Gaucher disease (GD), is an autosomal recessive lysosomal storage disease that is due to mutations in the glucocerebrosidase (GC) gene, with a prevalence of 1/57,000 to 1/75,000 births worldwide1 and significantly more common among the Ashkenazi Jewish heritage.2 GD is categorized into three clinical types4 and the clinical manifestations result from the accumulation of the lipid-laden macrophages in the spleen, liver, bone, bone marrow,3 leading to impairment of central nervous system in the most severe cases.4
Although several reports are available related to the risk of GD patients developing other diseases like Parkinson's disease5 and increased rates of malignancies, particularly hematologic,6 systemic lupus erythematous (SLE) has not been described in association with GD.
We report a case of a 32-year-old Caucasian woman diagnosed with GD type 1 at 17 years-old. She had a grandmother with GD, an uncle with SLE and a cousin with rheumatoid arthritis. There is no known Jewish heritage in her family. She was medicated with velaglucerase.
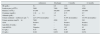
With 30 years old, the patient developed malar-rash and chest eczema, associated with sun exposure. One year after she noticed worsening asthenia, anorexia, nausea, hair loss, myalgias, bilateral gonalgia, oral ulcers, Raynaud syndrome and arterial hypertension (TA 140/90mmHg). The patient was referred to the nephrology unit with peripheral edema and the laboratory investigation showed parameters of ferropenic anemia (without signs of hemolysis), leukopenia, thrombocytopenia, elevated seric creatinine, hypoalbuminemia, active urinary sediment and nephrotic-range proteinuria observed in the 24h urine sample (Table 1). The immune assays revealed positive antinuclear antibodies (ANA) and anti-Sjögren's-syndrome-related antigen A, elevated immunoglobulin (Ig) G (20.7g/L) and IgA (4.64g/L), circulating immunocomplexes (>100μgEq/mL) and low serum complement (C3 0.16g/L, C4 0.021g/L, C1q 0.208g/L). The complementary immunologic and serologic study was negative. Renal and abdominal ultrasounds showed normal sized kidneys, increased cortical echogenicity with maintained differentiation and mild/moderate homogeneous hepatosplenomegaly. Echocardiogram revealed thickened pericardium and nuclear magnetic resonance of the inferior members showed bone alterations and moderate intra-articular left knee and mild right knee effusion.
Laboratory parameters.
| Admission | Discharge | 6 months | 12 months | |
|---|---|---|---|---|
| Hb (g/dL) | 9.1 | 8.9 | 13.6 | 13.2 |
| Leukcocytes (×109/L) | 2900 | 7400 | 5900 | 4500 |
| Platelets (×109/L) | 87,000 | 168,000 | 237,000 | 367,000 |
| Creatinine (mg/dL) | 1.38→2.1 | 1.5 | 0.73 | 0.7 |
| Albumin (g/dL) | 2.1 | 3.1 | 4.1 | 4.2 |
| Urinary sediment – erythrocyts (μL−1) | 225 (15% dysmorphic) | – | 8 (8% dysmorphic) | 10 (4% dysmorphic) |
| Urinary proteins (mg/24h) | 7600 | 4500 | 341 | 283 |
| ANA | Positive | – | Positive | Positive |
| Anti-SSA (UA/mL) | 786 | – | Positive | Positive |
| Anti-dsDNA | Negative | – | 182 | 83 |
| C3 (g/L) | 0.16 | 0.42 | 0.78 | 0.90 |
| C4 (g/L) | 0.021 | 0.052 | 0.085 | 0.074 |
ANA, antinuclear antibodies; anti-SSA, anti-Sjögren's-syndrome-related antigen A; anti-dsDNA, anti-double stranded DNA; C3, complement 3; C4, complement 4.
Kidney biopsy established the diagnosis of class IV-G lupus nephritis (LN) and the treatment according to KDIGO (Kidney Disease: Improving Global Outcomes) guideline7 was started. Hydroxychloroquine was redrawn due to gastric intolerance. She was discharged 1 month after admission with serum creatinine 1.5mg/dL, proteinuria 4500mg observed in the 24h urine sample (mg/24h), complement levels arose and albuminemia was at the normal range (Table 1). Six months after discharge the patient is clinically stable, with normal renal function, proteinuria of 341mg/24h and an amelioration of complement. Anti-double stranded DNA was positive for the first time 6 months after discharge (182U/mL) and decreased to 83U/mL in the following 6 months (Table 1).
We describe this case of a patient with GD and SLE simultaneously with the purpose of highlighting a possible immunologic proximity between these two diseases. Although the presence of renal pathology in GD is rather rare, it consists of varying degrees of proteinuria with or without renal insufficiency and it has been described in some patients associated with the accumulation of GC in form of Gaucher bodies in glomerular, mesangial, endothelial and interstitial cells of the kidney.8 It has been suggested that progressive accumulation of GC may trigger macrophage activation leading to chronic stimulation of the immune system.9 Increasing clinical evidence suggests that the pathophysiology of classic GD is more complex and involves system-wide dysfunction of cell types other than macrophages.10 Therefore, the immunological disturbances that occur in GD may function as a trigger to the development of SLE, bringing up the already existing doubt that the defects in lipid metabolism could contribute to the development of autoimmunity. In this particular case, clinical and laboratory results could led to a diagnosis of SLE: presence of 4 or more criteria, at least one clinical and one laboratorial Systemic Lupus International Collaborating Clinic (SLICC) criteria. However, and besides the clinical manifestations of malar rash associated with sun exposure, other like arthralgia, pancytopenia and hepatosplenomegaly were easily confounded with GD manifestations and the SLE diagnosis was not achieved until the renal manifestations occurred. The kidney biopsy revealing LN with positive ANA was preponderant to the diagnosis of SLE, according to SLICC criteria. Determining the class of LN was also important to guide the treatment by the histologic subtype, as the clinical presentation may not accurately reflect the severity of the histologic findings, and there was a positive clinical and laboratorial response.
However, the relationship between GD and SLE is not yet established. The involvement of immune cells has been implicated, but the underlying molecular defect is poorly understood. Further studies are necessary to highlight the possible immunologic proximity between these two rare conditions.
DeclarationInformed consent to publish individual data was obtained from the patient.
Conflict of interestThe authors declare no conflict of interest.