (EO); with eyes closed (EC); and with the patient performing a simultaneous task (COG). We performed one study at the start of the dialysis session, and a second study at the end. Stabilometry was measured in a control group under similar conditions.
ResultsWe studied 32 patients with a mean age of 68 years old; of this group, 20 subjects were male and 12 were female. Their mean weight was 74 kg, with a mean BMI of 27.6 kg/m2. In the controls, there were no significant differences in the stabilometry between the three situations studied. Both pre- and post-haemodialysis, patients with closed eyes showed greater imbalance, and there were significant differences with the other situations and controls. We found a significant increase in instability after the haemodialysis session, and greater instability in the 13 patients with diabetes (p < 0.05). The four patients with hyponatraemia (Na <136 mmol/l) had worse balance in the COG situation (p = 0.038). Various drugs: insulin, p = 0.022; antiplatelet agents, p = 0.036; and beta-blockers, p = 0.029 were associated with imbalance. The ten patients who suffered falls had greater imbalance, Yrange, Xrange, Area95 and AreaEffect, both pre- and post-haemodialysis (p < 0.05) than those without falls.
ConclusionsHaemodialysis patients have alterations which can lead to postural instability and a risk of falls. Prevention programmes which include specific exercises to improve balance could be beneficial in reducing the risk of falls in this population.
El equilibrio postural es el resultado de una compleja interacción de aferencias sensoriales que nos mantiene erguidos. Los pacientes en hemodiálisis presentan alteraciones que pueden generar inestabilidad postural y riesgo de caídas.
El objetivo es analizar la estabilidad postural, mediante una plataforma de fuerzas, en pacientes hemodializados y su relación con el riesgo de caídas.
Material y MétodosSe realizó una estudio prospectivo transversal. El balanceo postural se registró mediante una plataforma de fuerzas en los pacientes prevalentes en hemodiálisis. Se recogen datos epidemiológicos, diálisis, analíticos y de tratamiento. La incidencia de caídas fue registrada durante los 6 meses siguientes a las pruebas.
El análisis de la estabilidad postural se realizó con una plataforma portátil de galgas extensiométricas (AMTI AccuGait®) y una unidad de software específico para estabilometría (programa Balance Trainer®). Se determinan 31 parámetros de equilibrio; las variables de equilibrio utilizadas son: Area95; Area effect; VyMax; Xrange y Yrange. Los estudios de estabilometría se realizan en tres situaciones: con ojos abiertos (OA), con los ojos cerrados (OC) y otro mientras el paciente realiza una tarea simultánea (COG). Se realiza un estudio al iniciar la sesión de diálisis y el segundo al terminar. La estabilometria en condiciones semejantes se mide en un grupo control.
ResultadosSe estudian 32 pacientes, edad media de 68 años; 20 hombres y 12 mujeres. Su peso medio es 74 kg y el IMC 27,6 Kg/m2. En los controles no hay diferencias significativas en la estabilometría entre las tres situaciones estudiadas. Los pacientes con los ojos cerrados, pre y postHD, presentan más desequilibrio, con diferencias significativas con el resto de situaciones y controles. Después de la sesión de HD se observa un aumento significativo de la inestabilidad. Se observa mayor inestabilidad en los 13 pacientes diabéticos, p < 0,05. Los 4 pacientes con hiponatremia, Na<136 mmol/L, presentaban peor equilibrio en la situación COG, p = 0,038. Varios fármacos: Insulina, p = 0,022; antiagregantes p = 0,036; y betabloqueantes p = 0,029 se relacionaban con el desequilibrio. Los 10 pacientes que sufrieron caídas presentaban mayor desequilibrio, Yrange, Xrange, Area95 y AreaEffect, pre y postHD, p < 0,05, que los que no tuvieron caídas.
ConclusionesLos pacientes en hemodiálisis presentan alteraciones que pueden generar inestabilidad postural y riesgo de caídas. Programas de prevención que incluyan ejercicios específicos para mejorar el equilibrio podrían ser beneficiosos reduciendo el riesgo de caídas en esta población.
