The buttonhole (BH) puncture technique for arteriovenous fistulas is an alternative to the classical staggered puncture.
PurposeWe present 3 years’ results incorporating the BH puncture technique for arteriovenous fistulas in our dialysis unit.
Material and methodsTwenty-two patients were started on BH technique, 15 men and 7 women (mean age: 62 years; SD: 12), with time spent on dialysis when starting the BH technique of 34 months (SD: 34, median: 27, range: 3–136). Seven patients received acenocoumarol and 9 antiplatelet agents. The vascular access median time at the beginning of the technique was 27 months (range: 3–252).
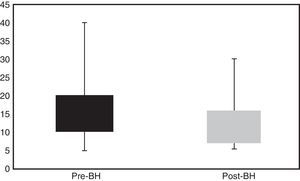
ResultsBetween 5 and 8 consecutive dialysis sessions were necessary to achieve a proper tunnel puncture. No patient suffered major complications. The average time on BH technique until December 2015 was 12 months (SD: 10, median: 9, range: 1–45). By the end of the study, 5 patients were performing self-puncture. Haemostasis times post-dialysis were reduced from 18.6min (SD: 8, prior to the BH technique), to 12.2min (SD: 3 after BH) (p=0.0005).
ConclusionsThe BH technique is an alternative puncture technique for dialysis patients. Self-puncture and reduction in haemostasis time are potential beneficial aspects. A greater diffusion of this technique in the haemodialysis units would allow it to be better applied. A highly motivated nursing staff is key and a necessary condition for its implementation.
La técnica de punción de buttonhole (BH) o de ojal para fístulas arteriovenosas es una alternativa a la punción escalonada clásica.
ObjetivoMostramos la experiencia en nuestra unidad de hemodiálisis tras la incorporación de esta técnica a la práctica clínica diaria.
Material y métodosSe ha aplicado la técnica de BH a 22 pacientes, 15 hombres y 7 mujeres, con una edad media de 62 años (DE: 12), con un tiempo en diálisis en el momento de iniciar la técnica de BH de 34 meses (DE: 34; mediana: 27; rango: 3-136). Siete pacientes recibían acenocumarol y 9 estaban antiagregados. La mediana de tiempo con el acceso vascular al inicio de la técnica de BH fue de 27 meses (rango: 3-252).
ResultadosFueron necesarias entre 5 y 8 sesiones consecutivas de diálisis para la consecución de un correcto túnel de canalización. Ningún paciente presentó complicaciones mayores. El tiempo medio en la técnica de BH fue de 12 meses (DE: 10; mediana: 9; rango: 1-45). Al final del periodo de estudio 5 pacientes realizaban autopunción. El tiempo de hemostasia posdiálisis se redujo de 18,6min (DE: 8) previamente a la técnica de BH a 12,2 (DE: 3) posteriormente a su utilización (p=0,0005).
ConclusionesLa técnica de BH es una alternativa de punción en hemodiálisis. Puede presentar aspectos beneficiosos como la autopunción o la reducción de los tiempos de hemostasia. Una mayor difusión en las unidades de hemodiálisis sería necesaria para mejorar en su aplicación adecuada. El personal de enfermería altamente motivado es clave y condición necesaria para su implantación.
Vascular access puncture is one of the most critical aspects in haemodialysis patients (HD).1 The rope-ladder puncture2 is the most accepted technique and is recommended by guidelines. However, many times this technique cannot be applied, for different reasons, poor development of the vascular access, limited length of the vessel, presence of aneurisms or physical limitations in the anatomical condition of the patient; then, area punctures are necessary. The buttonhole (BH) puncture technique is an alternative to these punctures. This technique was described in 1972 by Dr Twardowski and involves the cannulation of the arterialised vein using blunt needles, at the same angle and at the same site, via a previously formed tunnel.3 Once the dialysis is completed, after the corresponding haemostasia, a scab is left at the puncture site which should be properly removed in the next HD session.4 Several studies have shown that it is possible to improve clotting times, which could help to reduce pain and may also help to maintain vascular access as compared to other techniques.5–8 However, other studies have shown a high incidence of infections, therefore its acceptance has been limited.9–12 Its application is widely established in some countries, especially in some northern European countries and in the USA, but not in Spain, where there are only few centres that use it. To our knowledge, our centre is the first in the Madrid Region to use this technique regularly. Here we are presenting our experience, over 3 years, after its instauration and the maintained used of this technique.
