Introducción: el uso de catéteres en hemodiálisis se asocia a un gran número de complicaciones. Sin embargo, se han realizado pocos estudios diseñados específicamente para evaluar este problema. Los objetivos del estudio han sido conocer el impacto en la supervivencia del paciente y el gasto económico que implica la utilización de catéteres. Métodos: estudio observacional y prospectivo histórico de siete años de duración en 260 pacientes incidentes en hemodiálisis en nuestra área de salud, ajustado a la comorbilidad y albúmina al inicio de la hemodiálisis. La media de edad fue de 65,5 ± 15,2 años, 62,3% varones, 25% diabéticos. La media del índice de comorbilidad de Charlson fue de 7,05 ± 2,8. Resultados: el 47,3% de los pacientes inicia hemodiálisis con catéter, el 41,5% con FAV-auto y 11,2% con FAV-PTFE. El seguimiento medio fue 2,31 años/paciente. El riesgo de mortalidad ajustado por comorbilidad fue mayor para los que inician hemodiálisis con un catéter, HR: 1,86 (1,11-3,05). Este efecto negativo también se observó en el 57,3% de pacientes que a lo largo del seguimiento requirieron un catéter, HR: 1,68 (1,00-2,84) y, además, fue tiempo dependiente; a mayor tiempo con catéter, mayor mortalidad: HR 7,66 (3,34-17,54), tertil 3 vs. tertil 1. El coste del empleo mes/catéter fue de 561,31 euros. Conclusiones: el uso de catéteres tunelizados es un factor independientemente asociado con la mortalidad de los pacientes, tanto al inicio como a lo largo del seguimiento, es tiempo dependiente y conlleva un elevado coste económico.
Introducction: Tunneled catheters in hemodialysis are associated with poor prognosis, however, few prospective studies have been designed to specifically evaluate this aspect. The objective has been evaluate the impact of tunneled catheter in patient mortality and costs attributable to this procedure. Methods: A seven years prospective cohort study was performed in all patients starting hemodialysis in our health care area adjusting for comorbidity and albumin. The study comprised 260 patients with Charlson index 7.05 ± 2.8 (age 65.5 years, 62.3% males, 25% with diabetes mellitus and 37.7% with a previous cardiovascular event. Results: The first vascular access was a catheter in 47.3%, PTFE in 11.2% and native arteriovenous fistula in 41.5%. Minimum follow-up was one year, with an average of 2.31 years/patient. The mortality risk adjusted for comorbidity was greater among the patients that started with catheterization, HR: 1.86 [1.11-3.05]. This negative effect was observed in 57.30% of those subjected to catheterization at any stage (HR: 1.68 [1.00-2.84] and proved to be time dependent, i.e., the longer catheterization, the greater the risk: HR: 7.66 [3.34-17.54] third versus first tertil. The cost directly attributable to catheter use was 563.31 euros/month. All poor prognosis groups showed lower albumin and hemoglobin levels, without differences in efficacy. Conclusion: Tunneled catheter use at any time is associated with an increased risk of death. This effect increases with the duration of catheterization, both circumstances are independent of patient comorbidity at time start of hemodialysis and implies a higher net cost.
INTRODUCTION
Obtaining and maintaining vascular access is one of the most important challenges in the management of patients on haemodialysis (HD). The type of vascular access used has both clinical and economic implications. When compared with alternative HD access, the autologous arteriovenous fistula (AVF) lasts the longest, is the least likely to become infected and is the least expensive.1-4 Several .studies have shown the potential high risk of death from the use of tunneled catheters (CAT) in HD patients. CAT are associated with a higher number of dysfunctions, infections and hospitalisations.5-7 According to Medicare data from the United States, the use of catheters also costs an additional 20,000 dollars when compared with auto-AVFs.8 Current guidelines recommend the use Auto-AVF for vascular access and, if a suitable vein cannot be found, a prosthetic Poly tetra fluoro ethylene (PTFE) graft should be implanted. A CAT should only be considered when no other vascular access can be obtained. In order to follow these recommendations it is essential that a multidisciplinary vascular access team is created.1 Some studies have described the differences that exist from one country to another in the prevalence and consequences of using different types of vascular access.9 In Spain, scarce prospective data is available regarding survival outcome and costs associated with CAT use. Therefore it is important that up-to-date information is obtained about the situation in our health care area.
The objective of this study is to establish the impact that the use of CAT has on the survival of haemodialysis patients and ascertain the costs associated with this type of vascular access.
