Different studies have shown how patients in a haemodialysis programme with native arteriovenous fistulas (nAVF) have a higher patency rate and fewer associated vascular complications.1 However, even though nAVF are the best type of vascular access, according to the latest data from the Registro de Enfermos Renales de Cataluña (RMRC) [Catalonia Registry of Patients with Kidney Disease],2 year on year the rate of use has been reducing (59.8%) and only 39.9% of those who started haemodialysis in 2018 did so with this type of vascular access. Use of the venous catheter as access is therefore an increasing reality related to the older average age of our patients and the coexistence with different cardiopulmonary comorbidity factors (low cardiac output and severe pulmonary hypertension).
The main complications associated with central venous catheters are mechanical dysfunction (fibrin sheath and thrombosis) and endovascular infection. Catheter-related bloodstream infection (CRBSI) is considered the leading cause of hospital admission, at times leading to severe septic complications and requiring removal of the catheter, with the consequent increase in related morbidity and mortality rates.3
Different authors have described that catheters become colonised by microorganisms, which produce a mucopolysaccharide matrix (biofilm) over the surface of the catheter, and this plays a significant role in the development of CRBSI, as it protects the microorganisms from the immune system and different antimicrobial agents.4,5
Currently, advances in the prevention of CRBSI have placed particular emphasis on the use of catheter lock solutions deposited in the lumen of the catheter after each dialysis session aiming to maintain the device patent; this has been shown to be an effective way of preventing infection, possibly by reducing biofilm formation.5 Our group concluded based on previous studies that locking the catheter lumen with an antiseptic solution with taurolidine-heparin significantly reduces not only the rate of bacteraemia and the inflammatory response, but also the formation of adherent biological material.6,7 Recent studies show the superiority of lock solutions with taurolidine in its different combinations compared to the use of 4% citrate alone (lower rate of CRBSI and dysfunction), particularly with the use of the preparation containing urokinase.8,9 However, currently there is little scientific evidence on whether or not there are significant differences between the different formulations containing taurolidine (heparin vs urokinase) and whether the therapeutic change is cost-effective.
The main aim of this research was to analyse whether the systematic lock of the catheter with taurolidine-urokinase (T-U: 4% taurolidine-citrate and 25,000 IU urokinase) during the long interdialytic period produces fewer complications as compared to the conventional regimen of taurolidine-heparin (T-Hep: 4% taurolidine-citrate and 500 IU heparin) in each haemodialysis session.
We conducted an observational, retrospective cohort analysis (2013–2018) in 57 prevalent patients with CKD stage 5D (23 T-Hep and 34 T-U), with a mean age of 66.2±14.5 years (35–93) and 61.4% male. No significant differences were found between subgroups in terms of socio-demographic variables, biochemical parameters or haemodialysis adequacy. During the follow-up period, a total of 25 replacements were performed due to dysfunction, 16 in the T-Hep group and nine in the T-U group; P=.003. A total of two bacteraemia episodes were identified during the follow-up period, one in each group (P=NS).
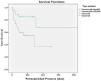
Fig. 1 shows the different rates of primary patency (PP) in each of the study subgroups. The PP in the group locked with T-U was significantly higher, 1105.9±202.9 days (708.1–1503.6) than that of the T-Hep group, 261.5±53 days (157.5–365.4); P=.014. Table 1 shows an analysis of the mean cost-effectiveness during the follow-up period in each of the study subgroups. As can be seen, the average cost was higher in the group with T-U lock, albeit with a lower cost for angiography/radiological procedures due to dysfunction.
Analysis of the economic costs by tunnelled catheter lock subgroup (T-Hep vs T-U).
| Unit price | T-Hep (N=23) | T-U (N=34) | P value |
|---|---|---|---|
| Locka | Є202±5.90 (213−189) | Є400.60±13.80 (426−369) | .000* |
| Urokinaseb | Є2.10±10.10 (48.90–0) | Є2.80±11.60 (48.90–0) | .801 |
| Admission for bacteraemiac | Є150.90±723.90(3,472–0) | Є124±723(4,216–0) | .799 |
| Replaced due to dysfunctiond | Є1000±1266.30(3,800–0) | Є473.50±1093(3,800–0) | .033* |
| Total mean coste | Є1355.10±1343.30(4,003.80–97.50) | Є1001±1564.20(7,926.10–369.20) | .494 |
In the search for new lock solutions, an American study recently published concluded that systematic locking with sodium bicarbonate significantly reduces the rate of thrombosis (0.17 episodes/1000 catheter days vs 4.1 episodes/1000 catheter days; P<.0001) and endovascular bacteraemia (0.17 episodes/1000 catheter days vs 2.6 episodes/1000 catheter days; P=.0004) compared to saline.10 This potential dual beneficial effect of bicarbonate as an antithrombotic and anti-infective agent should therefore be investigated in the future.
According to the results obtained in our study, the use of systematic locking with the combination T-U in the long interdialytic period significantly reduces the number of replacements due to dysfunction, increasing primary patency rates with no additional financial cost. Nevertheless, the present data is preliminar and will need to be correlated with the design of future prospective, randomised studies.
FundingThe authors declare that they have not received funding for this article.