Materials and methodsFrom 2012 to December 2015, all the patients who started the BH technique at our centre were evaluated. A retrospective study was carried out to analyse the characteristics of the patients, clinical evolution, the expected benefits of the technique and the possible drawbacks of its implementation.
The inclusion criteria for the BH technique were patients over the age of 18 years presenting with one of the following circumstances: patients with the option of home HD, patients with autologous arteriovenous fistulas (AVFs) that are difficult to puncture or with multiple unsuccessful punctures, or patients with significant pain or unable to deal with the fear for AVF puncture. Also included, were those who expressed an interest in the technique and had no contraindications. All patients were verbally informed with additional written information if requested.
The exclusion criteria were those with a prosthetic device for vascular access or those that did not came to the unit for prolonged periods of time and were incapable of self-cannulation since it could imply that they were treated at another centre not familiar with the BH technique.
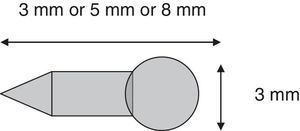
Buttonhole techniqueThe buttonhole technique involves the creation of a subcutaneous tunnel as a permanent and invariable route of access to the AVF; once it is created a blunt needle can be inserted. The first puncture must be made using a conventional needle. The area should be selected, considering that the 2 puncture areas should be at least 6cm apart and, avoiding aneurysmal areas. Once the first HD session is finished, both needles are removed, and the site is left to form a clot without any haemostatic dressing. After the correct coagulation as been completed the area it is sterilised with aqueous chlorhexidine. After leaving it for a few minutes f to have an antiseptic effect, a 5mm-long polycarbonate device, similar to a peg, is used at the puncture site to stabilise the tunnel (BioHole® Nipro Corp)13,14 (Fig. 1). The BioHole is inserted using a sterile technique and covered with a transparent dressing. The BioHole remains in place until the next session. At the next session, the transparent dressing is removed without removing the BioHole, and it is sterilised with aqueous chlorhexidine, prior to and after manipulation (double asepsia). Once the BioHole is removed with the aid of tweezers and using sterile technique, the vascular access will be cannulated using a blunt needle once the tunnel is visible. The stabilisation BioHole should be inserted in 5–6 sessions, always using the same technique and by the same previously trained nurse.15
Buttonhole handling techniqueOnce the tunnel is established, the puncture is made using a blunt needle. The first step is to remove the scab that is formed at the access site after clotting. Again using an aseptic technique, and ensuring that the area is disinfected both before and after removal of the scab (double asepsis). Next the site is cannulated using the blunt needle, following the path of the previously formed tunnel. Clotting should be helped manually, without using any type of haemostatic dressing, in order to minimise the risks of infection and reduce the possibility of the haemostatic dressing plugging the tunnel.
Organisation of nursing staffOne single nurse is responsible for creating the BH and he/she will have to adjust his/her work schedule until the BH is correctly formed. After successful completion, the rest of the staff, who has been previously trained in this technique, is informed of the location and peculiarities of the specific BH. From then on, BH punctures can be performed by any member of the nursing staff.
Statistical analysisThe results are expressed as the mean and standard deviation; the median and range are also shown when required. At the start and end of the study, means were compared using the Student's t test for parametric data. A p-value <0.05 was considered to be significant.
ResultsOver this 3y period 22 patients were evaluated. Table 1 describes their baseline characteristics. There were 15 male and 7 female patients with a mean age of 62 years. 9 patients received antiaggregation therapy and 7 were anticoagulated with acenocoumarol. Mean time on HD at the start of BH was 34 months (SD: 34; range: 3–136 months).
