Antecedentes: El síndrome urémico hemolítico (SUH) es la causa más común de insuficiencia renal aguda y la segunda de insuficiencia renal crónica (IRC) durante la infancia. Los factores que condicionan la recuperación incompleta de la función renal antes del ingreso hospitalario han sido poco estudiados. Objetivos: Identificar en niños con SUH, antes de su internación, los factores de riesgo que determinan una recuperación incompleta de la función renal. Métodos: Estudio retrospectivo de caso control. Variables: edad, sexo, duración de la diarrea (D+), deposiciones con sangre, vómitos, fiebre, deshidratación, antibiótico en terapia previa y recuperación incompleta de la función renal definida como la presencia de proteinuria, hipertensión arterial, aclaramiento reducido de creatinina e IRC durante el seguimiento. Se incluyeron pacientes de ambos sexos, menores de 15 años, con SUH. Resultados: Se estudiaron 36 pacientes, 23 de ellos varones (65,3 %, intervalo de confianza [IC] 95 % 45,8-80,9). Con una media de edad de 2,5 ± 1,4 años. 21 requirieron diálisis (58 %, IC 95 % 40,8 a 75,8) y 13 (36,1 %, IC 95 % 19,0 a 53,1) no recuperaron por completo su función renal. En un modelo de análisis bivariado solo fue un factor de riesgo significativo la deshidratación definida como una pérdida de peso > de 5 % (odds ratio [OR] 5,3, IC 95 % 1,4 a 12,3; p 0,0220). En un modelo multivariado (regresión de Cox), fue marginalmente significativa la deshidratación (CR 95,823, IC 95 % 93,175 a 109,948; p = 0,085). Conclusiones: Los resultados obtenidos sugieren que la deshidratación previa a la internación puede constituir un factor que incrementa el riesgo de presentar una recuperación incompleta de la función renal a largo plazo en niños que padecieron SUH D+. Por ello, se recomienda una cuidadosa vigilancia del estado de hidratación en niños con riesgo de desarrollar SUH D+ durante los cuidados ambulatorios.
Background: Haemolytic uremic syndrome (HUS) is the most common cause of acute renal failure and the second leading cause of chronic renal failure in children. The factors that affect incomplete renal function recovery prior to hospital admission are poorly understood. Objective: To analyse the risk factors that determine incomplete recovery of renal function prior to hospitalisation in children with HUS. Method: A retrospective case-control study. Variables: age, sex, duration of diarrhoea, bloody stools, vomiting, fever, dehydration, previous use of antibiotics, and incomplete recovery of renal function (proteinuria, hypertension, reduced creatinine clearance, and chronic renal failure during follow-up). Patients of both sexes under 15 years of age were included. Results: Of 36 patients, 23 were males (65.3%; 95%CI: 45.8 to 80.9), with an average age of 2.5±1.4 years. Twenty-one patients required dialysis (58%; 95% CI: 40.8 to 75.8), and 13 (36.1%; 95% CI: 19.0 to 53.1) did not recover renal function. In the bivariate model, the only significant risk factor was dehydration (defined as weight loss >5%) [(OR: 5.3; 95% CI: 1.4 to 12.3; P=.0220]. In the multivariate analysis (Cox multiple regression), only dehydration was marginally significant (HR: 95.823; 95% CI: 93.175 to 109.948; P=.085). Conclusions: Our data suggest that dehydration prior to admission may be a factor that increases the risk of incomplete recovery of renal function during long-term follow-up in children who develop HUS D+. Consequently, in patients with diarrhoea who are at risk of HUS, dehydration should be strongly avoided during outpatient care to preserve long-term renal function. These results must be confirmed by larger prospective studies.