MATERIAL AND METHODS
Methodology and study design
A prospective observational cohort study of incident HD patients in the health area. 510,000 people live in this area which includes a Hospital Dialysis Unit and an outpatient centre. All data was collected prospectively from a single database that covered the whole health area. The process was coordinated by a hospital nephrologist and information was added to the hospital patients’ electronic medical records.10
Patients on haemodialysis from 1/1/2000 to 31/12/2005 and who were monitored until 31/12/2006 were included. The following data was used: 1) baseline characteristics and patient evolution: date of birth, sex, cause of chronic kidney disease, Charlson comorbidity index,11 cause of hospitalisation and death; 2) Vascular access characteristics: type of vascular access ( auto-AVF, PTFE graft, CAT), date vascular access was obtained and evolution of vascular access (dysfunctions, infections and thrombosis). The patients’ survival time was calculated from the first dialysis session to the time of death; survivors were censored” when transplanted, when there was a change in dialysis modality or at the end of the observation period. The duration of catheterisation was calculated for each haemodialysis patient as a percentage of the total follow-up time. The catheter was tunneled in 94% of cases. Non-cuffed central venous catheters in our health arera are almost immediately replaced by CATs. These were Hemaglyde-DE BARRD®, Mahunkar QUINTON® and Canon ARROW®. Patients who received dialysis using a PTFE graft were excluded in order to be able to compare the survival of patients who underwent dialysis with “the best vascular access” (auto-AVF) and “the worst vascular access” (CAT).
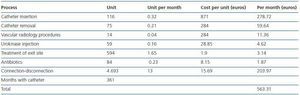
The cost assessment of catheter use was carried out over a two-year period, starting in January 2005, using a specific data collection process which recorded: the type of tunneled CAT, type of event (malfunction, thrombosis, infection, extrusion), radiological procedure (check-up, repositioning or removal and new insertion), nursing intervention (connection, changing the dressing and treatment), treatment of infections and the use of thrombolytic drugs. The cost of each component was established according to the hospital charges. The monthly cost of a catheter was calculated on the basis of the total accumulative cost and the duration of the follow-up. In order to calculate the estimated cost, the cost of catheter insertion and removal was added and divided by the total duration of the follow-up period in months. The costs that were exclusively generated by the catheter were calculated, such as the cost of connecting and disconnecting it, the cost of nurse time and the materials used in each haemodialysis session, as well as any maintenance and treatment costs associated with the catheter.
Statistical analysis
The analysis was carried out using the statistical software package SPSS version 11.0 for Windows. The qualitative variables were expressed as percentages and the quantitative variables as the mean ± standard deviation (SD). The Student’s t-test or the analysis of variance (ANOVA) were used to compare quantitative variables and the chi-square test was used for qualitative variables. The analysis of survival was carried out using the logrank test and Kaplan-Meier curves. The Hazard Ratio was calculated using the Cox regression model; the univariate analysis included diabetes mellitus, age, Charlson’s comorbidity index, sex, as well as haemoglobin, albumin and Kt/V at the start of dialysis, and the initial the type of vascular access. All the variables that were significant in the univariate analysis were included in the multivariate logistic regression model with stepwise backward elimination procedure. During the adjustment, if the model included the Charlson index, it could not include diabetes or age since they were already included in this index. The proportionality of hazards over time was assessed for the final model.
Cohort description
This study involved 260 patients with a mean age of 65.5 ± 15.2 (range 22-88); 62.3% were men, 25% had diabetes mellitus and 37.7% had suffered a cardiovascular event before starting haemodialysis. The mean score in the Charlson index was 7.05 ± 2.8 (range 2-16), distributed in the following way: 40.3% scored between 2 and 5; 31.2% scored between 5 and 7 and 28.5% scored over 7.
RESULTS
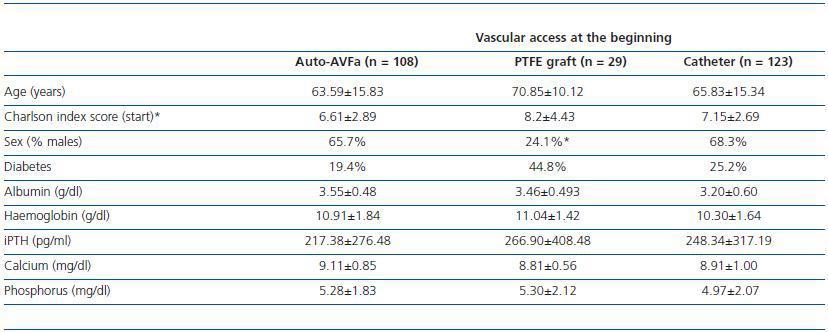
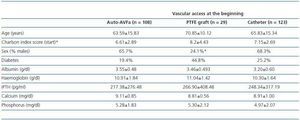
Forty seven per cent of patients underwent haemodialysis with a catheter, 41.5% with an auto-AVF and 11.2% with a PTFE graft. Table 1 shows the baseline characteristics of patients in relation to the type of initial vascular access.