Baseline data.
| % (n) | n=22 |
|---|---|
| Mean age (years) | 62±12 |
| Male/female | 15/7 |
| Aetiology of kidney disease | |
| Diabetes mellitus | 50 (11) |
| Malignant HTN | 9 (2) |
| Glomerulopathy | 23 (5) |
| Polycystic kidney | 4 (1) |
| Bilateral nephrectomy | 4 (1) |
| Unknown | 9 (2) |
| HTN | 100 (22) |
| Diabetes | 68 (15) |
| Heart disease | 77 (17) |
| Oral anticoagulation therapy | 32 (7) |
| Antiplatelet agents | 41 (9) |
| Type of haemodialysis | |
| High-flux HD (6 sessions/week)a | 4 (1) |
| High-flux HD (5 sessions/week) | 4 (1) |
| High-flux HD (4 sessions/week) | 14 (3) |
| High-flux HD (3 sessions/week) | 68 (15) |
| High-flux HD (2 sessions/week) | 9 (2) |
| Previous vascular access | 32 (7) |
| Previous tunnelled catheter | 45 (10) |
| Analytics | |
| Mean haemoglobin (g/dL) | 11.3±1 |
| Mean haematocrit (%) | 35±4 |
| Mean platelets (103/μL) | 185±62 |
The types of vascular access and the puncture technique prior to the BH technique are shown in Table 2. The most common AVF was left radiocephalic AVF in 9 patients, followed by left humero-cephalic AVF in 8 patients, the other AVFs were: 2 right radiocephalic AVFs, 2 left humero-basilic AVFs and one right humero-cephalic AVF. The technique of the previous puncture was the rope-ladder in 10 cases, the area technique in 6 patients and in 6 other cases a combination of the area and rope-ladder techniques were used. Mean time of vascular access before the technique was changed was 41 months (SD: 55; median: 26; range: 3–252).
Characteristics of vascular access and status at the end of the study.
| Patient No. | Type of AVF | Type of puncture prior to BH | Months of AVF at the start of BH | Months on RRT at the start of BH | Time with BH (months) | Status of the BH in Dec 2015 |
|---|---|---|---|---|---|---|
| 1 | LRC | Rope-ladder | 252 | 120 | 45 | Functioning |
| 2 | RHC | Mixed | 40 | 63 | 26 | Kidney transplant |
| 3 | LRC | Rope-ladder | 20 | 29 | 26 | Functioning |
| 4 | LRC | Rope-ladder | 45 | 34 | 22 | Functioning |
| 5 | LHC | Rope-ladder | 31 | 35 | 22 | Kidney transplant |
| 6 | LHC | Mixed | 8 | 15 | 22 | Functioning |
| 7 | LRC | Rope-ladder | 20 | 16 | 5 | Death (cerebral haemorrhage) |
| 8 | LHC | Rope-ladder | 8 | 3 | 8 | Kidney transplant |
| 9 | LHC | Area | 23 | 17 | 16 | Not functioning (thrombosis of the AVF) |
| 10 | RRC | Rope-ladder | 3 | 59 | 4 | Kidney transplant |
| 11 | LHC | Area | 30 | 13 | 12 | Functioning |
| 12 | LHC | Rope-ladder | 17 | 29 | 13 | Functioning |
| 13 | LRC | Area | 40 | 45 | 10 | Functioning |
| 14 | LRC | Mixed | 45 | 42 | 9 | Functioning |
| 15 | LHB | Area | 29 | 29 | 9 | Functioning |
| 16 | LRC | Mixed | 22 | 19 | 8 | Functioning |
| 17 | LRC | Rope-ladder | 23 | 25 | 6 | Kidney transplant |
| 18 | LRC | Area | 11 | 13 | 9 | Functioning |
| 19 | LHC | Mixed | 42 | 7 | 0 | Abandonment of BH (suspected infection) |
| 20 | LHB | Area | 40 | 6 | 1 | Abandonment of BH (failure of BH) |
| 22 | LHC | Rope-ladder | 15 | 5 | 0 | Kidney transplant |
| 22 | RRC | Mixed | 148 | 136 | 2 | Functioning |
BH: buttonhole; AVF: arteriovenous fistula; LHB: left humero-basilic; RHC: right humero-cephalic; LHC: left humero-cephalic; mixed: combination of rope-ladder and area; RRC: right radiocephalic; LRC: left radiocephalic; RRT: Renal replacement therapy.
