Objetivo: la nefropatía diabética es la causa más común de entrada en tratamiento renal sustitutivo en España, con una incidencia que parece estable desde 1997. Los datos sobre incidencia de nefropatía diabética en consulta son escasos al no existir registros similares a los usados en el tratamiento renal sustitutivo. Diseño y métodos: se ha revisado retrospectivamente la base de datos de la consulta de Nefrología de nuestro hospital entre enero de 1991 y diciembre de 2006. El diagnóstico se hizo en la mayor parte de los casos por criterios clínicos (proteinuria asociada a retinopatía diabética). En 21 casos se realizó biopsia renal por incumplimiento de estos criterios. Resultados: durante ese tiempo, 478 (49,7 pmp) pacientes fueron diagnosticados de nefropatía diabética (edad media 61,2 años, 50,4% mujeres). Se aprecia una tendencia progresiva de crecimiento desde 33,3 pmp en 1991 hasta 76,2 pmp en 2006. No se han producido variaciones significativas en la edad media de los incidentes. Ciento seis pacientes (22,1%) han iniciado tratamiento renal sustitutivo. En el resto de los casos, el diagnóstico más frecuente fue nefroangiosclerosis (129) y glomerulonefritis (n = 103). La supervivencia estimada antes de llegar a tratamiento renal sustitutivo fue del 87,5% al año y del 48% a los cinco años de seguimiento. Conclusiones: la incidencia de nefropatía diabética parece tender a crecer significativamente en los últimos años, sobre todo en el grupo de edad mayor de 70 años. A pesar del perfeccionamiento de los tratamientos, el pronóstico sigue siendo desfavorable. La mayor permisividad en la edad para la derivación puede haber influido en estos resultados.
Objective: Diabetic nephropathy is the most common cause for starting renal repacement therapy in Spain with a steady incidence since 1997. Data on incidence of diabetic nephropathy previously to dialysis are scanty because they are not registries similar to those used for renal replacement therapy. Design and methods: It have been retrospectively studied the records of our hospital Nephrology outward from January, 1991 to December, 2006. Diagnosis was commonly made using clinical criteria (proteinuria plus diabetic retinopathy). There were 21 cases which did not meet theses criteria and so renal biopsy was performed. Results: During this time 478 (49.7 pmp) patients were diagnosed of diabetic nephropathy (mean age 61.2 years, 50.4% women). Incidence increased from 33.3 pmp (1991) to 76.2 pmp (2006). There were not significant changes in the age of patients along the time. Other common diagnosis in diabetic patients were nefroangiosclerosis (129) and glomerulonefritis (n = 103). Survival until renal replacement therapy was 87.5% at one year and 48% at five years of follow up. Conclusions: Incidence of diabetic nephropathy seems to have increase last years specially in the patients aged 70 or older. In spite of therapeutic improvements the prognosis is still unfavourable. Less rectricted age criteria for submitting patients may have influenced these results.
INTRODUCTION
Diabetic nephropathy incidence, measured by the percentage of patients diagnosed with this failure in relation to the total number of patients who initiate Renal Replacement Therapy (RRT), increased significantly in Spain towards the end of the 90s.
In 1990, diabetic nephropathy was one of the least common reasons for admission to RRT compared with idiopathic glomerulonephritis;1 however, by1999 it had become the most common reason for initiating dialysis treatment in Spain (21% of all patients), according to data published by Spanish Society of Nephrology and ONT Registry in collaboration with different Regional Registries.2 The data from subsequent years do not appear to indicate significant changes in incidence rates, though there has been a slight increase in the number of incidences (24%) and a significant increase between those aged between 65 and 75 (30% of cases occurred in RRT patients).3 Incidence in Spain is still lower than that of the United States, which stands at around 45%.4
Nevertheless, despite the relevance of this failure, there are little data regarding the incidence of patients diagnosed with diabetic nephropathy in nephrology clinics. The incidence of kidney failure in type I patients seems to be similar to that of other European countries; however, these patients only represent a very small percentage of those who have diabetes mellitus.5 No new data on this subject has been published since our findings were published in 1996, which was the first time an increase in diabetic nephropathy diagnosed in a nephrology clinic in Spain had been documented6. The annual incidence of diagnosed cases of diabetic nephropathy in our clinic during the period of 1991 to 2006 has been reviewed. The survival rate during this period before initiating haemodialysis has also been calculated as no data has been published on this subject in Spain ever since treatment with reninangiotensin system blocking agents was universally introduced.