The total cumulative follow-up time was 600.82 years (2.31 years/patient), during which there were 14.6% transplants, 27.9% deaths, 7.1% patient transfers to other areas, 2.8% patients recovered their kidney function and 2.2% switched to peritoneal dialysis.
Prognostic value of catheterization on patient survival
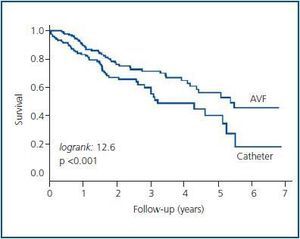
Starting haemodialysis with an auto-AVF vs. CAT
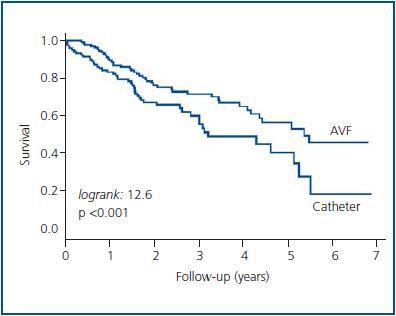
Survival among patients who start dialysis with an auto-AVF is 2.79 years/patient whereas for those who start haemodialysis with a CAT, it is 1.95 years/patient. After one year, the probability of survival is 91.7% for patients who used an auto-AVF whereas for patients who used a CAT, it is 83.34%. After four years, the probability of survival for patients using an auto-AVF is 73.72% but it is 48.97% for patients using a CAT (logrank 12.6, p < 0.001), (figure 1).
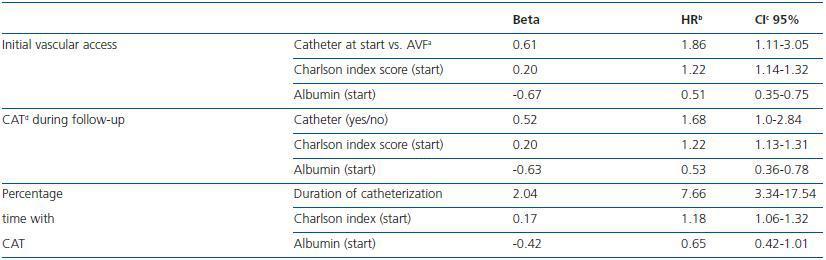
All the variables that were significant in the univariate Cox model were included in the multivariate analysis. The final adjusted model included the variables “type of vascular access”, Charlson index and albumin (table 2). The Cox regression analysis showed a risk-adjusted mortality rate for patients who started haemodialysis with a CAT that was 1.86 times higher than that of those patients who started with an AVF, CI 95% (1.11-3.05).
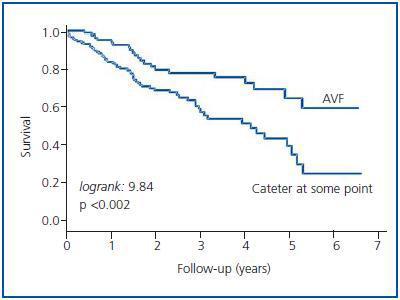
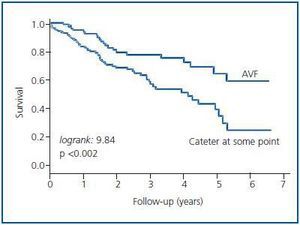
Occasional use of a catheter vs. continued use of an AVF
A total of 57.3% of patients needed a catheter at some point during follow-up vs. 35.38% who always continued to dialyzed with an AVF and 7,32% who always was been dialyzed with a PTFE graft. The survival time for patients who never had to use a CAT was 2.75 years/patient whereas for patients who had to use a CAT it was 2.11 years/patient. After one year, the probability of survival was 95.31% for those who had never used a CAT and 83.4%, for those who had done so at some point. After four years, the probability of survival for those who always used an auto-AVF was 74.8% versus 52.0% for those who had used a CAT at some point (logrank 9.84, p < 0.002), (figure 2).
The final model, adjusted using the Cox proportional hazards model, included the variables “type of vascular access”, Charlson index and albumin. The risk of death, adjusted for albumin and comorbidity, in patients that required a CAT was 1.68 with a CI 95% (1.00-2.84), (table 2).
