La permeabilidad peritoneal es diferente entre sujetos al inicio de la Diálisis Peritoneal (DP) y puede aumentar con el tiempo en la técnica. Este último fenómeno está condicionado por las peritonitis, la biocompatibilidad de los líquidos de diálisis y el abuso de glucosa como agente osmótico. Objetivo: evaluar si el uso de icodextrina desde el inicio de la DP afecta a la evolución de la permeabilidad peritoneal. Pacientes y métodos: incluimos 56 pacientes incidentes en DP (edad media: 48,3 ± 14; 62,5% varones; 17,9% diabéticos) que utilizan desde el inicio un cambio con icodextrina. Se les realizó una cinética peritoneal basal y cada seis meses, determinando la relación D/P creatinina (D/P cr) y los coeficientes de transferencia de masa de urea (MTC urea) y creatinina (MTC cr). La evolución de los MTC cr en el primer año se comparó con un grupo «histórico» de 249 pacientes que desde el inicio de la DP habían utilizado exclusivamente glucosa. Resultados: la permeabilidad peritoneal determinada por MTC cr, MTC urea y D/P cr descendió durante los primeros 12 meses (11,7 ± 5,7 vs. 8,1 ± 3,1; 23,5 ± 7,3 vs. 18,9 ± 3,8; 0,72 ± 0,09 vs. 0,67 ± 0,08, respectivamente), manteniéndose posteriormente estable. Los pacientes con Alto Transporte (AT) peritoneal basal (cuartil mayor de MTC cr) presentaron una mayor disminución de MTC cr a lo largo del primer año. El descenso del MTC cr al inicio y tras doce meses de DP usando icodextrina fue significativamente mayor (p <0,001) que el obtenido en el grupo «histórico» que sólo usaba glucosa (10,5 ± 5,3 vs. 10,1 ± 4,6). Los pacientes con AT peritoneal basal (cuartil mayor de MTC cr) son los que presentaron una mayor disminución de MTC cr a lo largo del primer año. Conclusión: el uso de icodextrina al inicio de la DP podría ayudar a corregir la alta permeabilidad basal en los primeros meses de diálisis. Las cinéticas realizadas a los 6 y 12 meses tras el inicio de diálisis son más representativas de la función peritoneal a largo plazo que las basales.
Peritoneal permeability differs between patients at the time of starting peritoneal dialysis (PD) and it can increase along with time on the technique. This fact is related to peritonitis, the biocompatibility of the dialysis fluids and the use of glucose as osmotic agent. The aim of the present study was to evaluate if the use of one exchange a day of icodextrine from the time of DP initiation affects the evolution of peritoneal permeability. Patients and methods: 56 patients starting PD (mean age: 48.3 ± 14.0; 62.5% males; 17.9% diabetics) that used one exchange a day with icodextrine from the time of starting PD. We performed a peritoneal transport kinetic study at the time of starting PD and then every 6 months during two years. We calculated the peritoneal mass transfer area coefficient of creatinine (Cr-MTAC) and urea (U-MTAC) as well as the D/P creatinine relationship (D/P Cr). As a control group we used the results of Cr-MTC of 249 patients that had used glucose as the only osmotic agent from the time of starting PD. Results: The peritoneal transport, calculated using Cr-MTC, U-MTC and D/P Cr, diminished at 12 months (11.7±5.7 vs. 8.1±3.1; 23.5±7.3 vs. 18.9±3.8; 0.72±0.09 vs. 0.67±0.08; respectively), staying stable afterwards.We found that high transporters (HA) patients (higher quatril Cr-MTC ) showed a higher diminution of Cr-MTAC along the first year of treatment. The diminution of Cr-MTAC after 12 months using icodextrine was significantly higher (p<0.001) that the one observed in the control group that only used glucose as osmotic agent (10.5±5.3 vs. 10.1±4.6). We found that high transporters (HA) patients (higher quatril Cr-MTC) showed a higher decrease of Cr-MTAC along the first year of treatment. Conclusion: the use of icodextrine at the time of starting PD might help to correct the high transport status observed in some patients during the first months of treatment. The peritoneal transport kinetic studies performed at 6 and 12 months after starting PD are more representative of the long term peritoneal transport characteristics of the patients than those performed at the time of starting PD.
