To the Editor,
Sarcoidosis is a multisystemic disease which affects the kidneys in between 4% and 20% of cases. Disorders of calcium metabolism such as hypercalcaemia and/or hypercalciuria, nephrolithiasis, and tubular dysfunctions are the most common kidney disorders.1 Glomerular disorders associated with sarcoidosis have also been reported, among which membrane glomerulonephritis is the most common.2 Interstitial granulomatous infiltration is usually silent and rarely manifests as acute kidney failure, and if this does happens, damage to other organs is usually evident. Kidney failure caused by granulomatous interstitial nephritis (GIN) in the absence of extrarenal sarcoidosis is an extremely rare clinical condition.
We present the case of a patient with acute renal failure caused by sarcoidosis affecting only the kidneys.
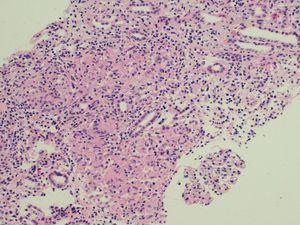
The patient was a 56-year-old woman with no allergies or substance abuse and with no medical history of interest or regular medical treatment. She was referred to emergency services by her family doctor after an abnormal blood test (creatinine 8mg/dl), carried out to study a toxic syndrome of 6 to 7 months evolution with a weight loss of 10 kg. She had an analysis carried out 5 months earlier in a check-up at work which highlighted a Hb level of 11 g/dl and creatinine level of 1.7 mg/dl. The patient had normal blood pressure in the physical examination, and pale mucous membranes; everything else was normal. Analyses showed results of Hct/Hb 28 %/9.6 g/dl, urea/creatinine 192/9.4 mg/dl (estimated GFR 4ml/min), calcium 10 mg/dl, FENa 10. Proteinuria 0.6 g/24 h, and sediment was normal. PTHi and vitamin D levels were normal. Patient was negative for HbsAg, HCV and HIV. Immunological study: ANA, anti-DNA, ANCA, serum complement and immunoelectrophoresis were normal or negative. The Rose Bengal test for anti-Brucella antibodies was negative. Urine culture in Löwenstein-Jensen medium was negative. The PPD skin test was negative. ACE levels were 189 U/l (8-52 U/l). The chest x-ray, abdominal ultrasound and CT scan of chest, abdomen and pelvis were normal. No significant changes were found in the eye and ENT examinations. A jugular catheter was inserted and haemodialysis was begun. A percutaneous kidney biopsy was performed showing 10 glomeruli, 2 of them sclerotic, the rest with normal appearance. Large amount of granulomas comprised of epithelioid cells and Langhans multinucleated giant cells without necrosis (Figure 1) were observed in the interstitium. The histochemical techniques to detect fungi and acid-alcohol resistant bacilli were negative. Treatment began with prednisone at 1 mg/kg/day. The patient had conserved diuresis and haemodialysis was well tolerated. After four weeks of corticosteroid treatment, a progressive improvement in kidney function was observed, enabling her to stop the replacement treatment. At present, 4 months after starting treatment and with a dose of 0.3 mg/kg/day, she has a plasma creatinine level of 2.8 mg/dl (GF 19 ml/min) and a normal level of ACE.
GIN is a very rare histological diagnosis, found in between 0.5% and 0.9% of native kidney biopsies.3,4 It has been associated with drugs (mainly NSAID, allopurinol and antibiotics), infections (tuberculosis, brucellosis and fungal infections, among others), Wegener’s granulomatosis, crystal-induced nephropathy, paraproteinemia, TINU syndrome, idiopathic infections, and sarcoidosis. Joss et al. reviewed the cases of kidney biopsies performed in Glasgow over a 15-year period and identified a total of 18 GIN (in less than 1% of the total biopsies). Of these, 5 were due to sarcoidosis, 2 were associated with TINU syndrome, 2 were secondary to medication, and 9 were classified as idiopathic.5
Acute renal failure in sarcoidosis is mainly associated with hypercalcaemia, and in its chronic form with nephrocalcinosis.6 GIN is another cause of kidney disease in sarcoidosis, present in a third of patients with sarcoidosis and evidence of kidney disease. In 1987, Ford described the first association of GIN in a patient with sarcoidosis who developed acute renal failure.7 GIN in the absence of extrarenal sarcoidosis is very rare. Robson et al. presented 7 cases of GIN in the absence of extrarenal sarcoidosis.8 Of note is the predominance of men (71%), the mean age of 69, the severe renal failure at the time of presentation (calculated creatinine clearance of 14 ml/min), the need for temporaryy haemodialysis at onset in one case, minimal proteinuria (mean 0.4 g/day), high ACE levels in 3 patients, and good response to corticosteroid treatment in 5 cases (prednisolone at between 20 and 60 mg/day). Two patients needed to begin periodic haemodialysis at 3 and 15 months after diagnosis. The common histological characteristics were normal glomerular levels and the presence in the interstitial fluid of in the interstitial fluid composed of epithelioid cells and multinuclear giant cells.
It is worth highlighting the importance of kidney biopsies in cases of non-justified kidney failure, and in cases of suspected sarcoidosis in particular, given the variety of lesions it can cause. Performing a biopsy can optimize the choice of clinical treatment.
Figure 1. Kidney cortical