Postural balance is the result of a complex interaction of sensory inputs which trigger a constant muscular response sufficient to keep us upright. The vestibular system, vision, joints, tendons, muscles, the peripheral nervous system and the cerebellum are all actively involved in this process.1–5 Diseases that affect these systems or organs, as well as functional changes associated with ageing, lead to balance disorders.6,7
Patients with chronic kidney disease (CKD) have alterations in blood pressure and homeostasis and an accumulation of harmful substances, such as uraemic toxins; they are also prescribed drugs that can affect their postural stability.8,9 Patients with advanced CKD need haemodialysis (HD) to replace kidney function, eliminate uraemic toxins and regulate the amount of fluids and minerals and the acid-base balance. HD is a necessary and effective treatment in these patients, but this situation involves risks that need to be controlled.
The dialysis process can lead to haemodynamic instability, which may be accompanied by episodes of hyper- or hypotension, alterations in homeostasis and/or abnormal levels of ions, such as sodium, potassium, calcium and magnesium, which can act on the different organs and tissues, and can affect the person's postural balance.8,10–14 Patients on HD are increasingly older, owing to which they have a greater degree of underlying postural instability related to the ageing process, affecting vision, proprioception, the locomotor system and nerve conduction, all of which are active parts of the aforementioned postural control.15,16 Added to this is the very high rate of polypharmacy among haemodialysis patients, recognised as a risk factor for falls owing to the postural disturbances it can provoke.17 Moreover, patients who have been on dialysis for several years can develop problems due to amyloid deposits affecting joints essential for postural control, such as the hip, knee and ankle.
Prevention of falls in HD patients is of paramount importance due to the significant consequences in terms of quality of life, associated morbidity and the reduction in life expectancy, without forgetting that the economic and healthcare load of problems deriving from falls is very high, especially in the elderly.18,19 Falls are associated with postural instability.
HD patients are therefore exposed to a number of different risk factors, which can lead to postural instability and risk of falls, and which need to be identified, diagnosed and corrected at an early stage.
Material and methodsWe designed an observational, cross-sectional, prospective study to measure postural stability using a pre-HD and post-HD force platform in prevalent patients with CKD treated in a hospital HD unit. We collected epidemiological, dialysis, analytical (pre-HD and post-HD) and treatment data. We also collected data on the incidence of falls six months after the tests, and the SF-36 quality of life test.
ObjectivesThe main aim of this study was to analyse postural stability in haemodialysis patients using a force platform, and determine the effect of the HD session on their postural stability.
Our secondary objectives were to:
- •
Analyse the postural stability of HD patients compared to a control group.
- •
Analyse postural stability before and after the HD session.
- •
Analyse dialysis parameters and the time the patient has been on HD as risk factors for postural stability.
- •
Analyse the possible association between the patient's laboratory values, such as natraemia, and postural stability.
- •
Analyse the effect of medications on postural stability.
- •
Analyse the predictive value of stabilometry with respect to the risk of falls.
- •
Analyse the possible relationship between balance disturbances and a poorer quality of life.
We included prevalent patients on HD from the Hospital Universitario Infanta Leonor HD Unit who voluntarily agreed to take part in the study.
Inclusion criteria: individuals aged over 18, with CKD on HD, who previously agreed with and signed an informed consent form explaining the format and purpose of this study.
Exclusion criteria: central neurological diseases, patients with vestibular or visual disorders without optical correction, deformations of the locomotor system and, in general, patients not able to stand up on their own. Patients on treatment with neuroleptics. Patients who did not give their informed consent.
Control group: balance was analysed in a control group without related disease and with a similar age and gender distribution to the patients with CKD.