INTRODUCTION
Peritoneal Dialysis (PD) has been shown to be a treatment option for Chronic Kidney Disease (CKD) with short and medium-term results equivalent to or higher than those of Haemodialysis (HD) in terms of patient survival.1-3 Since the peritoneum is a biological membrane that is repeatedly exposed to contact with non-fluids, its characteristics, which may differ from patient to patient at the start of dialysis, may also vary during the course of PD. Approximately 20% of patients on PD develop a high transport (HT) state during mid to long term, which results in failure of water transport or Ultrafiltration (UF).4,5 We call this acquired HT. This has been associated with a high incidence of peritonitis and time on PD, which suggests that inflammation and persistent exposure to a nonphysiological dialysis fluid (acid pH with lactate or a high glucose content) may be the main pathogenic factors. The use of glucose polymers (icodextrin) as an osmotic agent is, at least from the theoretical standpoint, a factor that can affect the peritoneal function over time. In an evaluation arising from the EAPOS study, it is shown that the use of icodextrin in prevalent patients is associated with a smaller increase in peritoneal permeability with time on dialysis. Thus it was suggested that the use of icodextrin could lead to less use of high concentration glucose dialysate, which would help to preserve the peritoneal function as high UF could be obtained during long dwell periods.6 Additionally, some investigators observe that the use of icodextrin, when compared to conventional solutions, is associated with a lower level of Glucose Degradation Products (GDP).7 Contrary to the theory that icodextrin can help preserve the peritoneal function is the fact that this solution still contains lactate and has an acid pH5,2 and it has been suggested that this may increase peritoneal inflammation and, consequently, permeability.8
The purpose of this study is to ascertain the evolution of the peritoneal function in the short-medium term in patients starting with PD using an exchange of icodextrin, and to verify whether its behaviour differs from our historic group which uses only glucose as an osmotic agent, and lactate as a buffer.9
PATIENTS AND METHODS
56 patients on the PD programme between February 1998 and October 2003 were included in the study. From the start, all the patients used one icodextrin exchange per day and the rest of the exchanges were standard glucose dialysate containing lactate as a buffer and acid pH. Eight patients (14.3%) were dialysed with on continuous ambulatory peritoneal dialysis (CAPD) and 48 (85.7%) on Automatic Peritoneal Dialysis (APD). All the patients were subjected to a baseline peritoneal kinetic study (within 4-6 weeks after the start of dialysis) and during the observation period, the kinetic study was repeated every six months on patients remaining on PD, which were 49, 38, 23 and 11 after 6, 12, 18 and 24 months respectively.
A peritoneal kinetic study was performed using a standard protocol of four-hour dwell period with 3.86% glucose concentration 2 L volume exchange. During the peritoneal function study, the patients fasted and were given no medication except for low doses of subcutaneous insulin as necessary. To measure the diffusive cacpacity, six samples of the peritoneal effluent were collected (at time 0, 30, 60, 120, 180 and 240 minutes) and a blood sample was also taken. Based on these determinations, the D/P Cr was calculated as described by Twardoski10 was calculated, as well as the mass transfer coefficients of urea (urea-MTC) and creatinine (cr-MTC) based on the mathematical model described previously.4 Depending on the peritoneal permeability change over time, the patients were classified, the patients were classified into four groups: high; mid-high; mid-low and low, depending on the Creatinine-MTC quartiles of our population.
To test the function of the aquaporins, sodium sieving was measured after 1 hour of dwell time during the peritoneal kinetic study at 6 and 18 months and, expressed as the percentage of relative reduction of sodium compared to the initial sodium level of 132mmol/L.
Cases of peritonitis and the cumulative number of days of inflammation during six month periods were recorded.
The Residual Renal Function (RRF) was measured at baseline and every six months as the average clearance of urea and creatinine, KT/V and weekly creatinine clearance.
The use of Agiotensin-Converting Enzyme Inhibitors (ACEI), Angiotensin II Receptor Blockers (A2RB) and betablockers was recorded.
The effect on cr-MTC after twelve months of using icodextrin was compared with a ‘historic’ control group on dialysis at La Paz Hospital between 1980 and 2001 using only glucose as the osmotic agent and lactate as a buffer, the data of which had already been published.9
The statistical analysis was made using SPSS11.0. The values are expressed as mean ± SD. A p value < 0.05 value was considered as being statistically significant. The differences between the groups were calculated by chisquare test, Student’s t-test or ANOVA as appropriate and by the Bonferroni post hoc test.
