Objetivo: Determinar si la utilización de sueros hipotónicos supone un riesgo en la aparición de hiponatremia iatrogénica en los niños hospitalizados por gastroenteritis aguda (GEA). Pacientes y método: Estudio prospectivo realizado con 205 pacientes de edades comprendidas entre 1 y 28 meses e ingresados con diagnóstico de deshidratación leve o moderada por GEA para recibir sueroterapia en la sección de lactantes de un hospital pediátrico de Madrid (España). El grado de deshidratación inicial se estimó con mediciones clínicas estándar. El suero administrado fue glucosalino 0,3 % en 198 casos y en los 7 casos restantes, todos con hipernatremia inicial, se administró suero glucohiposalino 0,2 %. Se analizó la respuesta a los líquidos intravenosos según si el niño se hallaba normo, hipo o hipernatrémico antes de iniciar el tratamiento. Las cifras de sodio en sangre y la excreción fraccional de sodio (EFNa) se consideraron como medidas de resultado. Resultados: Los 205 pacientes incluidos en el estudio se distribuyeron en tres grupos según el resultado inicial de la natremia. En 37 casos se detectó hiponatremia (18,04 %), en 133 niños isonatremia (64,87 %) y en 35 niños hipernatremia (17,07 %). Después de administrar soluciones hipotónicas encontramos en todos los grupos diferencia significativa entre el sodio sérico inicial y el final; en el grupo con hiponatremia el sodio subió y en los grupos con iso e hipernatremia el sodio descendió ligeramente. Se evidenció correlación significativa entre la EFNa y la evolución de la natremia (Na sérico inicial – Na sérico final). No se detectó ningún caso de hiponatremia posinfusión y tampoco se encontró correlación entre el agua libre administrada y la evolución de la natremia. Conclusiones: En lactantes con funcionamiento renal normal no se ha encontrado hiponatremia como resultado de la administración de sueros hiposalinos intravenosos, hallándose diferencias significativas en la EFNa que indican el ajuste renal de la natremia.
Objective: The purpose of this study is to analyse whether the use of hypotonic fluids increases the risk of iatrogenic hyponatraemia in children hospitalised with acute gastroenteritis (AGE). Patients and methods: Prospective study carried out on 205 patients with ages ranging from 1 to 28 months and admitted with a diagnosis of mild or moderate dehydration due to AGE and treated with intravenous hypotonic fluids in a paediatric department in Madrid (Spain). The degree of dehydration at presentation was estimated using standard clinical measures. 198 children received 0.3 % glucosaline solution and in 7 patients, with baseline hypernatraemia, 0.2 % gluco-hyposaline solution was administered. We analysed the results according to whether children were hyponatraemic, normonatraemic or hypernatraemic at presentation. The blood and urine samples were analysed and the concentration of sodium and fractional sodium excretion (EFNa) before and after intervention were considered as outcome measures. Results: The 205 patients included in the study were distributed in 3 groups according to the baseline natraemia results. In 37 cases we detected hyponatraemia (18.04%), in 133 cases isonatraemia (64.87%) and in 35 children hypernatraemia (17.07%). After administering hypotonic fluids we detected a significant difference between initial and final natraemia in all groups; in the group with hyponatraemia, sodium increased and in the groups with iso and hypernatraemia, sodium slightly decreased. A significant correlation between the EFNa and the evolution of natraemia was found. No cases of hyponatraemia post-infusion were seen and there was no correlation between free water administered and natraemia evolution. Conclusions: Results show that the use of hypotonic fluids does not increase the risk of hospital acquired hyponatraemia in hospitalised children with normal renal function. Our children with gastroenteritis did not develop hyponatraemia even though they were all treated with hypotonic intravenous solutions.