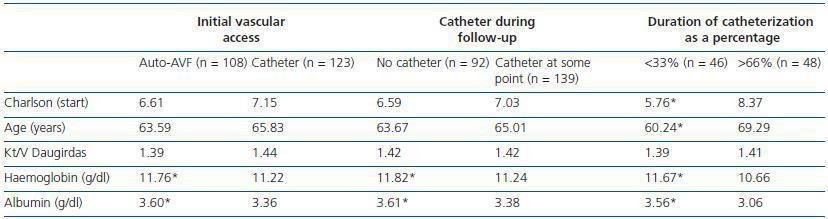
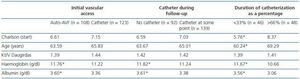
Table 3 shows the following variables distributed into 3 groups (vascular access at the beginning of haemodialysis, the use of CAT at any point during the follow-up, and the duration of haemodialysis with a CAT as a percentage): patient age and the Charlson index score at the beginning of haemodialysis, as well as haemoglobin, albumin and Kt/V (Daugirdas formula).
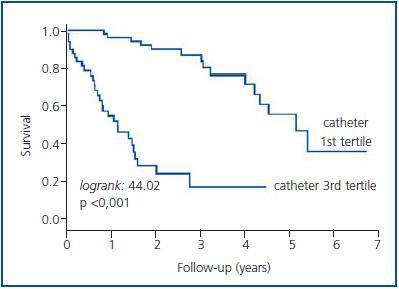
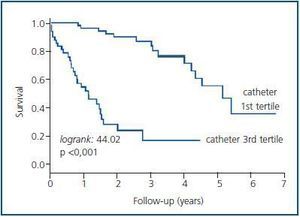
Duration of catheterization (1st tertile vs. 3rd tertile)
The 139 patients who required a catheter at some point were classified into tertiles and the duration of dialysis treatment with a catheter was calculated as a percentage. A third of patients underwent dialysis with a catheter for less than 18% of the time, with a follow-up of 3.2 years/patient vs. 0.95 years/patient for the third that underwent dialysis for over 52% of the time using a catheter (logrank: 44.02, p < 0.001), (figure 3). The remaining third underwent dialysis with a catheter for between 18 and 52% of the time. The probability of survival is 96.0 vs. 53.54% for the first year and 75.9 vs. 14.56% for the fourth. The probability of survival for patients who used a catheter less than 18% of the time in dialysis was 5.25 years and 1.17 years for those who used the catheter for more than 52% of the time. These differences are still evident after correction for patient comorbidity with an adjusted HR of 7.66 (3.34-17.54), (table 2). Table 3 shows the comorbidity index, patient age, mean haemoglobin, albumin and Kt/V of the first and last tertile.
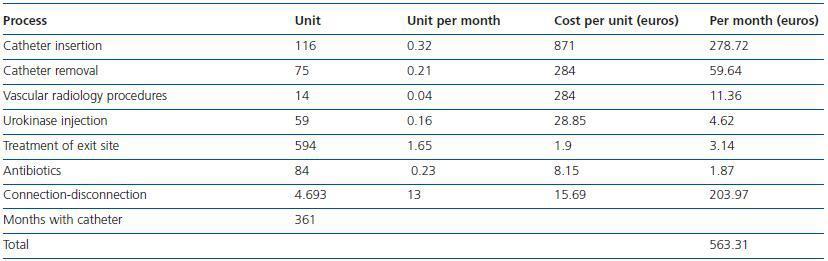
Catheter cost analysis
The number of events per month and the unit cost per event can be found in table 4. The cost of connecting/disconnecting a catheter was 15.69 euros, including costs derived from complications and not including hospitalisation costs.
DISCUSSION
Our study demonstrates the deleterious effect that the use of a catheter in haemodialysis can have on patient survival and the elevated costs associated with this type of vascular access. Although there are limitations associated with an observational study, it is not possible to carry out a controlled study for ethical reasons. Nevertheless, all patients from the health area were included and a careful multivariate analysis was carried out in order to monitor more complicated variables and increase the validity of the results.
