La estenosis del cayado o arco de la vena cefálica (EAC) es un tipo peculiar de estenosis del acceso vascular para hemodiálisis. Por ejemplo, y a diferencia de los restantes casos de estenosis, la etiopatogenia de la EAC no está totalmente esclarecida y su prevalencia parece ser inferior en el enfermo diabético. Presentamos tres casos de EAC diagnosticados en nuestra Unidad de Hemodiálisis mediante la aplicación de un programa de monitorización del flujo sanguíneo del acceso vascular utilizando el método Delta-H. Se revisa la prevalencia, la etiopatogenia, la relación con la diabetes mellitus y el perfil funcional de este tipo de estenosis. Hasta la fecha, es el primer estudio funcional efectuado sobre la EAC.
INTRODUCTION
Regular vascular access blood flow (QA) testing is the preferred method of monitoring the function of vascular access.1 Since June-2000, we have introduced in our haemodialysis (HD) Unit a programme for early vascular access estenosis detection based on QA values obtained by the Delta-H method.2
In recent years, there has been increasing interest in cephalic arch stenosis (CAS) located at the cephalicaxillary junction.3-8 This type of stenosis presents some characteristics that are different to other kinds of vascular access stenosis.3-5
Furthermore, there is no evidence of any studies previously carried on the functional profile of CAS. The functional profiles of three cases of CAS and a comparative study involving the other cases of stenosis diagnosed in our HD unit are presented here.
PATIENTS AND METHOD
Patients
We monitored 145 vascular accesses in 131 patients over a period of five years by regularly testing the QA of the vascular access.2 The average age of the subjects was 62.6 ± 13.5 years and they underwent dialysis treatment three times a week in the HD Unit of the Nephroplogy Department at Mollet Hospital Private Foundation with two needles through a native arteriovenous fistula AVF (84.1 %) or a graft AVG (15.9%), using double needle for their haemodialysis.
Method
The QAwas determined during HD by the Delta-H method, using the Crit Line III Monitor (ABF-mode; HemaMetrics, United States). This dilution method, described and validated by Yarar et al.,9 is a photometric technique based on the inverse relationship that exists between volaemia and haematocrit (Hct). The QA is determined from changes in Hct after sudden changes in the ultrafiltration rate (from 0.1 to 1.8 l/h) with HD lines in normal and inverted configuration. The changes in Hct are recorded continuously by an optical sensor attached to a blood chamber inserted between the dialyser and the arterial line. The QA was calculated using the following formula:
QA= (max UF - min UF) · rev Hct max / Δ Hct rev - Δ Hct nor
where max UF is the maximum ultrafiltration rate, min UF is the minimum ultrafiltration rate, rev Hct max is the maximum haematocrit measured with reversed lines, Δ Hct rev is the change in arterial haematocrit with lines in the reverse configuration, and Δ Hct nor is the change in arterial haematocrit with lines in the normal configuration.
The QAwas measured at least every four months during the first hour of the HD session, maintaining a constant blood flow from the HD pump (QB) at 300ml/min. Patients remained in the supine position and resting throughout the examination; patients were not allowed to eat and neither perfusion medication nor saline solution were administered while the QA was being measured. Basal QA was calculated as the average of the first two values of QA obtained during two consecutive HD sessions. All cases with an absolute QA below 700ml/min or a temporary reduction in QA above 20% in relation to the basal value were considered test positive [Test (+)] and were referred them for angiography plus subsequent elective vascular access intervention by angioplasty or revision surgery when vascular luminal stenoses >_ 50% were detected. The mean arterial pressure MAP (diastolic arterial pressure + 1/3 pulse pressure) and the Kt/V index (using the second generation Daugirdas formula, the one-compartment model) were established at the same time as QA.
Statistical analysis
The data was analysed using the SPSS program version 12.0 for Windows. Values were expressed as percentages or mean ± standard deviation. The comparative study of continuous variables among subgroups of patients compared in pairs was performed using a T-test for two independent samples and the Mann-Whitney U test. Values of p < 0.05 were considered to be statistically significant.
RESULTS
During the follow-up period, 54 Test (+) cases, affecting 47 vascular accesses, were identified (seven vascular accesses had a Test (+) twice) due to basal QA below 700 ml/min (n = 27) or a temporary reduction in QA of more than 20% from the basal value (n = 27). An angiography was carried out in most cases of Test (+) (87%, 47/54) and, of them, 43 cases (91.5%, 43/47) had significant vascular access stenosis (reduction in the vascular lumen of 80.5 ± 12.9 %); 46.5% (20/43) of cases of stenosis were diagnosed on the basis of a temporary reduction in QA.
Venous stenosis of the vascular access was detected in 28 cases, involving the arterialized vein of AVF or the venous anastomosis of AVG. This stenosis was isolated (n = 27) or predominant over a simultaneous arterial stenosis (n = 1). Of them, 17 cases were diagnosed on the basis of a temporary reduction in QA.
Arterial stenosis of the vascular access was found in 15 cases, involving the feeding artery of AVF or the arterial anastomosis of AVG. This stenosis was isolated (n = 11) or predominant over a simultaneous venous stenosis (n = 4). Of them, only three cases were diagnosed on the basis of a temporary reduction in QA.