RESULTS
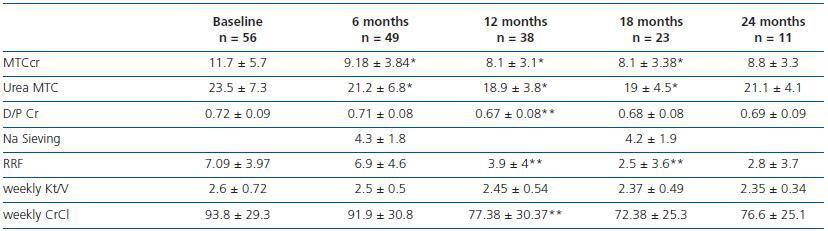
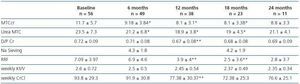
The average age of the patients was 48.3 ± 14 years (range: 20-85), 62.5% males and 17.9% diabetics. The causes of the CKD were: 25% Glomerulonephritis (GN); 17.9% tubulointerstitial nephropathy; 16.1% Diabetes Mellitus (DM); 16.1% systemic; 8.9% APKD; 7.1% glomerulosclerosis; 7.1% unknown; 1,8% vascular. 45% of the patients used ACEIs, 22% A2RB, and 45% beta blocker drugs. Table 1 shows the characteristics of peritoneal and residual renal function at baseline and six month intervals. The MTC for creatinine and urea and D/P Cr fell significantly with respect to the baseline values during the first year and later became stable. The sodium sieving did not vary between 6 and 18 months.
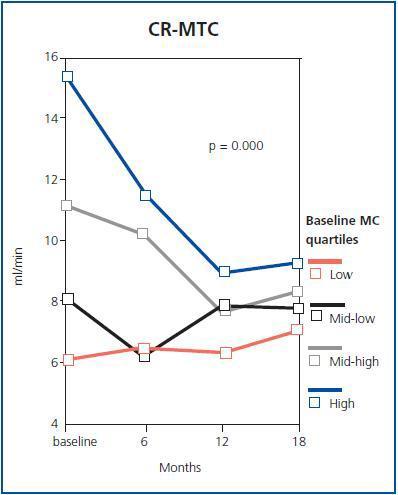
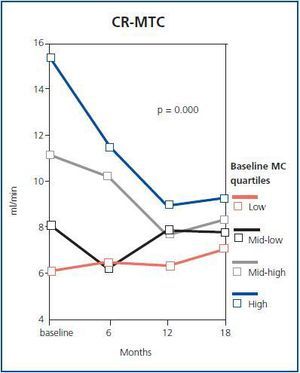
Diabetic patients showed greater initial transport, cr-MTC (15.8 ± 8.6 vs. 10.8 ± 3.4; p = ns) and D/P cr (0.78 ± 0.11 vs. 0.71 ± 0.08; p = 0.03). We found no differences in permeability during the first year among diabetics and nondiabetics and no significant differences in peritoneal transport from baseline in patients treated with CAPD and APD (data not shown). We found no differences in Cr-MTC whether or not the patients received ACEIs and/or A2RBs during the first year (10.4 ± 4.2 to 7.4 ± 2.7 in those using ACEIs or A2RBs and 11 ± 5.3 to 9.2 ± 2.8 in those not using them). Only 12 patients (21.4%) had peritonitis during the first year and only three (5.3%) had more than four accumulated days of peritonitis, with no significant differences in in MTC and Cr D/P among patients with or without peritonitis. When the patients were divided into four categories based on the transport type, according to baseline Cr-MTC, we found that patients with greater basal peritoneal permeability were those with the greatest reduction in cr-MTC during the first year (figure 1).