INTRODUCTION
Acute gastroenteritis (AGE) is one of the most frequent medical pathologies in the first years of life and it can lead to dehydration that requires the child’s hospitalisation and the subsequent use of parenteral rehydration solutions. An imbalance between the intake and loss of free water or serum sodium can occur in AGE which can cause hyponatraemia, in other words, a serum sodium level <135 mEq/l1. Ever since Holliday and Segar initiated a parenteral rehydration standard in 1957 that continues today, it is frequent to use hypotonic fluid in the intravenous correction of water deficit in children with AGE2. Furthermore, in 1957, Schwartz published the first case of a metabolic disorder in which the anti-diuretic hormone (ADH) was released by non-physiological stimuli, which would cause the retention of electrolyte-free water followed by a high sodium concentration in the urine with resulting hyponatraemia3. When a loss of intravascular fluid occurs due to dehydration, ADH is released, which forces the kidneys to retain water even if suffering from hyponatraemia, since the signalling for volaemic compensation takes priority over the natraemia control mechanisms. Nausea, vomiting and dehydration make up the non-osmotic stimuli for ADH secretion and are present in AGE4. Serious secondary effects from the use of hypotonic fluids or from perfusion rhythm were documented, since they can cause dilution hyponatraemia with the risk of neurological repercussions of variable severity5.
At present, higher levels of NaCl in hydration solutions are recommended to prevent hyponatraemia, but there is the possibility that these recommendations are not appropriate in infants6.
Most electrolyte imbalances occur in the hospital and among them, hyponatraemia is the most frequent. Children have a particularly high risk of secondary hyponatraemia and prognosis is worse than in later life.
This study aims to determine whether the use of hypotonic fluids involves a risk for iatrogenic hyponatraemic in children hospitalised due to AGE and to analyse whether initial natraemia can predict the risk of developing iatrogenic hyponatraemia in our series.
PATIENTS AND METHOD
This is a prospective study involving 205 patients aged between 1 and 28 months, of which 23 were younger than 6 months. Patients were admitted with dehydration due to AGE and/or intractable vomiting in order to receive fluid therapy in the infant department of the Niño Jesus Children’s Hospital, Madrid, from January to December 2010.
The reasons recorded for admittance and subsequent parenteral rehydration were the combination of mild or moderate dehydration and/or continuous vomiting, as well as insufficient intake of oral liquid during stay in the emergency department. The initial degree of initial dehydration was estimated using standard clinical measurements, according to the Gorelick score7.
55 patients presented mild dehydration, and the remaining 155 patients were moderately dehydrated.
19 children were excluded from the study, the exclusion criteria being: nephropathy, heart disease, chronic diseases, hypothalamus-hypophysis pathology and also admittance to the intensive care unit due to the seriousness of the process. Informed consent was obtained and the hospital’s ethical committee approved the study.
In order to determine whether baseline plasma sodium was a subsequent risk indicator for dilution hyponatraemia, response to intravenous fluids was analysed based on three groups of baseline natraemia: normonatraemia, hyponatraemia and hypernatraemia.
Hyponatraemia was defined as a sodium serum level <135mmol/l; normonatraemia as 135-145mmol/l; and hypernatraemia >145mmol/l.
A separate analysis of the results was carried out in accordance with the classification of hyponatraemia, isonatraemia or initial hypernatraemia.
Urine and blood samples were taken to determine sodium levels and osmolality before starting fluid therapy and before beginning oral feeding and/or administering any oral liquid. The urine sample was taken as close to the blood sample as possible.
Fractional sodium excretion represents the percentage of sodium filtered that is finally excreted and is calculated in all patients using the formula: sodium in urine x creatinine in blood x 100/sodium in blood x creatinine in urine8. Free water administered in ml / kg of weight and ml/hour was also analysed. The difference between the volume of fluid infused with saline solution and the volume of fluid infused with isotonic saline solution was calculated in order to administer the same amount of sodium chloride; all calculated in ml/hour divided by the child’s weight (kg)9.
The solutions administered were 0.3 % glucosaline (0.3 % saline solution with 5 % glucose) in 198 cases and 0.2 % gluco-hyposaline (0.2 % saline solution with 5 % glucose) in the 7 remaining cases, all with initial hypernatraemia. Fifteen patients previously needed expansion with saline solution. Fluid infusion included baseline requirements in addition to estimated deficit.
Administration of fluids and/or oral solids restarted when vomiting eased.
The statistical analysis was carried out using SPSS 15.0 commercial software. Basic data was expressed in means and standard deviations for quantitative variables, and in numbers and percentage for qualitative variables. 95 % confidence intervals (95 % CI) were calculated. Comparisons between quantitative variables were made using the Mann-Whitney test after verifying that they were not adjusted to a normal distribution (Kolmogorov-Smirnov test). If distribution was normal, the Student’s t-test was applied. The Pearson correlation coefficients were calculated. Values of P<.05 were considered to be statistically significant.
