Hematuria in the absence of an obvious underlying condition (e.g., cystitis, nephrolithiasis) is quite common. In many such patients, particularly young adult patients, the hematuria is transient and of no consequence. Schistosomiasis is a disease that can cause hemorrhagic cystitis and be associated with bladder cancer.1,2 It is caused by Schistosoma haematobium, being more frequent in Africa and in the Middle East.3 The prevalence of schistosomiasis in Spain is not known. We present the case of a 20-year-old patient from Madagascar, in Spain for five years, who consulted for intermittent macroscopic hematuria secondary to genitourinary schistosomiasis, as well as intestinal parasitosis due to Trichuris trichuria and Necator americanus.
A 20-year-old patient who consulted in 2012 his primary care physician requesting a routine blood test and to complete his vaccine scheme. The patient presented intermittent macroscopic hematuria, isolated episodes of mictional symptoms and fever, on physical examination: suprapubic pain and no renal tenderness, being treated empirically with Azithromycin and Doxycycline. The follow up, a few months later, revealed the persistence of macroscopic hematuria with normal blood test and urinary test with abundant red blood cells and leukocytes, with an albumin/creatinine ratio of 300mg/mg. In 2013, the patient was seen by a specialist in urology performing a urological ultrasound, that ruled out alterations of the urinary system. With no other findings, the patient was sent for a nephrology consultation. On his first visit, the patient presented respiratory infection with a dry cough. On physical examination only slight wheezing in the left lung was found. Urinary sediment alterations persisted with an important eosinophilia on the blood test. Immunological tests, as well as abdominal ultrasound were negative, viral serology reported presence of antibodies against hepatitis B virus. No other test were performed due to the lack of social security card according the healthcare laws at that time.
In November 2016, the patient appears ones again at the nephrology consultation with the same clinical sings as in 2012. The blood tests showed: hemoglobin 15.6g/dl, leukocytes 7480/μl with 36% neutrophils and 17% eosinophils, platelets 172000/μl, creatinine 0.6mg/dl with estimated glomerular filtration rate >90ml/min/1.73m2, potassium 5.2mmol/L sodium 138mmol/L, iron 40μl/dl, ferritin 18ng/ml, urinary sediment: 163 leukocytes/μl, 104 RBC/μl.
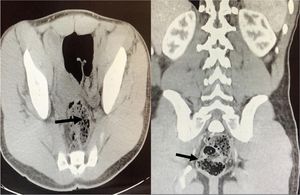
Abdominal ultrasound was repeated, showing both kidneys with apparent discrete diffuse cortical thickening and slight bilateral and symmetric calyceal ectasia, repleted bladder with internal echoes (detritus and fibrin). To complete the study an Uro-TAC (Fig. 1) was performed, with findings suggestive of urinary schistosomiasis. The urine parasitological test revealed: abundant Schistosoma haematobium eggs. Simultaneously the parasitological study of feces found Trichuris trichuria and Necator americanus eggs. The patient was referred to Internal Medicine and treated with Albendazole and Praziquantel, with negative subsequent parasitological tests; continuing with frequent trips to Madagascar and Mozambique.
Schistosomiasis is a parasitic disease caused by flatworms of the trematode class, of the genus Schistosoma. It is relatively common in developing countries, especially in Africa.4 Although its mortality rate is low, schistosomiasis is highly disabling, having a great health and economic impact. There are five species that produce human disease, each one with its respective clinical manifestations: Schistosoma mansoni and intercalatum: intestinal schistosomiasis, Schistosoma haematobium: urinary schistosomiasis, Schistosoma japonicum and mekongi: Asian variety.
The clinical and epidemiological diagnosis is guided by the anamnesis, deducting possible contact with water from endemic or high-risk areas.5,6 Patients usually present with microscopic or macroscopic hematuria, pyuria, and in longstanding infection an obstructive uropathy due to granulomatous inflammation fibrosis or calcification of the urinary tract. Identification of the eggs in feces or urine by microscopy techniques is the most practical diagnostic method, being the unit of measurement the number of eggs per gram of feces or urine. In case of suspicion of S. haematobium, the urine test is preferable. In cases of negative results, a bladder biopsy can be done.
One of the most effective drugs against the acute phase of schistosomiasis is Praziquantel; although there are others equally efficient, as commonly used Albendazole and Metranidazole.7 However, it does not prevent reinfection.8 Even if in some young adult patients the hematuria is transient and of no consequence, in others must be studied thoroughly to find its cause, specially in patient with frequent contact with endemic areas of Schistosomiasis.
Please cite this article as: Narváez A, et al. Esquistosomiasis genitourinaria como causa de macrohematuria persistente en paciente de 20 años natural de Madagascar, asociado a parasitosis intestinal por Trichuris trichuria y Necator americanus. Nefrologia. 2019;39:559–560.