Analysis of postural stabilityPostural stability analysis was performed with a portable strain gauge platform (AMTI AccuGait®, 44 × 500 × 500 mm, Advanced Mechanical Technology Inc., Watertown, MA, USA) and a specific software unit for stabilometry (Balance Trainer®; Advanced Mechanical Technology Inc., Watertown, MA, USA),20–24 following the same initial positioning protocol for all patients. Three stabilometry studies were completed for each patient and control: one with their eyes open (EO), another with their eyes closed (EC), and another while the patient performed a cognitive task (COG), consisting of counting backwards aloud from 100 to 0. The studies were all performed under similar lighting conditions.
Two studies of postural stability were performed on each patient. The first, before starting the dialysis session (pre-HD) and the second, at the end of the session (post-HD).
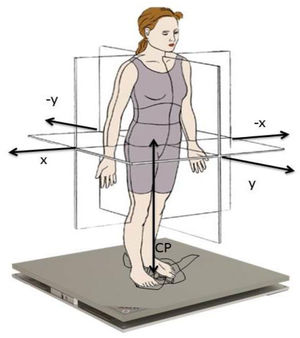
The platform and its analysis software had been previously used in other studies and were used as references to validate other postural stability analysis systems25 (Fig. 1).
The platform was placed 2−3 m from a wall on which a black dot had been marked 1.5 m from the floor to fix the gaze on during the stabilometry data collection tests. On the first day of putting in place, we checked for possible interference with other nearby instruments, and to make sure that the floor was even and that the platform was stable. The platform was plugged into the electricity supply one hour before beginning the tracings on the study population. To confirm that the platform was properly calibrated, a tracing was made without a patient to check for any vibration that could interfere with data collection during the assessments.
The protocol followed to obtain the stabilometric variables was the same for each subject. The participants climbed onto the platform and the points that defined the standard support base were marked with a washable marker. These points are at the level of the ball of the first toe, the first metatarsophalangeal joint, the internal area of the heel, the external area of the heel and the fifth metatarsophalangeal joint. The tracing with the Balance Trainer computer program® was then started. The points marked for each subject were pressed to trace their base of support. Next, calibration was carried out before each tracing; the patient climbed onto the platform placing their feet to line up with the marks and the tracing was started, selecting a frequency of 100 Hz/min.
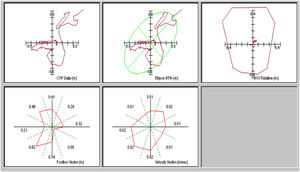
The stability limits were expressed as the measure of the displacements (cm) from the centre of pressure (CoP) in the medial-lateral (X) and anterior-posterior (Y) axes, the area of the ellipse generated by the displacements of the CoP, with 95% confidence, and the velocities of displacement of the CoP. The computer program provides 31 variables depending on the displacement of the CoP. The CoP is defined as the point where the ground reaction forces under the feet are applied (Fig. 2). The balance variables used in the study were: Area95, AreaEffect, VyMax, Xrange and Yrange.
Statistical analysisSample size: accepting an alpha risk of 0.05 and a beta risk of 0.2 in a bilateral contrast, 29 subjects are required, as based on previous studies,10,12 the initial proportion of events is 0.27 and at the end 0.73. We estimated a loss to follow-up rate of 0%.
The main variables were: (1) the mean displacement of the CoP in the sagittal and lateral planes; (2) the mean velocity of these movements; and (3) the area that included the displacement of the CoP with a 95% confidence interval. These are all continuous quantitative variables (Table 1). We used these variables and the measurements before and after the HD session to compare postural balance between the control group and the study patients.
