Atrial fibrillation (AF) is the most frequent type of arrhythmia with a prevalence of 8.5%1 in the general population, ranging between 13.62 and 23.4%3 in patients on haemodialysis (HD). It tends to be associated with structural heart disease, particularly left atrial dilation, and electrolyte imbalances such as hypokalaemia and hypocalcaemia must be avoided as they can precipitate a cardiac arrhythmia. We present the case of a patient with chronic renal failure (CRF) on HD, with a flutter that was difficult to treat pharmacologically because of intolerance to various antiarrhythmic drugs. The patient required pacemaker implantation in order to introduce treatment with beta-blockers (BB) and control the heart rate (HR). The patient was 72 years old with end-stage CRF and a history of ischaemic heart disease, high blood pressure, diabetes mellitus, severe vascular disease, chronic AF, and inclusion in the HD programme since 2004. The history of heart disease began in November 2003 when the patient suffered an acute myocardial infarction with an episode of fluttering, which reverted after administering diltiazem retard in 120mg doses every 12 hours. The echocardiogram showed a non-dilated left ventricle with moderate septal hypertrophy (18mm), preserved ejection fraction (EF) and dilated left atrium. In August 2005, the patient presented a new episode of rapid AF and digoxin treatment was reinitiated with a dose of 0,125mg twice per week. Treatment was suspended after one week due to digitalis toxicity. In January 2005, due to a new episode of rapid AF, treatment was begun with 200mg amiodarone five days a week, with which we managed to achieve sinus rhythm (SR). Treatment was discontinued after one month due to hypothyroidism. Bisoprolol (5mg/dat) was added for persistent cardiac arrhythmia and the patient reverted to sinus rhythm, but it had to be discontinued ten days later due to bradycardia. In May 2006, the patient presented another AF episode despite being treated with diltiazem. Since it was ineffective, it was discontinued and treatment with bisoprolol was initiated once more. In August 2009, bisoprolol was increased to 7.5mg due to rapid AF. The drug was discontinued one month later due to symptomatic bradycardia of 38 beats/min (Table 1). No electrophysiological study was performed at any time during the course of events due to patient refusal. Given the treatment difficulty, we decided to implant a pacemaker in order to reintroduce BB treatment to control the HR. The patient is currently asymptomatic and shows a good tolerance of the treatment. Treatment of AF consists of achieving SR and/or controlling the heart rate. Different drugs may be used: digoxin, beta blockers, non-dihydropyridine calcium channel blockers and amiodarone. However, they are not free from adverse effects in CRF patients. Digoxin is less effective for controlling heart rate, but it is very widely used in patients with a low EF. For patients on HD, it is recommended not to use loading doses, and the maintenance dose should be 0.0625mg/day or 0.125mg every other day. The most frequent adverse effects are supraventricular tachycardia and bradyarrythmia (to the point of atrioventricular block), bigeminy and gastrointestinal abnormalities.4 BB and non-dihydropyridine calcium channel blockers are the correct drugs for preserved EF, but care must be taken with patients with decreased EF due to the drugs’ negative inotropic effects.4 BBs with non-renal excretion can be safely prescribed depending on the heart rate and blood pressure. Amiodarone is the drug of choice in patients with a low EF whose HR cannot be controlled with digoxin. Its adverse affects are as follows: In the thyroid, hypothyroidism or hyperthyroidism; in the respiratory tract, pulmonary fibrosis; and in the heart, long-QT interval and bradycardia with atrioventricular block.4 With HD, dosage for antiarrhythmics is a complicated topic, given the increase in its half life and multiple interactions with other drugs commonly used by these patients. Our patient presented numerous complications associated with different antiarrhythmic treatments without gaining control over the chronic AF and with frequent tachyarrhythmia episodes. He therefore required implantation of a permanent pacemaker in order to control HR using beta blockers, with no new cardiac incidents.
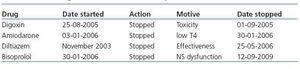
Table 1. Chronological evolution of antiarrhythmic treatment