INTRODUCTION
Haemolytic uremic syndrome (HUS) is a multi-system thrombotic microangiopathy with various aetiologies. This entity is clinically defined as the triad composed of microangiopathic haemolytic anaemia, thrombocytopenia, and acute renal failure (ARF). HUS is the most common cause of ARF and the second leading cause of chronic renal failure (CRF) in infants.1
HUS is divided into two classes, depending on whether the patient previously suffered from diarrhoea (D+) or not (D-).2 The most common class of HUS in children is D+, which is caused by a shigatoxin (STX) produced by one of a group of enterobacteria, primarily enterohaemorrhagic Escherichia coli O157:H7 (EHEC).3
HUS associated with STX is prevalent throughout the world in regions of high incidence of EHEC gastroenteritis, such as Argentina, Canada, United States, and Western Europe.4
In HUS produced by EHEC, more than 95% of children recover from the acute disease, thanks to modern methods of managing electrolyte and water balance, arterial hypertension, and ARF. Mortality is primarily derived from intercurrent infections and neurological, gastrointestinal, or cardiac complications.5
Cohort studies of patients who survive for at least 3 years of follow-up have shown that 65% of these individuals recover renal function and normal blood pressure levels, 15% continue to exhibit proteinuria with or without hypertension, and 20% end up with CRF.6
The long-term renal prognosis in these cases is determined by the severity of acute renal damage and by the initial destruction of nephronal mass. Several studies have demonstrated that in hospitalised patients during the acute phase of the disease, the presence, intensity, and duration of anuria, hypertension, and the need for dialysis are all associated with an increased risk of residual renal damage and CRF.7
Given that pre-renal ARF due to dehydration is the most common cause of oliguria and anuria in small children, representing 70% of non-hospital cases of ARF,8 several authors have shown that volume expansion in hospitalised paediatric patients with HUS has a nephro-protective effect.9
However, there is lack of studies in the medical literature that examine which factors that are present prior to hospitalisation contribute to an increased risk of incomplete recovery of long-term renal function in paediatric patients with HUS D+.10,11
The goal of our study was to identify the risk factors present prior to hospitalisation that are associated with incomplete recovery of renal function in children with HUS.
METHOD
We designed a retrospective study of cases (patients with HUS D+ who did not completely recover renal function) and controls (patients with HUS D+ who did eventually recover complete renal function). For retrospective data collection, we reviewed all consecutive clinical histories for patients hospitalised between 01/01/2000 and 31/12/2011.
We included patients of both sexes, aged 15 years or less, and who were diagnosed with HUS D+ (microangiopathic anaemia with schistocytes, thrombocytopenia, some degree of ARF, and an abdominal ultrasound revealing symmetrically enlarged kidneys)1; we excluded all patients with thrombotic thrombocytopenic purpura, malignant hypertension, vasculitis, disseminated intravascular coagulation, sepsis, or renal vein thrombosis.12
We formulated an ad hoc datasheet with the following variables: age, sex, weight, height, hydration state (defining patients as normally hydrated or dehydrated if any of the following symptoms were present: dry mucosa, lack of tears, decreased skin turgor, slow capillary refill, or weight loss >5%), previous administration of antibiotics to treat diarrhoea, the duration of diarrhoea, bloody stools, vomiting, fever, dialysis requirements, and incomplete recovery of renal function defined as the presence of proteinuria, arterial hypertension, reduced creatinine clearance, or CRF during the follow-up period.
Discrete variables were described as percentages with a 95% confidence interval (CI), and continuous variables were described as mean ± standard deviation. We compared samples using Fischer’s χ2 tests and Student’s t-tests. We performed a bivariate risk analysis using odds ratios (OR) with a 95% CI. We also performed a multivariate analysis using a Cox multiple regression equation. We interpreted P-values <.05 to be significant.
Our study received the approval of the hospital ethics committee, and was self-financed.
RESULTS
We reviewed the clinical histories for all patients admitted with a probable diagnosis of HUS D+ to the paediatrics and neonatology department at the Cordoba Private Hospital (Argentina) between 1 January 2000 and 31 December 2011. We excluded 9 patients due to a final diagnosis that was not HUS D+, 3 who were transferred to other institutions during peritoneal dialysis, and 2 due to incomplete data registries.
The final sample size was 36 patients with a confirmed diagnosis of HUS D+: 23 boys (65.3%; 95% CI: 45.8-80.9) and 13 girls (36.1%; 95% CI: 19-53.2), with a mean age of 29.1±16 months and a range of 9.2 months to 7.3 years of age.
For our analysis, patients were divided into two groups: a case group, composed of 13 patients (36.1%; 95% CI: 19.0-53.1) with HUS D+, who did not completely recover renal function during the follow-up period, and a control group, composed of 23 patients (63.9%; 95% CI: 46.8-80.9) with HUS D+, who did completely recover renal function during the follow-up period. The mean duration of follow-up was 7.3±1.7 years for the case group, and 7.6±1.3 years for the control group (P=.3140). In the case group, 12 out of 13 patients required dialysis (92.3%; 95% CI: 63.9-99.8), whereas only 9 out of 23 patients required dialysis in the control group (39.1%; 95% CI: 17.1-61.2) (OR: 2.3; 95% CI: 0.7-7.0; P=.2052).