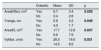
Comparison of balance parameters in the controls and the patients in the six situations in which they were measured.
| Area95, cm2 | AreaEffect, cm2 | Xrange, cm | Yrange, cm | VyMax, cm/s | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Measurement | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Patients, n = 32 | ||||||||||
| Pre-HD EO | 5.5434 | 3.86977 | 2.0241 | 1.34286 | 2.9388 | 1.03261 | 2.6312 | 1.12775 | 9.3641 | 5.53780 |
| Pre-HD EC | 8.6622 | 5.77865 | 3.1500 | 1.88413 | 3.6275 | 1.33657 | 3.9469 | 1.38059 | 14.9891 | 10.27166 |
| Pre-HD COG | 5.8556 | 5.85274 | 2.1031 | 2.01979 | 3.0163 | 1.43804 | 2.8569 | 1.33036 | 11.5131 | 7.60620 |
| Post-HD EO | 6.9031 | 5.02202 | 2.4766 | 1.71101 | 3.3603 | 1.31494 | 3.2588 | 1.38465 | 11.1106 | 8.07977 |
| Post-HD EC | 13.2506 | 10.81846 | 4.9013 | 4.10468 | 4.3381 | 1.86953 | 4.7544 | 2.59090 | 19.4284 | 14.58531 |
| Post-HD COG | 6.2716 | 5.51139 | 2.2003 | 1.89761 | 3.3444 | 1.40023 | 2.9591 | 1.19762 | 12.0763 | 7.29004 |
| Controls, n = 9 | ||||||||||
| EO | 4.36889 | 1.341580 | 1.59000 | 0.400156 | 2.4811 | 0.46590 | 2.3311 | 0.48748 | 13.99444 | 13.076864 |
| EC | 6.16111 | 2.405439 | 2.14889 | 0.802612 | 3.3311 | 0.50780 | 2.9433 | 0.64788 | 12.21222 | 5.522490 |
| COG | 4.35333 | 1.353505 | 1.57778 | 0.496809 | 2.4189 | 0.53757 | 2.7867 | 0.72030 | 14.54667 | 8.731284 |
| Among controlsa | NS | NS | NS | NS | NS | |||||
| Patients/controlsb | p >0.05 | p >0.05 | NS | p >0.05 | NS | |||||
COG: cognitive task; EC: eyes closed; EO: eyes open; NS: not significant; post-HD: after haemodialysis; pre-HD: prior to haemodialysis; SD: standard deviation.
Pair-wise multiple comparison between the main balance variables.
In bold: measurements with closed eyes, both before haemodialysis2 and after5, were significantly higher among the patients. Measurements with eyes closed were significantly higher after haemodialysis than before.
Sample study: once the database was built, it was debugged. The Kolmogorov-Smirnov test was used to determine whether or not the continuous variables followed a normal distribution. The results were expressed as the mean ± the standard deviation.
The comparison of means between the control group and the patient group was carried out using the Student's t test for the normal quantitative independent variables. Categorical variables were expressed as percentages and compared using the χ2 test.
The different consecutive measurements in each patient were compared using a paired t test or Dunnett's test, as appropriate.
Values of p < 0.05 were considered significant.
Statistical analysis was performed with the SPSS® 15.0 package (SPSS Inc., Chicago, IL, USA).
This study was approved by the Ethics Committee (Hospital Universitario Infanta Leonor-Hospital General Universitario Gregorio Marañón) with the title "Balance disturbances in patients with chronic kidney disease on haemodialysis (HD)", with protocol code: Hospital Universitario Infanta Leonor-18/001, protocol version 4.5 and version date 15 February 2018.
ResultsThe study was completed by 32 patients with a mean age of 68 years (13) [35–87]; 20 male and 12 female. Their mean weight was 74 (17) [51–130] kg, height 164 (7.8) cm and BMI 27.6 (5.3) [19.3–43.4] kg/m2.
Thirteen (40.6%) had diabetes and 25 (78.1%) hypertension, 15 (46.9%) had a history of heart failure, 15 (46.9%) of dyslipidaemia, 4 (12.5%) of severe secondary hyperparathyroidism and 2 (6.3%) hypothyroidism. The mean time on renal replacement therapy was 9.3 (8.9) 1–17 years.