RESULTS
205 was the total number of patients admitted with a diagnosis of mild/moderate dehydration caused by AGE in 2010 and who were included in the study; 117 patients were boys (57.03 %) and the remainder, girls. The degree of dehydration was mild in 55 cases (26.82 %) and moderate in 150 (73.17 %).
198 patients received 0.3 % saline solution (0.3 % saline with 5 % glucose) and 7 patients, whose analysis showed baseline hypernatraemia, received 0.2 % gluco-hyposaline solution (0.2 % saline with 5 % glucose). Expansion with saline solution was previously required in 15 patients.
The age range of the children was 1 to 28 months; average age was 11.52 months and standard deviation (SD) 5.77. Twenty-three patients (11.21 %) were younger than 6 months. Mean weight of the patients was 8.44kg, 1.85SD. Mean infused volume/kg/hour was 5.51, 1.3SD. The incidence of baseline hyponatraemia in these patients was 18.04 %.
In the initial analysis, we separated the patients into three groups according to baseline natraemia: 37 hyponatraemic patients (18.04 %), 133 normonatraemic patients (64.87 %) and 35 hypernatraemic cases (17.07 %).
Mean baseline glycaemia was 99.42mg/dl (18.61SD), with range 40-166mg/dl, and values <70mg/dl were found in 45 children (21.95 %).
In the first group, after administering 0.3 % saline solution, serum sodium increased from 131.9mEq/l (2.07SD) to 135.6mEq/l (2.54SD). Serum sodium slowly reduced in the second group, without resulting in hyponatraemia, from 139.18 (2.9SD) to 137.92 (2.5SD); and likewise reduced in the third group from 150.17 (4.2SD) to 142.02mEq/l (4.3SD). There were no cases of hyponatraemia post-infusion. Blood and urine tests were performed after an average time of 12.34 hours (95 % CI 11.94-12.56) from the onset of fluid therapy.
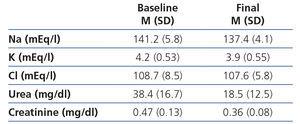
Table 1 shows the results of the biochemical measurements in blood at the time of diagnosis and at the end of treatment, before beginning oral feeding.
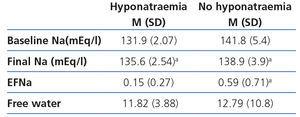
Table 2 shows the evolution of natraemia in all the study’s patients, depending on whether or not they had initial hyponatraemia. An increase of serum sodium was observed in those patients with initial hyponatraemia and these patients had significantly lower fractional sodium excretion compared to those without initial hyponatraemia.
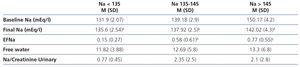
Shown in table 3 are the analytical results obtained in blood and urine after beginning fluid therapy with hypotonic solutions and in accordance with baseline natraemia: hyponatraemia, isonatraemia and hypernatraemia. We found significant difference between baseline and final serum sodium in all groups: sodium increased in the group with hyponatraemia, and slightly decreased in the groups with isonatraemia and hypernatraemia.
The Pearson correlation coefficients between fractional sodium excretion and the analysed variables were: 0.413 with baseline sodium (P=.01), 0.808 with sodium evolution (P=.003) and there was no significance with infused free water (r = 0.028).
DISCUSSION
This study evaluates parenteral treatment with hypotonic saline solutions in mild and moderate dehydration of paediatric patients hospitalised with AGE and the possible link with the iatrogenic development of hyponatraemia, which was not proved in our case.
Despite the recommendation and acceptance of solutions taken orally to rehydrate children with mild or moderate dehydration caused by AGE, it was observed that intravenous fluids were frequently used in developed countries10,11.