DESIGN AND METHOD
The nephrology clinic database in Infanta Cristina Hospital, which contains details of all patients diagnosed since October 1990, was retrospectively reviewed. The review spanned the period between 1st January 1991 and 31st December 2006. The number of diabetic patients that were seen during this period was examined. In most cases the diagnosis was made using clinical criteria (proteinuria above 500mg/day or microalbuminuria above 300mg/day associated with documented diabetic retinopathy confirmed by examining the back of the eye). A kidney biopsy was carried out to confirm the diagnosis in those cases where the patient did not present diabetic retinopathy and proteinuria was above 1g/day, after patient consent was obtained. Kidney failure in the absence of proteinuria or macroalbuminuria was not considered a diagnostic criterion.
According to the National Statistics Institute (INE), the population of Badajoz was 676,936 in 1990 and 672,029 in 2008. The population has fluctuated during this period and was at its lowest when it fell to 650,938. Subsequently, incidence rates have been calculated per million people for this Health Area that served approximately 660,000 people between 1991 and 2006 (which corresponds to the entire population of the province of Badajoz). The Nephrology Unit in the Regional Hospital of Zafra was opened in 2002 and covers a health area that includes approximately 135,000 people, therefore incidence rates have been calculated for a population of 525,000 that were seen between 2002 and 2006. The few patients that came from the area around Zafra from that date onwards were not included in the study.
The survival of patients was calculated according to the Kaplan-Meier method using terminal kidney failure (creatinine clearance <15ml/min, stage 5 KDOQI guidelines) or the admission to renal replacement treatment as the censoring variable. Calculations were done using the statistics package SPSS version 13.0 for Windows. The results were expressed as the mean or median.
RESULTS
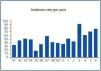
During this time, a total of 4,875 patients were seen. Of these, 1,140 had diabetes mellitus and 478 were diagnosed with diabetic nephropathy in accordance with the aforementioned criteria. The mean incidence of diabetic nephropathy throughout the period studied was 49.7pmp, with an average age of 61.2 ± 14.2; 50.4% of these were women and 49.6% were men. In 21 cases, the diagnosis of diabetic nephropathy was made by carrying out a biopsy in the absence of diabetic retinopathy. Among the rest of the diabetic patients studied, the most common diagnosis was nephroangiosclerosis (129), primary or secondary glomerulonephritis (n = 103, 76 of which were confirmed following a kidney biopsy), and interstitial nephropathy or chronic pyelonephritis (n = 80). A progressive increase in incidence from 33.3pmp in 1991 to 76.2pmp in 2007 was observed. Average incidence rates were 38.5pmp from 1991 to 1995; 42.1pmp between 1996 and 2000; and 65.1 from 2001 to 2006 (figure 1).
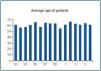
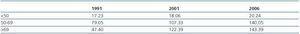
There were no significant variations in the average age of patients throughout the period of study (figure 2). However, when incidence was adjusted for age, an increase in the number of cases affecting patients over 70 was observed. (table 1).
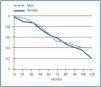
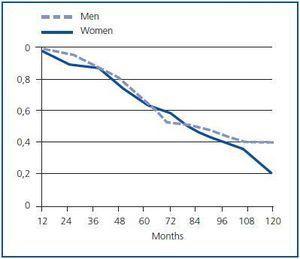
The data corresponding to those patients that were seen between 1st January 1990 and 31st December 2001 were used in order to calculate survival rates. There were a total of 225 patients, 103 (45.7%) of which initiated renal replacement treatmentduring this period. The estimated mean survival was 83.4 (6.25) months and the median survival was 49.0 (11.5) months. The survival curve is shown in figure 3. The estimated survival rate was 87.5% after one year and 48% after five years. Men (n = 106) had a median survival of 84.0 (24.9) months, while for women (n = 119) it was 42.0 (8.5) months. The same difference was identified in the mean values: men 95.2 (9.4); women, 65.6 (5.9) months. The survival curves are shown in figure 4. The differences between them do not reach statistical significance (p = 0.0598).
DISCUSSION
Despite diabetic nephropathy is now one of the main reasons for admitting patients to RRT in Spain, our data suggests that incidence will continue to increase over the next few years, bringing us closer to levels observed in the United States. Poor patient progress reinforces this idea despite the fact that all patients in this study received renin-angiotensin system blocking agents in accordance with the established recommendations (angiotensin receptor antagonists in recent years).7
There are practically no data published in Spain regarding the incidence of diabetic nephropathy prior to admission to renal replacement therapy, apart from the data collected in our own clinic from the early 90s.6 It is difficult to reduce the data collection area in most nephrology departments, except when they serve a single province and when immigration is low in the region and the number of patients transferred from other parts of Spain or the rest of the world is limited, as was the case in this study. Although the Health Area covering Badajoz is divided, it is clear from the registry when a patient comes from the other area. Furthermore, the closed structure of the health system makes it very difficult for these patients to register with us. This also occurs to a certain extent in the other province in this region, which rarely shares patients with us for the same reason. Therefore, the incidence rates of diabetic nephropathy observed in this study reliably reflect the current situation.