In this series, 47% of patients began haemodialysis with a catheter. Other studies also describe a high incidence of patients that do the same.9,12,13 When patients begin haemodialysis using a CAT, even after correction for comorbidity, they present a mortality risk that is almost twice that of patients who undergo haemodialysis with an auto-AVF. This statistic is similar to that published in other studies which describe a clear link between mortality and the use of catheters.14-16 Therefore, perhaps our first objective should be to try to minimise the use of catheters when starting haemodialysis, which is something that we believe is possible within the context of a multidisciplinary vascular access follow-up, by creating an advanced chronic kidney disease clinic where AVFs can be planned in advance. Following this study, over 70% of patients who were assessed in the multidisciplinary clinic underwent haemodialysis with vascular access other than by venous catheter. A similar figure was reported by Lorenzo et al.16,17
Another interesting finding was the fact that increased mortality associated with the use of the catheter is not only evident at the start of dialysis treatment but also continues throughout the follow-up. In effect, patients who require a catheter at any point have a lower probability of survival than patients who continue to use an auto-AVF, regardless of the initial comorbidity. Similarly, a recent study described how mortality in patients who used an AVF increased if they required a catheter and decreased if a patient switched from using a catheter to an AVF.18 These results suggest that when a patient is undergoing dialysis with an AVF, this should be maintained for as long as possible by implementing a programme for preventing AVF dysfunction and carrying out an emergency declotting of the AVF if thrombosis occurs. The aim is to use a CAT only when it is absolutely necessary.
Similarly, the duration of catheterisation (and this can be considered a completely new analysis) is also associated with patient survival, irrespective of comorbidity. This analysis, based on tertiles showed a mortality risk up to seven times greater in patients who undergo dialysis for more than 52% of the time with a catheter.
We found that the underlying causes for the association between the use of CAT and increased mortality are older age, increased comorbidity and the CAT itself, the latter a factor that remains statistically independent. The Pastan S19 study reported similar findings with regard to comorbidity and attributed part of the morbidity associated with catheters to an inadequate dialysis dose. Nevertheless, our study did not identify any differences in the mean dialysis dose received by patients when they used a catheter and when they did not because the Kt/V was similar. Another possible explanation for the link between mortality and the use of catheters could be the chronic subclinical inflammation associated with CAT, aside from any other complications associated with the exit site, tunnel or bacteraemia. Low albumin and haemoglobin levels, as well as resistance to treatment with EPO, are factors that are commonly linked to inflammation and mortality.20-22 In this study, patients who required a catheter at any point or who underwent dialysis for more than 52% of the time with a catheter presented lower mean albumin and haemoglobin values. The study carried out by Allon et al.18 also described a link between mortality and catheters, attributing it to inflammation, although this study was unable to demonstrate higher C-reactive protein levels for the CAT group. This study did not assess C-reactive protein and therefore could not provide a more precise assessment of the effect of inflammation on the albumin and haemoglobin values.
Finally, the use of a dialysis catheter costs over 500 euros a month. This cost may not necessarily be universal across all centres but it gives an indication of what to expect when making comparisons. Similarly, in a study carried out in Canada in 2005, the mean cost of catheter use per patient/per year was 5,278 euros, which was slightly lower than the amount calculated in this study: 6,760 euros (563.31 x 12).23 Consequently, we should promote the use of the AVF and optimize or increase the resources available if necessary. Even if this requires an initial investment, it would be justified as the use of catheters and the costs associated with them would decrease.
In conclusion, our study shows that the use of catheters compared with AVFs in patients on haemodialysis is associated with higher mortality both at the beginning of dialysis and throughout the follow-up, irrespective of the patient’s initial comorbidity. Mortality is higher in patients who use the catheter for longer. Furthermore, the use of a catheter implies additional cost. The creation of multidisciplinary vascular access teams would result in a reduction in the use of CAT and probably an increase in patient survival rates.
Further studies that focus on the relationship between “duration of catheterization” and mortality are needed.
Acknowledgements
This study was partially financed by a project run by the Alcorcón Hospital Foundation and the Íñigo Álvarez de Toledo Kidney Foundation, centres which are part of REDinREN (Carlos III Health Institute, Red 6/0016). Coauthors: The multidisciplinary vascular access team is also made up of the following members: Rubio E, Alegre R, Valero R, Armijo J, Lasala M, Rueda JA, Fernández G, López Revuelta K, Barrio V, Del Castillo C, Marco B, Ochando A, Rayuela C, Mas M, Prieto R, Sesmero C, Piña MD, González A.
Figure 1.
Table 1. Baseline characteristics of the patient subgroups according to the type of initial vascular access. The values are shown as the mean ± standard deviation, * p < 0.05 (ANOVA)
Figure 2.
Figure 3.
Table 2. Predictors of mortality in the Cox proportional hazard model
Table 3. Comorbidity and age values at the start of haemodialysis, together with mean haemoglobin, mean albumin and dialysis effectiveness (Kt/V Daugirdas) during follow-up. Patients were classified according to the type of initial vascular access (catheter vs. AV
Table 4. Summary of clinical events and a calculation of the costs of the general follow-up and of the use of a catheter during one month. These processes are not applicable to fistulas and therefore represent additional monthly costs associated with the use of ca