Guillain-Barre syndrome (GBS) manifests itself as a progressive and symmetrical muscular weakness in lower limbs and arreflexia. Occasionally, patients require invasive ventilation and with a 15–30% mortality rate.1 The association between respiratory and gastrointestinal infections is well known and occurs in two-thirds of cases.2,3 In a solid organ transplant it is a rare complication, however it is slightly more frequent in bone marrow transplantation. However, Guillain-Barre syndrome is an exceptionally rare complication in a nephrotic syndrome patient, treated with tacrolimus and whose renal biopsies reveal the separate entities, a focal and segmental glomerulofritis and a IgA nephropathy. We present the case of a 65-year-old patient with multiple comorbidity, nephrotic syndrome secondary to focal and segmental glomerulofritis and an IgA nephropathy treated with tacrolimus and drifting into in a Guillain-Barre syndrome.
This is a 65-year-old patient who was referred to a nephrology department from primary care in 2014 because of proteinuria and uncontrolled blood pressure. Among the personal history, it can be highlighted in Table 1. He was firstly seen in October 2014 at nephrology consultation. He was in a good general condition. Analysis revealed GFR>60 (MDRD) Cr 1.1mg/dl Hb 11mg/dl, Na 136mmol/l K 4.3mmol/l, proteinogram with inflammatory profile, good diuresis, unchanged immunological profile, ACRO 3600mg/g, proteinuria of 4g/24h, no hypoprhoeaemia, Alb 3mg/dl and TP 6mg/dl. There was no anemia. Immunoglobulins were not altered.
Personal history.
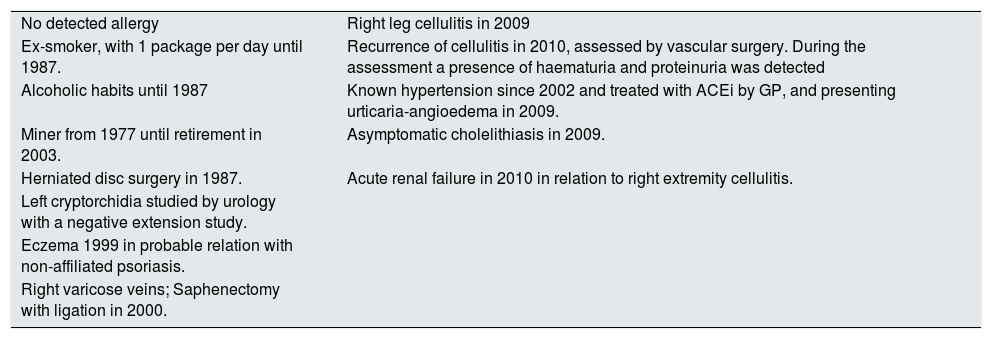
| No detected allergy | Right leg cellulitis in 2009 |
| Ex-smoker, with 1 package per day until 1987. | Recurrence of cellulitis in 2010, assessed by vascular surgery. During the assessment a presence of haematuria and proteinuria was detected |
| Alcoholic habits until 1987 | Known hypertension since 2002 and treated with ACEi by GP, and presenting urticaria-angioedema in 2009. |
| Miner from 1977 until retirement in 2003. | Asymptomatic cholelithiasis in 2009. |
| Herniated disc surgery in 1987. | Acute renal failure in 2010 in relation to right extremity cellulitis. |
| Left cryptorchidia studied by urology with a negative extension study. | |
| Eczema 1999 in probable relation with non-affiliated psoriasis. | |
| Right varicose veins; Saphenectomy with ligation in 2000. |
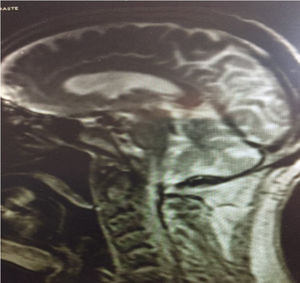
With a normal abdominal ultrasound, a renal biopsy was performed with a diagnosis of focal and segmental glomerulonegritis. Treatment with corticosteroids was started with a 1mg/kg/day on September 2015. The following month the patient had to be hospitalized in internal medicine presenting an adison crisis in relation to the suppression of the steroids by the patient. The patient remained hospitalized for a few days, the corticotherapy was reintroduced and he was discharged. At January 2016 corticoresistance was verified, a proteinuria of 5.5g in 24h was observed. Treatment with cyclosporine was initiated with a poor response and multiple side effects. Therefore, it was suspended after three months of use and a change to mycophenolate mofetil 1000mg/12h was made. From October to November the patient was hospitalized do to anasarca and nephrotic syndrome. A second renal biopsy was performed and tacrolimus was initiated adjusted to the levels of (range 8–12ng/ml). The subsequent biopsy reveals IgA M1 E1 S1 T1 nephropathy in the Oxford classification. The patient appears once again at the emergency room in January 2017, presenting general deterioration with important loss of tone and mobility at the lower limbs, that has been progressive. Subsequently the patient manifested that it started to occur mildly several weeks after the onset of tacrolimus. Given the suspicion, of a possible Demyelinating neuropathy by tacrolimus or a GBS, the consultation to neurology was made and the drug was progressively withdrawal. An MRI of the skull was performed (Image 1), a lumbar puncture reflected proteins 76mg/dl and glucose of 68mg/dl. Secondary causes of GBS were also discarded. The neurophysiological study was done with the following result: signs of symmetrical generalized peripheral neuropathy (sensory polyneuropathy) of probable axonal origin and moderate-severe intensity, with greater involvement of the lower extremities. However, the symmetrical progression of the affection makes more suspicion a GBS. The patient was seen by psychiatry and rehabilitation, with current monitoring of the two specialties. He continued his treatment with a lower dose prednisone. At discharge his Glomerular Filtration was over 60ml/min, a Cr of 1.2mg/dl and a proteinuria of 6g/24h. Overall condition improved considerably from admission.
GBS is an uncommon disease with a worldwide incidence of 1–2 cases per 100,000/year,4 while the incidence of GBS in patients receiving tacrolimus secondary to the nephrotic syndrome is not known. This syndrome, often described as an immunological disorder, has been thought to be rare among immunosuppressed patients, since immunosuppression acts as a protection. The pathophysiology of tacrolimus toxicity is not well studied, although most cases are described in association with high systemic levels of the drug. Although nerve conduction studies in patients with tacrolimus polyneuropathy may also show evidence of demyelinating changes,5 the symmetrical ascending presentation and the absence of a history of elevated tacrolimus levels goes toward the diagnosis of GBS over tacrolimus polyneuropathy.6 The treatment of GBS secondary to tacrolimus in patients with nephrotic syndrome is not known, except the withdraw of the medication. Even this case is exceptionally rare, it is necessary to take into account the presence of this pathology when the medication is used, an early and timely diagnosis, would avoid greater sequelae in all the patients that might be affected.
Please cite this article as: Jakovler IR, Nieto CP, Antonio MR, Blanco FS, Javier RM. Síndrome Guillain-Barré secundario a tacrolimus en paciente con síndrome nefrótico corticorresistente secundario a glomerulonefritis focal y segmentaria y nefropatía IgA. Nefrologia. 2018;38:665–666.