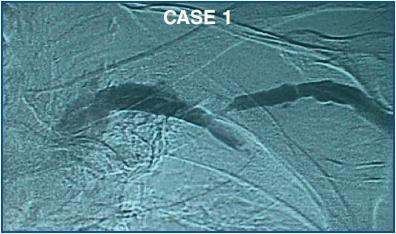
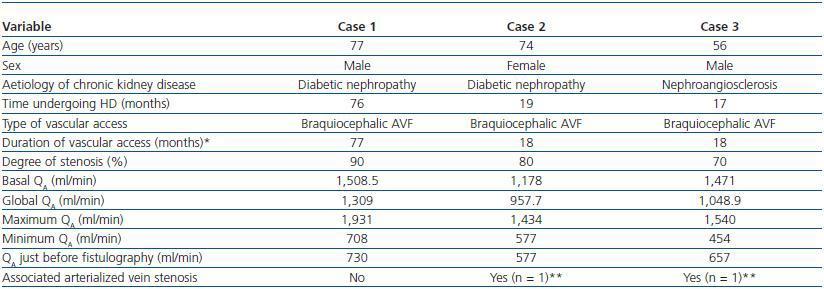
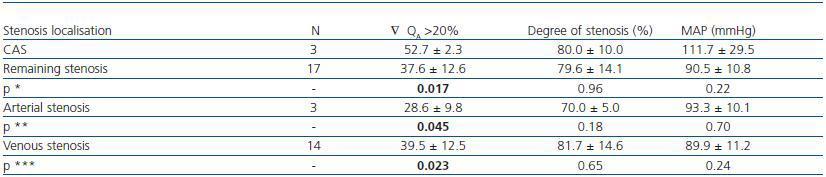
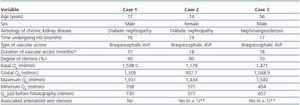
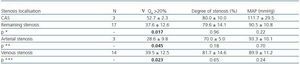
During the study period, three cases of CAS were identified (mean degree 80.0 ± 10.0 %) on the basis of a temporary reduction in QA of 52.7 ± 2.3 % (figure 1). The prevalence of CAS was 11.1, 15 and 17.6%, taking into account the cases of vascular access with Test (+) (n =27), the cases of significant vascular access stenosis (n = 20) and the cases of significant venous stenosis (n = 17), all based on the temporary reduction in QA. Table 1 shows the characteristics of patients and vascular access presenting this type of stenosis. Table 2 shows the comparative study performed between the cases of CAS (n = 3) and: the remaining cases of stenosis (n = 17), the cases of arterial stenosis (n = 3) and the remaining cases of venous stenosis (n = 14), in relation to the temporary reduction in QA, the degree of stenosis and the MAP.
As we can see in table 2, CAS shows a different functional behavior in comparison with the rest of cases of stenosis: despite a similar degree of stenosis, the temporary reduction in QA is significantly greater in the cases of CAS. This functional disparity is not secondary to differences in MAP values.
DISCUSSION
The prevalence of CAS varies according to the different published series. In relation to the total number of dysfunctional AVF, the prevalence of this type of stenosis ranges between 4.25 and 64%.4-7,10,11 The lowest prevalence (4.25%) was found in a recent study carried out by Nam et al., involving 1,623 patients with AVF treated using angioplasty.7 In the retropective study carried out by Rajan et al. (n = 177) and in the prospective study carried out by Jaberi et al. (n = 58) on dysfunctional AVF, the prevalence of CAS was 14.7 and 31%, respectively.5,6 The highest prevalence of CAS at 64%4 was described in the retrospective study by Hammes et al., which involved 127 patients who at least underwent one AVF venogram.
Although the aetiopathogenesis of CAS is not completely clear, all the investigators agree that the presence of a braquiocephalic AVF is the most important predisposing factor.3,5,6 In this study, the three patients with CAS were receiving haemodialysis via a braquiocephalic AVF. In the retrospective study by Rajan et al., involving 177 patients with dysfunctional AVF, the prevalence of CAS was significantly higher for humerocepahlic AVF than for radiocephalic AVF (39 vs. 2%).6 In the prospective and observational series by Javeri et al., involving 58 patients who underwent fistulography, almost all patients with CAS had a braquiocephalic AVF (94%) as compared to the rest of the patients (70%) (p = 0.046).5
Two of the three patients with CAS in this study had diabetic nephropathy and therefore, we cannot confirm the inverse relationship that has been described between this type of stenosis and the presence of diabetes mellitus.4,5 In the aforementioned study by Javeri et al., the prevalence of diabetes was significantly lower in patients with CAS (17 vs. 48%, p = 0.03) and in the series by Hammes et al., the prevalence of CAS was also significant lower in diabetic patients as compared to the rest of the patients.4
The funcional behavior of CAS seems to be different to that of other stenoses. In this study, the temporary drop in QAis significantly higher in cases of CAS in comparison to stenosis at other locations, despite presenting a similar degree of vascular lumen reduction and similar MAP values. An explanation for this functional difference, yet to be confirmed and only speculation at this stage, could be the proximal localisation of this segment of the cephalic vein. This functional disparity, if it is confirmed in further studies, could explain the increase in the prevalence of cases of thrombosis secondary to CAS that some authors have described.4
To sum up, CAS is a unique type of stenosis. If the results of this study are confirmed, then CAS has a functional profile that may be different to that of stenoses at other locations. To date, this is the first functional study on this type of stenosis that has been carried out.
Figure 1.
Table 1. Characteristics of the patients and AVF presenting CAS
Table 2. Comparative study between CAS and the remaining cases of stenosis. The MAP value was obtained
together with the QA value just before the fistulography.