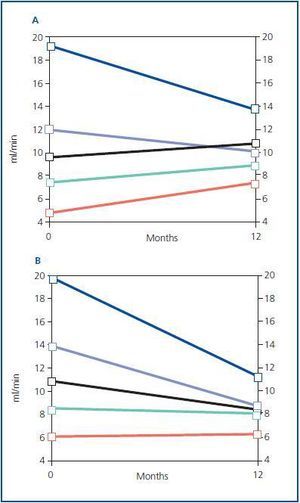
On comparing the current results with the historic group, we observed that the patients in the historic group were older (51.9 ± 16), there was a higher percentage of diabetics (25%) and a higher rate of peritonitis (35% of patients suffered one episode of peritonitis during the first year). No data was available on ACEIs or A2RBs use in the historic group but it is unlikely that its use was widespread in 1980 – 2001. There was a fall in Cr-MTC in all patients, between the start and twelve months after PD but in the icodextrin group (11.7 ± 5.7 to 8.1 ± 3) this was significantly higher than the historic group which used only glucose dialysate (10.5 ± 5.3 vs. 10.1 ± 4.6), (p < 0.001).
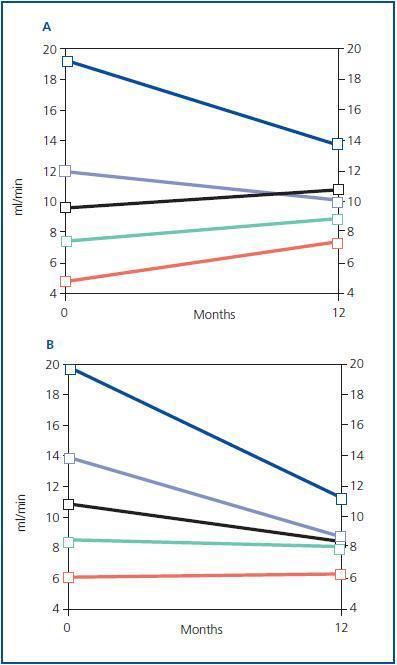
When we compare Cr-MTC quintiles as described in a previous study,9 we found that as in the control group (figure 2 A) the high transporters at baseline show a significant reduction in Cr-MTC by the first year (figure 2B) as compared with baseline. However, we should say that the patients in this study had baseline Cr-MTC levels that were higher than the historic group (11.7 ± 5.7 vs. 10.5 ± 5.3) and that the greatest reduction in peritoneal permeability was observed in patients with higher cr-MTC whereas, in patients in which the MTC was lower than 10, the peritoneal permeability remained practically unchanged.
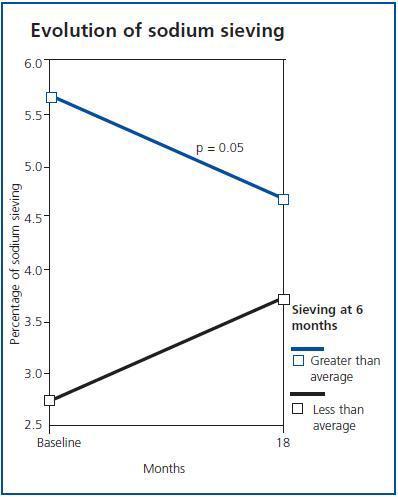
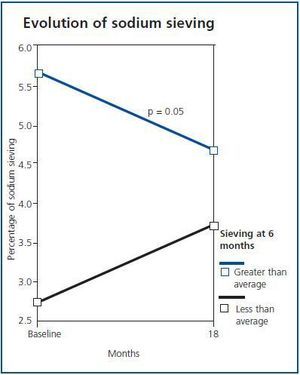
As can be seen in table 1, there were no significant changes in sodium sieving over time over time. However, as occurred with MTC, the sodium tended to normalise during the first months of PD (figure 3). Thus, in patients with a sodium sieving after six months that was lower than average (3.5%) we observed an improvement in the same (changing form 2.7 to 3.7%), while in those which a high sieving value, this fell (from 5.6 to 4.6%). We found no differences in the sodium sieving after six months or in the evolution after 18 months, based on the gender, type of dialysis, prsence of diabetes, use of drugs or having suffered from peritonitis. The sodium sieving maintained a good correlation with the MTCr (r = -0.39; p = 0.016), but not with the D/P cr.