Of the 22 BHs performed at the unit, 12 continued to function as of December 2015. The main cause of BH loss was kidney transplantation in 6 patients. One case of BH loss was due to death, caused by a cerebral haemorrhage, in a diabetic patient with hypertension. In one case it was due to vascular access thrombosis and in 2 cases the BH technique had to be abandoned. One of those cases was due to suspected infection of the tunnel (despite negative control culture), as the patient was immunosuppressed, within the context of a functioning liver transplant and, the other case was due to difficulty in obtaining access to a very deep humero-basilic AVF as the patient was significantly obese. This particular patient subsequently required superficialisation of the basilic vein. At the end of the study, the mean time with BH was 12 months for all patients (SD: 11; median: 9). The mean BH time, for those who maintained the BH technique at the end of the study, was 15 months (SD: 11). The patient who spent the longest period of time using the BH technique is currently on home HD (patient 1). All the other patients are undergoing a HD programme at the hospital.
InfectionsWe did not observe any bacteraemia that we could be related to a BH infection of the during this follow-up period. A distal tunnel infection was observed in patient 4, which was confirmed by means of a positive culture for Staphylococcus epidermidis. There were no systemic repercussions. After oral antibiotic treatment and removal of BH from said tunnel, a new tunnel was inserted, which continues to be functional and in use to this date. Patient 3 presented with suspected infection with serous exudate: the culture was negative and the BH remained in use.
HaemostasisHaemostasis times were analysed prior to installing the BH in all patients and at, 1, 6 and 12 months after regular use. Mean haemostasis time prior to the BH was 18.6min (SD: 8) and it was significantly reduced to 12.2min (SD: 3) at month 1 (p=0.0005) (Fig. 2). Mean haemostasis time at 6 months was 11.2min (SD: 2; p=0.001; n=16 patients) and at 12 months it was 10.9min, (SD: 4; p=0.05; n=9 patients).
Self-cannulationAt the beginning of the study none of the patients self-cannulated their vascular access. Once the BH was installed, at the end of the study, 5 patients self-cannulated on a regular basis.
Pain managementSurveys were conducted to assess pain, in which 1 indicated no improvement and 10 indicated an absolute improvement compared to the puncture prior to the installation of the BH. The mean response as to whether there had been an improvement from the previous technique was 9.1. The comparison of pain perception before and after installation of the BH (1 – worst pain and 10 – no pain) was 4.7 vs. 8.8 respectively and significantly favouring the BH, (p=0.00001).
Other complicationsOn 9 occasions a new BH tunnel had to be created due to the failure of the previous one. On 2 occasions, after receiving care at other centres, in one case due to the voluntary transfer of the patient and in another case due to surgery. The BH technique could be subsequently maintained after the creation of a new tunnel in all cases.
DiscussionThe majority of observational studies describe that with BH technique there is a reduction of pain, a lower number of punctures, less bruising and a reduced formation of aneurysms.16,17 However, systematic reviews focused on this technique have shown that current evidence does not support these results and that the risk of infection is greater in patients with BH.12,18,19 In spite of that, the BH technique may be a valid alternative in some situations. Area puncture complications are well-known and on many occasions rope-ladder punctures are difficult to achieve.1 We decided to include the BH technique as an additional option of puncture techniques at our centre.