Suitable tonicity of the solutions is a subject of controversy, without which a consensus on the type of solution for the most convenient maintenance in hospitalised children would be reached. At the time of assessing and discussing the results of the consulted literature, the studied paediatric pathologies should have been considered12, since the baseline hydrosaline situation of the case of a child with AGE differs to that of a critical patient or that of a child who undergoes surgery. Hydroelectrolytic management in the infant has to be performed cautiously due to the immaturity of the renal function. Newborns have a high percentage of total body water, with a higher percentage of extracellular water and lower intracellular water percentage than adults. This situation changes progressively with age and the percentages of total, intracellular and extracellular water normalise around 6-12 months of life13. The newborn presents glomerular-tubular imbalance and a limited capacity of concentration and dilution of urine. The excreted sodium fraction is inversely proportional to gestational age in the newborn and there is no aldosterone suppression due to sodium load, which would explain the small adaptation of the youngest infants to sodium excess14,15.
In 2007, the National Patient Safety Foundation16 in the United States recommended changing parenteral saline solutions from 0.18 % to 0.45 % to prevent hyponatraemia in infancy. However, Coulthard17 warns about the risk of developing hypernatraemia with the previous standard and considers hypotonic solutions as more physiological at the time of replacing the losses. Halberthal et al. recommend the use of hypotonic solutions in patients with serum sodium >140mmol/l18. Curiously, the publications by Moritz18, which group various studies on the subject from 2004 to 2011, indicate that the administration of hypotonic fluids is dangerous and anti-physiological19,20.
Our results coincide with those presented in 2006 by Sánchez Bayle at al.21 The incidence of hyponatraemia at the time of diagnosis was 18.04 % in our study and there were no cases of iatrogenic hyponatraemia. The high incidence of baseline hypoglycaemia in our patients leads us to think that the use of a glucose-free solution would aggravate baseline hypoglycaemia, with consequential risks. As regards fractional sodium excretion, our results show that it is significantly lower in children with baseline hyponatraemia, which seems to demonstrate that renal management of sodium is the essential physiological mechanism for regulating and correcting natraemia.
Neville et al.22,23 report an baseline hyponatraemia incidence of 36 %, they recommend the use of 0.9 % saline solution in the case of AGE and refer to the non-osmotic stimuli present in patients with AGE which could be involved in iatrogenic hyponatraemia. Holliday and Segar24 did not consider that hospitalised patients were submitted to numerous non-osmotic stimuli for ADH secretion and considered that secondary hyponatraemia at the rehydration standard proposed by them in 1957 would be due to excessive administration of fluids. The results obtained by Hoor et al.9 in their study using a sample of 1586 children concluded that hyponatraemia was due to incorrect treatment in which more fluids were administered than necessary. It is important to remember that natraemia does not precisely reflect body sodium content and that rather than the reduction of serum sodium, it more precisely reflects the increase of total body water. True hyponatraemia is associated with serum hypo-osmolality; therefore it is necessary to understand plasma osmolality and also urine osmolality to determine whether there is deterioration in the capacity to excrete free water. However, Kannan et al.25 report 14.3 % iatrogenic hyponatraemia after administering 0.18 % saline solution, but patients with AGE were not included in their study. Armon et al.26 consider that using 0.9 % solutions would not be protective. Caramelo et al.27,28 do not find association between more hypotonic solutions and hyponatraemia in their study carried out on operated adult patients and they emphasise the importance of renal retention of water and the volume of fluid administered as a mechanism to consider in hyponatraemia. Other studies performed using critical patients or patients undergoing surgery have conflicting conclusions29-31.
A limitation of our study is that it was undertaken in one centre and future studies on the subject should be recommended.
As a conclusion and in light of the significant disparity in this field, we point out that it is not possible to accept the conclusion that hyponatraemia is generated with hyposaline maintenance solutions. Considering the high percentage of children with hypoglycaemia, the use of hypo-sodium solutions would protect against this hypoglycaemia, in addition to not inducing hyponatraemia in a healthy kidney.
The monitoring of electrolytes before and during treatment is necessary.
It is important to reconsider the frequent and in many cases, unnecessary use of parenteral pathway in dehydrated patients and those with acceptable oral tolerance and to remember that oral rehydration is key, since it is associated with less secondary effects and significantly reduces hospital stay.
FUNDING
The present study has not received any type of funding.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Initial and final analysis (before starting oral feeding)
Table 2. Comparison of initial and final sodium of each group
Table 3. Fluid therapy according to natraemia