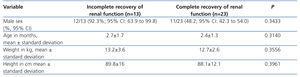
The baseline demographic and anthropometric characteristics (weight, height, sex, and age) were similar between the two groups (Table 1).
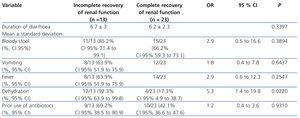
The comparison using the bivariate model, which included the following clinical variables assessed prior to hospitalisation: duration of diarrhoea, bloody diarrhoea, fever, vomiting, dehydration, and use of antibiotics, revealed that only dehydration was significantly correlated with a lack of complete recovery of renal function during the follow-up period (Table 2).
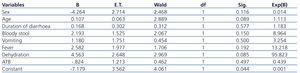
As regards the multivariate test that we carried out using the same potential risk factors from prior to hospitalisation, dehydration was the only factor that was a marginally significant predictor at the time of hospitalisation (Table 3).
DISCUSSION
To our knowledge, this is the first study to report dehydration prior to hospitalisation as a risk factor for incomplete recovery of renal function during the follow-up period in children with HUS D+.
Several previous studies have linked acute renal failure to the severity of renal damage, the level of destruction of the nephronal mass, the presence and duration of anuria, and severe hypertension as signs associated with renal damage and the need for dialysis among hospitalised patients.7,10,11
Only two studies have examined risk factors for ARF and the need for dialysis prior to hospitalisation, one prospective10 and one retrospective,11 but neither of these studied the effect of dehydration on long-term renal function in patients on and off dialysis with HUS D+.
As indicated by Spizzirri et al.,6 long-term prognosis is worse among patients with more than one day of anuria and those requiring dialysis. In this study, 37.3% of patients with these characteristics developed some level of renal involvement during the follow-up period, a value very similar to the rate we observed in the follow-up of our own study sample, although the risk factors evaluated were different.
The primary strength of this study was to consider factors present prior to hospitalisation that could plausibly produce long-term renal damage (due to hypovolemia from dehydration), based on the observation of the protection afforded to the kidneys by volume expansion in hospitalised patients.9
Our results differed from those by Carter et al., who long ago demonstrated the relationship between prior administration of antibiotics and later development of HUS.13 In our study sample, the results did not show a similar trend; however, in accordance with our results, this hypothesis has been questioned by other authors as well, who did not observe an increased risk of HUS or incomplete recovery of long-term renal function, especially in patients who received fosfomycin or trimethoprim-sulfamethoxazole to treat the enteric diarrhoea produced by EHEC.14,15
We also observed the tendency that patients with an incomplete recovery of renal function were primarily male, and had an older age than control patients, although these differences did not reach statistical significance; the predominance of this condition in males has been mentioned in other studies.10
Patients with an incomplete recovery of renal function during the long-term follow-up period in our study had a more severe degree of acute deterioration in renal function, and in concordance with the results from the study by Balestracci et al., required dialysis at a greater frequency than control patients, although we did not observe statistically significant differences in this context.11
The primary limitation of our study was the small sample size, which may have led to the lack of statistical significance for several of the factors analysed both in the bivariate and multivariate analyses (type II error or ß), as well as the retrospective nature of the data collection, which may have produced a bias in regards to the information obtained.
Without a doubt, the most relevant finding of our study (the importance of dehydration at the moment of hospitalisation) must be confirmed through larger, prospective studies. Unfortunately, the prospective study by Wong et al. did not take into account this aspect, although they do mention unstoppable vomiting as a significant risk factor,10 this being a known precursor of dehydration.
CONCLUSIONS
Our results suggest that dehydration prior to hospitalisation is a factor that could increase the risk of incomplete recovery of renal function during long-term follow-up in paediatric patients with HUS D+. As such, hydration state should be closely monitored in children at risk of developing HUS D+, and in the case that dehydration should be detected, it must be treated in a timely and effective manner using volume expansion methods in order to prevent hypovolemia, renal damage, and the risk of incomplete recovery of renal function. These results require corroboration from larger, prospective studies.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the content of this article.
Table 1. Baseline demographic and anthropometric characteristics of the study sample
Table 2. Bivariate analysis of risk factors that played a role prior to hospitalisation
Table 3. Cox regression model adjusted for risk factors that play a role prior to hospitalisation