In the dialysis process on which the study was carried out, a Kt L of 58.0 (5.23) [50.9–68.00], Kt/V 1.87 (0.38) [1.22−3.01] and a total UF of 2,477.4 (943.3) [1,000–5,000] were obtained.
In terms of prescribed drugs, there were 20 patients (62.5%) on statins, 14 (43.8%) on antiplatelet drugs, 5 (15.6%) on dicoumarinics, 7 (21.9%) on OAD, 7 (21.9%) on insulin, 4 (12.5%) on antidepressants, 13 (40.6%) on benzodiazepines, 7 (21.9%) on diuretics, 24 (75%) on PPI, 10 (31.3 %) on allopurinol, 15 (46.9%) on antihypertensives, 6 (16.8%) on sedatives, 2 (6.3%) on thyroid hormone, 18 (56.3%) on vitamins, 21 (65.6%) on phosphorus binders, 2 (6.3%) on steroids, 13 (40.6%) on analgesics, 12 (37.5%) on vitamin D, 7 (21.9%) on antihistamines, 13 (40.6%) on calcimimetics, 8 (25%) on calcium resin and 9 (28.1%) on betablockers.
The result of the SF-36 quality of life test was 61.43 (19.85) [32.22–89]. Table 2 shows the results of the Delta test.
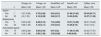
Correlations between stabilometric parameters and falls with the SF-36 score.
| Area95, cm2 | VyMax, cm/s | AreaEffect, cm2 | Yrange, cm | Xrange, cm | ||
|---|---|---|---|---|---|---|
| SF-36 | Pearson's correlation | −0.342 | −0.433 | −0.349 | −0.430 | −0.105 |
| p | 0.055 | 0.013 | 0.051 | 0.014 | 0.569 |
| Falls | Mean | SD | Standard error of the mean | |
|---|---|---|---|---|
| SF-36 | Yes | 56.09 | 20.748 | 2.678 |
| No | 63.87 | 18.662 | 1.624 | |
| p | Mean difference | Standard error of the difference | 95% confidence interval for the difference | |
| 0.010 | −7.782 | 3.010 | (−13.720; −1.844) |
| Delta test | Frequency | Percentage | Valid percentage | Cumulative percentage | |
|---|---|---|---|---|---|
| Valid | 0−9 | 26 | 81.3 | 81.3 | 81.3 |
| 10−15 | 5 | 15.6 | 15.6 | 96.9 | |
| 16−20 | 1 | 3.1 | 3.1 | 100.0 | |
| Total | 32 | 100.0 | 100.0 |
SD: standard deviation.
Significant relationships and the correlation coefficient are shown in bold.
The control group consisted of five males and four females with no related disease, with a mean age of 60 (18) [32–68]. Age and sex were not significantly different from those of the patients.
Postural stability of HD patients compared to the control group in the three situationsAnalysing the stabilometric parameters in the control group, no significant differences were found between the three situations studied.
The HD patients had greater loss of balance during the assessment of the test with EC compared to the controls: Yrange, AreaEffect and Area95 (Table 2). This difference was not significant in the tests performed with EO or COG.
In the HD patients, all the tests performed with EC, both in pre-HD and post-HD, showed a significantly greater loss of balance than the rest of the situations and among them, it was in post-HD and EC where the study's stabilometric variables showed a greater loss of balance. The descriptive values of the study variables according to the test conditions are detailed in Table 1.
Comparison of postural stability pre-HD and post-HDThe effect of dialysis on postural balance was evaluated and we found a significant increase in instability after dialysis. With EO there was a significant increase in Yrange values pre-HD 2.6 (1.1) and post-HD 3.3 (1.3) (p < 0.05), and in VyMax pre-HD 9.4 (5.5) and post-HD 15.1 (6.4) (p = 0.035). With EC, after dialysis there was a significant increase in the values for AreaEffect, pre-HD 3.1 (1.8) and post-HD 4.8 (4.1) (p < 0.05), and Area95, pre-HD 8.6 (5.7) and post-HD 12.9 (10) (p < 0.05). No significant differences were found in the variables analysed during COG.