DISCUSSION
In this study carried out in incident PD patients who used one icodextrin exchange from the start of PD, we found that the peritoneal fluid transport characteristics tends to normalise during the first months of PD as shown by near normal Cr-MTC, which is expressed in an approximation to normal of the extreme values of the Cr-MTC. This tendency to normalisation occurred mainly in patients with a high initial permeability in which we observed an important fall in the same during the first months of PD. This fact has already been reported by our group in previous studies performed on dialysate that contains only glucose as the osmotic agent and lactate as the buffer: after the first few months of contact with the dialysis fluids, if no serious peritonitis occurs, the peritoneal function tended to normalise.9 We previously observed in other studies that a peritoneal kinetic study performed after six months and one year would be more representative of what will happen in the long term, especially with respect to extreme values.4
Our main aim was to evaluate whether the use of icodextrin in patients subject to PD is of benefit to peritoneal function. Indeed, the evolution of the peritoneal permeability with icodextrin is similar to that observed with the use of classic glucose and lactate solutions (figures 2A and 2B), with a tendency to normalise the cr-MTC and a greater reduction in permeability during the first few months in patients with high cr-MTC values. However, overall, the fall in cr-MTC was significantly higher (p < 0.001) in the icodextrin group than in the ‘historic’ group, which only used glucose.
There are several explanations for the fall in the permeability during the first year in the icodextrin group, since it is a group with a lower rate of peritonitis, greater use of ACEIS and which starts with a higher baseline Cr-MTC. It is precisely in the high transporter group of patients that a reduction in peritoneal permeability is best observed during the first few months. However, the use of icodextrin may have contributed to the improved behaviour in the peritoneal permeability, since it permits a lower use of hypertonic glucose in patients HT at baseline. Solutions with higher concentrations of glucose may have toxic effects on the peritoneum, both direct and through the production of GDP, especially taking into account that we are making the comparison with a historic group that used lactate, which favours the formation of GDP. The findings of this study in incident PD patients the results of the EAPOS study performed on prevalent patients6 in which it is observed that in patients with an average time of three years on PD, the use of icodextrin slows down the increase in peritoneal permeability caused over time in PD, which would confirm the beneficial effect of using icodextrin in HT patients.
Sodium sieving results show an improvement of the peritoneal membrane function after initial contact with the dialysis solutions. We observed that patients with a low initial sodium sieving also improved during the first few months, which will almost certainly be accompanied by an improvement in UF. Thus, in those patients the use of icodextrin would not only permit good UF to be obtained despite having high permeability and a poor sodium sieving, but would also prevent the use of hypertonic glucose and its harmful effects on the peritoneal membrane from the start of PD.
However, the correlation between sodium sieving and Cr-MTC, but not with D/P Cr and the fact that HT patients (higher quartile of Cr-MTC) and those with a low sodium sieving are those who can improve the most during the first year, leads us to recommend the performing of kinetic studies during the first year with 3.86%, glucose concentration and sodium sieving and/or Cr-MTC in order to select the patients who would obtain the greatest benefit from using glucose polymers.
These results are of relevance, precisely at a time when the predictive value HD at baseline on morbidity and mortality is being debated,11 and some investigators have even suggested that these patients are poor candidates for PD and should be changed to HD.12 We have shown that the state of extreme HT characteristic at baseline may be partly reversible and that the use of icodextrin, which allows for high UF without an overuse of glucose, seems to ameliorate the HT status during the first few months of PD. Most studies in which the worst survival rate for HT at baseline has been found in CAPD patients who use glucose as the only as the osmotic agent,13-15 while in studies on patients on APD and/or patients using icodextrin, the predictive value of HT on morbidity and mortality disappears.16
The greatest limitation of this study is that a comparison is made between a historic group that does not have exactly the same characteristics as the current group in terms of permeability, use of ACEIS or A2RBs and incidence of peritonitis and it is possible that one or several of these facts is contributing to a greater fall in permeability during the first year. Although in both the historic group and the current group, lactate is used as a buffer, which may favour the formation of GDP and peritoneal toxicity due to overuse of glucose, we did not have a group that used glucose solutions low in GDP for comparison purposes.
In conclusion, the use of an exchange of icodextrin in HT patients at the start of the PD could help to correct the high permeability at baseline during the first months of dialysis. On the other hand, kinetic studies performed 6 and 12 months after the start of dialysis may be more representative of the peritoneal function in the long term.
Acknowledgements
To Fernando Álvarez-Ude, for his critical reading and statistical analysis.
Table 1. Evolution over time of the patients' kidney and peritoneal function
Figure 1.
Figure 2.
Figure 3.