The draw back of BH technique is the higher incidence of infections. The rate of bacteraemia described in previous studies was 0.15–0.6 per 1000 patients/day or 0.05–0.2 per patient/year.5,6,20 The review conducted by Muir et al. put forward evidence for this, though it was conducted on a population on home HD, which could mean less control of asepsis.18 However, the Alberta group's published in 2014 more complete review, covering patients on conventional HD, indicating that the risk of infections was greater, without a clear benefit in other respects. The authors concluded that this did not exclude the use of BH in certain specific situations.19
In our experience of 3 years of follow-up we have not observed any bacteraemia and we have had only one local infection confirmed by culture Similar results were described in the randomised clinical trial conducted by Vaux et al., which included 70 patients on the BH technique. No bacteraemia was observed during the follow-up period and only 2 infections were noted at the puncture site.21 In the Chan et al., 2014 study, found no significant differences in infection between the BH technique and the rope-ladder puncture technique (bacteraemia with BH: 5 [11%] vs. conventional: 3 [8%]; p: 0.62).22 Double asepsis was maintained at our unit and thorough monitoring was carried out by the nursing staff as key considerations for avoiding infections. Although some studies showed a potential benefit with topical mupirocin prophylaxis, this was not applied routinely in our population.23
Incidentally, we observed a single case of thrombosis in our group. Although our study was not designed to compare BH with other techniques, some studies have shown greater survival of vascular access with the BH technique.21 However, recent publications, such as that of MacRae, a randomised clinical trial that included 70 patients with BH, or the aforementioned of Chan et al. study, have not shown such a potential benefit.22,24
One of the aspects assessed in our study is the reduction in clotting time at the end of the HD session, which was significant in our population (Fig. 2). In our study, the fact that 75% of patients received anticoagulation or antiplatelet therapy has made it possible to predetermine our results, as they were patients with a higher risk of bleeding. Grau et al. observed a reduction in haemostasis time with the BH technique, although the sample was very small.8 In turn, in the aforementioned Vaux et al. study, bleeding time with the BH technique vs the conventional technique was also reduced: median 7.9 (6.3–10.4) vs. 9.1min (6.9–11.3) respectively, but without reaching statistical significance.21 However, other studies have not proven a reduction in clotting times and some studies have even observed an increased bleeding time, which determined the abandonment of the BH technique.7,24,25
At the same time, the inclusion of the BH technique has led to 5 patients to perform self-cannulation. Although the results are contradictory, especially in terms of home HD, self-cannulation offers benefits to the patient: increasing their autonomy less anxiety when the professional performing the puncture regularly is changed, as well as reducing the number of puncture attempts.5,18,24 The BH technique could be a way of facilitating the option of self-cannulation.
In terms of pain management, in our experience, changing to the BH technique has benefitted our patients. This is a biased population, which may determine our results. Some observational studies, such as that by Ward et al., have also observed a reduction of up to 81% in pain perception with this technique as compared to conventional techniques; however others, such as the van Loon et al. study, did not observe any differences in pain probably due to the routine use of local anaesthetics in classic punctures (30% use in rope-ladder punctures vs 8% in BH punctures; p<0.001).6,26 In randomised clinical trials differences in pain have not been demonstrated, and some studies have shown even an adverse effect of the BH technique.10,21
Finally, the presence of BH-associated complications, such as the need to change BH tunnels due to problems during cannulation, is not widely described. In our study, it was necessary to change the technique in 2 cases after admission to other centres where the BH was not used. Once the patients returned to our unit, it was necessary to restart the process. In the other 7 cases, the need to change the tunnel, was likely due to a change in professionals and this is despite the organisational efforts of the unit and the nursing staff's commitment. This is an essential aspect for the development of these techniques at our institutions, where in addition to the constant turnover of professionals there is an absence of specific training in the field of HD.
Our study has the usual limitations of an observational study without a control group and with a relatively short follow-up period. The patient selection present significant bias. However, broadening the range of puncture alternatives and improving knowledge of other techniques are relevant aspects of our results. Furthermore, although the follow-up period is not very long and the number of patients is reduced, our experience is the broadest in our community to date.
ConclusionsThe BH technique may be a valid puncture alternative for patients on HD, especially in some situations in which the alternative is area puncture. It may offer some benefits such as facilitating self-cannulation or reducing waiting times at the end of HD sessions. However, to improve this technique, it is necessary both to increase dissemination and to reduce the negative aspects that have been detected, and to have motivated professional nursing staff. It is likely that the frequent turnover of staff, absence of HD specialisation and lack of training in the technique may be resolved with a greater institutional commitment to healthcare professionals and, therefore, to patients.
Conflicts of interestMs Laura Baena has been a lecturer on different courses sponsored by Nipro Corp.
Dr José L. Merino has been a lecturer on different courses sponsored by Nipro Corp.
The other authors declare they have no conflicts of interest.
Nipro Corp. has not taken part in the design, analysis or drafting of this study.
Please cite this article as: Baena L, Merino JL, Bueno B, Martín B, Sánchez V, Caserta L, et al. Instauración de la técnica de buttonhole como alternativa de punción para las fístulas arteriovenosas. Experiencia de un centro en 3 años. Nefrologia. 2017;37:199–205.
Some of the information shown here has been presented as a poster at the 2nd Parc Taulí International Vascular Access Symposium, held in Sabadell on the 7th and 8th April 2016.