Comorbidity, dialysis parameters, and length of time on dialysis in relation to postural stabilityA significant increase in instability was found in haemodialysis patients who had diabetes (n = 13). Before dialysis, these patients presented a greater loss of balance with EC. After dialysis and with EC, instability in patients with diabetes increased significantly, as shown in Table 3.
Stability parameters in the patients with diabetes (n = 13) compared to those without diabetes (n = 19). Eyes closed post-haemodialysis.
| Diabetic | Mean | SD | p | |
|---|---|---|---|---|
| AreaEffect, cm2 | Yes | 6.7 | 3.4 | 0.028 |
| No | 3.4 | 2.6 | ||
| Yrange, cm | Yes | 5.8 | 3.2 | 0.049 |
| No | 4.0 | 1.7 | ||
| Area95, cm2 | Yes | 17.7 | 12.8 | 0.037 |
| No | 9.6 | 7.9 | ||
| VyMax, cm/s | Yes | 26.5 | 18.6 | 0.021 |
| No | 14.5 | 8.5 |
SD: standard deviation. Statistically significant differences are shown in bold.
The rest of the comorbidities studied were not related to balance.
The HD technique and data and the haemodynamic data were not associated with balance, except for Kt/V, which was associated in the EC and COG tests; this significance disappeared when corrected for weight.
Association between the patient's laboratory values and postural stabilityOnly four patients had hyponatraemia (Na <136 mmol/l); these patients showed greater loss of balance in the pre-HD COG situation, Yrange: 2.97 (2.1) vs 2.09 (0.5), p = 0.038; Area95: 6.31 (6.12) vs 2.67 (1.17), p = 0.009; and AreaEffect: 2.27 (2.1) vs 0.95 (0.46), p = 0.009 respectively.
No significant correlation was found between the rest of the analytical values studied and the balance parameters.
Association of medication with postural stabilityThe drugs associated with greater imbalance parameters (EC + post-HD) were insulin, antiplatelet agents and betablockers. The differences in these parameters are shown in Table 4. Other drugs, such as statins, benzodiazepines, diuretics, PPI, allopurinol, antihypertensives, phosphorus binders, analgesics, vitamin D and cinacalcet, showed no association.
Association of the stabilometric parameters with eyes closed and post-haemodialysis with the intake or not of drugs.
| Xrange, cm | Yrange, cm | AreaEffect, cm2 | Area95, cm2 | VyMax, cm/s | ||
|---|---|---|---|---|---|---|
| n | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Insulin | ||||||
| Yes | 7 | 5.37 (2.65) | 6.75 (3.36) | 8.04 (5.51) | 21.86 (14.54) | 30.34 (20.71) |
| No | 25 | 4.0 (1.53) | 4.19 (2.08) | 3.86 (3.17) | 10.43 (8.28) | 16.37 (11.09) |
| Betablockers | ||||||
| Yes | 9 | 5.23 (2.45) | 6.28 (3.16) | 7.34 (4.95) | 19.51 (13.28) | 26.61 (16.69) |
| No | 23 | 3.98 (1.50) | 4.15 (2.11) | 3.76 (3.31) | 10.36 (8.73) | 16.61 (13.0) |
| Anti-platelet agents | ||||||
| Yes | 14 | 4.63 (2.29) | 5.85 (3.34) | 6.57 (5.2) | 17.36 (13.55) | 24.53 (17.97) |
| No | 18 | 4.10 (1.48) | 3.89 (1.38) | 3.38 (2.28) | 9.49 (6.66) | 15.45 (10.13) |
SD: standard deviation.
Statistically significant differences with p < 0.05 are shown in bold.