Unlike our region, those that have a significant number of South American and black immigrants may have higher incidence rates of diabetic nephropathy given that these populations are more prone to developing kidney failure according to epidemiological statistics.4 Furthermore, the number of patients admitted to renal replacement therapy because of diabetes mellitus has traditionally been above the Spanish average in Extremadura without reaching the high incidence reported in the Canary Islands, despite the absence of an immigrant population.1,2 Therefore, this data may be extrapolated to the rest of the country, although complete accuracy cannot be guaranteed.
The ideal method for diagnosing diabetic nephropathy is a kidney biopsy, although this technique involves a degree of risk and a significant workload. Given that proteinuria and diabetic retinal lesions together have high specificity for diagnosing diabetic nephropathy, these criteria are generally considered reliable enough in order to be able to make a definitive diagnosis. When diabetic retinopathy is not present in type I diabetes patients with urine abnormalities, another kidney failure should be considered given that eye failures and kidney failure are often concurrent (90% of cases).8 These two indicators coincide less frequently (in approximately 60% of cases) in patients with type II diabetes, therefore the absence of retinopathy does not rule out the possibility of diabetic nephropathy.9 Biopsies are generally reserved for those patients with proteinuria who do not present retinopathy, which was the case in this study. Our data support this view since, of the 124 patients that underwent a kidney biopsy, less than 17% presented diabetic glomerulosclerosis lesions in the kidney biopsy sample (in other words, 83% presented a different type of kidney lesion).
Nevertheless, the opposite error may also have occurred; in other words, when patients presented proteinuria caused by something other than diabetes together with retinal lesions caused by diabetes mellitus, this could have been mistakenly diagnosed as diabetic nephropathy. However, autopsies of diabetic patients indicate that non-diabetic kidney failure is extremely uncommon.10 On the other hand, a retrospective study that was carried out to establish the factors that indicated non-diabetic kidney failure involving 109 diabetics showed that 12% of type I diabetics and 28% of type II diabetics presented another kidney failure that was or was not associated with diabetic nephropathy in the biopsy.11
Patients referred because of microalbuminuria or proteinuria <500mg have not been included in the diagnosis of diabetic nephropathy for two reasons. The first is that microalbinuria testing was practically unavailable in the primary health care system between 1990 and 2000. Including these patients would have introduced bias into the study because it would have resulted in an even greater increase in the incidence of diabetic nephropathy simply because of the improvement in diagnostic techniques. The second is that microalbuminuria is not a criterion for referring patients to the nephrology clinic unless the patient fails to respond to treatment. Therefore, most patients with microalbuminuria are not referred (if this were the case, there would be more patients with microalbuminuria than patients with proteinuria and/or kidney failure).12,13
It is clear that the real incidence rate of diabetic nephropathy is higher than the one indicated in this study, given that the primary inclusion criterion was that patients had to have been diagnosed in the nephrology clinic and it is most likely that many patients were never referred (at least during the initial phases of the failure) or did not want to come to theclinic for a variety of reasons, including age or distance. The criteria for referring patients with proteinuria or kidney failure did not change during this period. However, the same cannot be said of the criteria for patients with microalbuminuria, whichis why they have not been included in this study.
The reasons behind the increased incidence of this failure are unclear. It seems that age may have influenced the results. On the one hand, the censuses show that the population has aged. On the other, it is possible that referral criteria may have been modified, increasing the age limit over time. With regard to the role of diet in the pathogenesis of diabetic nephropathy, it is worth highlighting that Spanish eating habits have changed over the years with an increase in the amount of protein and fat consumed.14 In fact, the improved economic situation in other countries since the 50s correlates with a progressive increase in the prevalence of diabetes mellitus.15 The same can be said of the situation in Spain: the surveys carried out in Spain since the 50s also seem to suggest a progressive increase in the prevalence of this failure, reaching similar levels to those observed in central Europe.16,17 The prevalence of microalbuminuria, the ominous first sign of diabetic nephropathy, is the same as in the surrounding European countries.18 Similarly, the prevalence of metabolic syndrome is the same as that of other developed countries.19 However, in Spain there does seem to be a delay in establishing the same epidemiological patterns as those identified in other countries that underwent greater development earlier on.
In conclusion, it is possible to say that diabetic nephropathy incidence in the nephrology clinic continues to increase with time. Despite therapeutic advances, patient prognosis continues to be poor in the majority of cases.
Figure 1.
Figure 2.
Table 1. Age-adjusted incidence rate
Figure 3.