Lactic acidosis associated with metformin is a rare complication (9/100,000 person years).1–3 However, it is also serious, and usually occurs in association with certain predisposing conditions, all of which are absolute contraindications for the use of metformin: acute kidney injury; severe chronic kidney disease; liver disease; alcohol abuse; congestive heart failure; coronary heart disease; age >80; and tissue hypoxia states accompanied by haemodynamic instability.4 Lactic acidosis is defined as pH<7.35, blood lactate >2.0mmol/l and PaCO2<42mmHg.
We studied 30 patients treated with metformin who attended the Accident and Emergency department (1 September 2016 to 30 September 2017) and were found to have lactic acid levels in blood above 2mmol/l. Fourteen patients required haemodialysis (HD). Haemodialysis was indicated following the usual clinical and analytical criteria in acute kidney injury: oliguria/anuria; fluid overload; severe water/electrolyte or acid/base alterations; and elevation of nitrogen products. Metformin clearance could not be monitored because our hospital’s laboratory does not measure metformin levels.
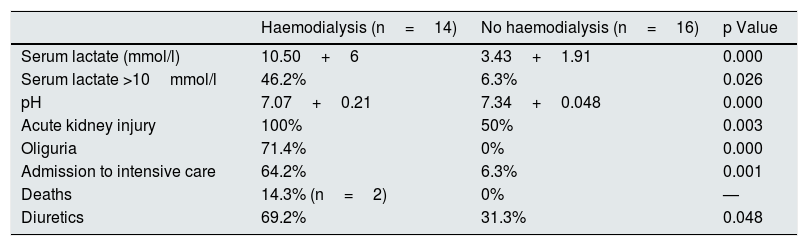
From a clinical point of view (Table 1), patients who required HD had a higher blood level of lactic acid i (10.50±6.61 vs 3.43±1.91mmol/l; p=0.000), lower pH (7.07±0.21 vs 7.34±0.048; p=0.000), a higher rate of associated acute kidney injury (AKI) (100% vs 50%; p=0.003) and a higher rate of admission to ICU (64.2% vs 6.3%, p=0.001).
Clinical differences between patients taking metformin with lactic acid above 2mmol/l according to the need for haemodialysis.
| Haemodialysis (n=14) | No haemodialysis (n=16) | p Value | |
|---|---|---|---|
| Serum lactate (mmol/l) | 10.50+6 | 3.43+1.91 | 0.000 |
| Serum lactate >10mmol/l | 46.2% | 6.3% | 0.026 |
| pH | 7.07+0.21 | 7.34+0.048 | 0.000 |
| Acute kidney injury | 100% | 50% | 0.003 |
| Oliguria | 71.4% | 0% | 0.000 |
| Admission to intensive care | 64.2% | 6.3% | 0.001 |
| Deaths | 14.3% (n=2) | 0% | — |
| Diuretics | 69.2% | 31.3% | 0.048 |
From a therapeutic point of view (Table 1), more patients requiring HD were taking diuretics (69.2 vs 31.3%; p=0.048), with no differences found regarding treatment with ACE inhibitors or ARBs or the dose of metformin.
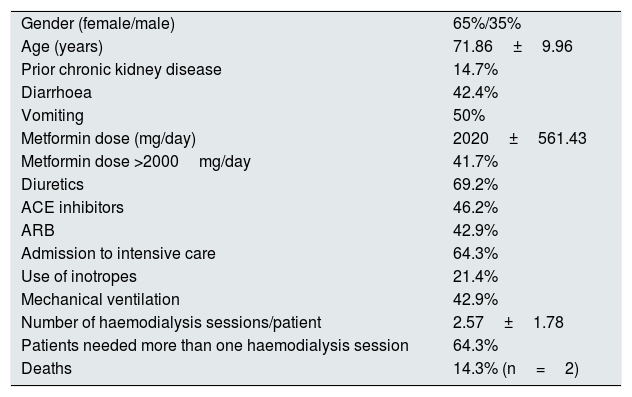
Table 2 shows the characteristics of the group of patients who received dialysis.
Characteristics of patients taking metformin with lactic acid above 2mmol/l and requiring haemodialysis.
| Gender (female/male) | 65%/35% |
| Age (years) | 71.86±9.96 |
| Prior chronic kidney disease | 14.7% |
| Diarrhoea | 42.4% |
| Vomiting | 50% |
| Metformin dose (mg/day) | 2020±561.43 |
| Metformin dose >2000mg/day | 41.7% |
| Diuretics | 69.2% |
| ACE inhibitors | 46.2% |
| ARB | 42.9% |
| Admission to intensive care | 64.3% |
| Use of inotropes | 21.4% |
| Mechanical ventilation | 42.9% |
| Number of haemodialysis sessions/patient | 2.57±1.78 |
| Patients needed more than one haemodialysis session | 64.3% |
| Deaths | 14.3% (n=2) |
ACE inhibitor: angiotensin-converting enzyme inhibitor; ARB: angiotensin II receptor blocker.
As both metformin and loop diuretics are removed by active tubular secretion, we analysed whether or not the pharmacological interaction between them might be at this level. Active secretion of metformin is carried out through the hOCT2 (human organic cation transporter 2) (basolateral)/hMATE1/2-K (human multi-drug and toxin extrusion proteins 1 and 2-K) (apical) pathway,5,6 which is the cationic organic acid secretory pathway. However, the active tubular secretion of loop diuretics takes place through hOAT1 (human organic anion transporter 1) and hOAT35 (basolateral)/hMATE2/4-K (apical), which is the secretory pathway for anionic organic acids. Thus, in principle and from a theoretical point of view, there would not appear to be any interaction between metformin and loop diuretics at the level of active tubular secretion of organic acids (hOCT or hOAT). It remains to be determined whether the interaction could occur at the level of the hMATE1 or hMATE2 transporters located at the apical level. In fact, furosemide has been reported to increase the concentrations of metformin in plasma and blood by 22%, without any significant change in renal clearance of metformin being observed if renal function is normal.
At the same time, it could be hypothesised that diuretics would contribute to greater renal hypoperfusion in acute kidney injury associated with lactic acidosis secondary to metformin, which tends to present with vomiting, diarrhoea and hypotension, and that is perhaps why it is these patients who most frequently require HD.
In conclusion, the data presented suggest that in patients who need diuretics as part of their treatment, we must be careful about prescribing metformin and particularly with the dose, as it will probably be these patients who, in the event of developing high blood lactic acid levels, are most likely to need HD and admission to ICU.
Please cite this article as: Viera YR, et al. Metformina y diuréticos. Nefrologia. 2019;39:557–558.