The incidence of falls was recorded in the six months following the assessment. Seven patients suffered one fall, three more than one, and 22 had no falls. Five patients required hospital care. All the patients who suffered falls had statistically significant (p < 0.05) greater loss of balance in the variables Yrange, Xrange, Area95 and AreaEffect than those who had no falls. The patients who fell had obtained significantly higher values in AreaEffect and YRange in the pre-HD EC test; these patients also obtained higher values with post-HD EC in the variables Xrange and Area95.
Relationship of quality of life with balance disordersThe quality of life assessment showed a significant inverse correlation (p = 0.036) between VyMax (EC + post-HD) and the SF-36 assessment (Table 2).
DiscussionIn this study, we found that patients with CKD undergoing HD had greater postural instability than subjects in the control group. The instability was greater with EC and post-HD.
This study shows that the HD session has a negative effect on postural stability. The patients have greater instability after the session, although we are unable to specify what factor or factors may be involved. These findings were also demonstrated in the studies by Erken et al.10 and Magnard et al.,12 while, using a different type of instrument for postural analysis in older patients on HD, other authors were not able to show that the HD session had a significant effect,13 although they were self-critical of their methodology.
The determination of postural instability using stabilometry and specifically by studying the displacements of the body CoP has been shown to be an objective, easy and reliable method to assess postural balance.26 As demonstrated in the studies by Golriz et al.,25,27 in which they use the platform used in our study as a reference platform, not all the platforms used have the same accuracy.
The fact that postural stability worsens with EC could be due to the fact that proprioceptive sensitivity and/or vestibular function would be altered in patients with CKD on HD.28 The dysfunction of the proprioceptive system could be explained by the peripheral neuropathy which is common in these patients, and that of the vestibular system by changes in body fluids that could affect the endolymph. Shin et al. showed that HD patients had poorer postural control than healthy control subjects, particularly while performing a cognitive task.14 These patients had a mean age of 48 years, clearly younger than that of our study. Age would be directly related to pre-HD postural instability and risk of falls.10 Our patients had a mean age of 68 years with scant dispersion, making it difficult to assess this factor.
In these studies, other tests have been used to assess physical function in HD patients, such as the Short Physical Performance Battery,20,29 with time taken to stand up from a chair and sit down again, walking speed and balance tests, calculating a score with tests of physical or cognitive ability; HD patients with systolic blood pressure above 130 mmHg have been found to have better physical function than patients with normal blood pressure below said value. In our study, we found no significant relationship between peri-dialysis blood pressure and postural balance. These authors conclude that the goal of aggressive blood pressure control in HD patients should be reconsidered, particularly for those with a low functional level. In HD patients, poorer physical function could be due to their CKD, but also to aspects of the HD itself. The severity of the CKD and having a GFR between 20−70 ml/min is associated with poorer physical function (Short Physical Performance Battery).20
In our study, postural instability was more marked in patients with diabetes. Patients with type 2 diabetes tend to have more stability problems and a higher risk of falls.21 As patients with diabetes may take more medication and have more problems with gait, peripheral neuropathy and impaired cognitive function, they belong to a sub-population requiring preventive measures to avoid falls.
In addition to the HD, these patients have other risk factors associated with postural instability, one of which is some of the drugs they are taking. HD patients are prescribed multiple medications. Of the drugs in our study associated with worse stabilometry, some were directly related to the nervous and muscular systems, but in others, the relationship was unclear. When prescribing new drugs for these polymedicated patients, the risk of affecting balance and increasing the risk of falls needs to be taken into account.
Hyponatraemia was a factor associated with greater postural instability in COG. The association between hyponatraemia and deterioration in brain functions has been clearly demonstrated.8,22 In fact, hyponatraemia can act as a direct toxin to the brain, causing encephalopathy. At the same time, there are situations in which the association between hyponatraemia and mortality is even greater, such as in cirrhosis or heart failure, and which are also more prevalent in HD patients.23 It has been suggested that the capacity for cognitive performance is limited and that using it may compromise its use for other functions, such as maintaining balance. One recent study24 included 4,153 patients on HD. The mean age was 64.7 years, the patients were predominantly male (64.2%) and 34.8% had diabetes. Patients whose natraemia level was below 136 mEq/l had a higher independent risk of mortality than the rest (OR 1.62). In 2016, the Falls Committee at Hospital General Universitario Gregorio Marañón conducted a study to determine the effect of hyponatraemia (Na+, p < 135 mEq/l) on the risk of falling.30 They carried out a case-control study on 207 selected patients, and concluded that having hyponatraemia quadruples the risk of falling compared to not having hyponatraemia, with an OR of 4.34 (1.37–6.00) and a Pearson's χ2 of p < 0.004.
Falls are associated with postural instability and a high mortality rate.31,32 In our study, we found an association between some of the stabilometry data and falls. The observed incidence of falls, 0.63 falls/patient/year, was lower than that found by Desmet et al.,32 1.18 falls/patient/year in HD patients, with a similar mean age of 70.9 years, and higher than that in individuals not on dialysis (0.32−0.7 falls/patient/year). Other studies have found a lower incidence of falls; 26.3% in 12 months.33 Patients with falls had a 2.13-times greater risk of death than those with no falls. The difference in incidence most likely depends on the inclusion/exclusion criteria in the different studies. Falls in HD patients would be more common after dialysis (73%) than before (27%).34 Suggested risk factors for falls include age, diabetes, the number of medications taken (some in particular, such as antidepressants) and poorer cognitive function. Roberts et al.34 focused on possible autonomic nervous system dysfunction and orthostatic hypotension in relation to fluid shifts. The HD session could, in itself, influence the risk of falls, affecting strength and mobility.12,21 When we consider the consequences in terms of quality of life, associated morbidity and the reduction in life expectancy, the prevention of falls is of utmost concern.18,19
Patients with more abnormal stabilometry parameters showed worse perceived quality of life in the SF-36 test. Postural instability creates insecurity and limitations in mobility, and this factor is likely to heavily influence a patient's perception of their quality of life.
The main limitation of this study is the small sample size. The scope of the study involved patients with the ability to maintain an upright position in the three situations studied. Many of the patients on HD in our setting are unable to mobilise or remain in an upright position independently. The Delta test shows that 26 of the 32 patients had a score of 0–9 and only one was above 16.
There is a variety of analytical methods for measuring instability, from the 1989 Berg scale to the use of the Wii™ Balance Board. We can classify the different methods into ordinal item scales, tests based on spatial-temporal measures, analysis of visual perception, or posturography through the use of force or pressure platforms. The validity of many of these tests has been studied and proven, and their limitations defined. The use of force platforms has been more limited owing to the high cost of the necessary equipment, but they are instruments with a high degree of reliability and precision for quantifying possible balance disturbances. The body sway around the CoP in the lateral and anterior/posterior planes, the velocity of these movements, and the area covered by the CoP trajectory are some of the variables these platforms measure and which have been associated with postural instability and the risk of falls.35,36
Stabilometry could be used to identify patients with a higher risk of falls, in order to apply prevention measures and early intervention, by way of exercise and improvements in the dialysis process.37,38
ConclusionsAnalysis of postural stability using a validated force platform shows that HD patients have poorer postural control than healthy individuals. Moreover, their postural balance is worsened by the effect of the HD session, compared to healthy individuals or controls, and even to themselves before undergoing the dialysis process. All of these differences are accentuated when performing the test with EC, or with another added factor, such as diabetes or hyponatraemia, or certain drugs.
Postural imbalance has a negative effect on patients' quality of life and can lead to falls and their potential adverse consequences. Detection and prevention tools therefore need to be applied to pre-empt such situations.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pérez-Gurbindo I, Angulo Carrere MT, Cobo PA, et al. Los pacientes en hemodiálisis presentan peor equilibrio postural, que se relaciona con el riesgo de caídas. Nefrologia. 2020;40:655–663.