Antecedentes: Las guías K/DOQI recomiendan el uso del ratio fósforo/proteína de los alimentos para un buen control del fósforo de la dieta. Existe evidencia de tablas con el ratio fósforo/proteína. No existe hasta el momento una tabla de alimentos habituales en la población española con la estimación del ratio. Objetivos: Estimar el ratio fósforo/proteína de alimentos de uso general en la población española y establecer su utilidad en la selección de alimentos para los pacientes con enfermedad renal crónica. Método: Las tablas con el ratio fósforo/proteína se han elaborado a partir de dos fuentes de datos de composición de alimentos españolas. Se ha considerado la composición química por cada 100 g de alimento crudo. Las tablas no incluyen el fósforo de los aditivos. No se eliminaron los alimentos con ratio fósforo/proteína elevado para poder establecer una comparación entre los distintos alimentos de cada grupo. Resultados: Se encuentran comprendidos en las tablas. Conclusiones: La prescripción dietética de los pacientes con enfermedad renal crónica debería tener en consideración no solo el valor absoluto de fósforo del alimento en cuestión, sino también el ratio fósforo/proteína de cada alimento y el total de la dieta. Cuanto más «natural» sea la dieta, más fácil será que alcance un ratio fósforo/proteína aceptable y mayor probabilidad de ser menor de 16 mg/g, no aumentando la morbimortalidad. Resulta evidente la necesidad de establecer un programa educativo sobre fuentes de fósforo y nutrición en el que la tabla pueda ser una herramienta útil para el equipo multidisciplinar que atiende al enfermo renal.
Background: The K/DOQI guidelines recommend the use of phosphorus/protein food ratios for proper control of dietary phosphorus. Evidence exists from tables with phosphorus to protein ratios for common foods. No such table exists for common foods consumed by the Spanish population with ratio estimations. Objectives: To estimate the phosphorus to protein ratio in foods commonly used by the Spanish population and to establish its usefulness in the selection of foods for patients with chronic kidney disease. Method: Tables with the phosphorus to protein ratio were prepared from two data sources concerning Spanish food composition. We evaluated chemical composition per 100g of raw food. The tables do not include phosphorus additives. No foods with high ratio of phosphorus to protein were eliminated in order to allow comparisons between different foods from each group. Results: Shown in the tables. Conclusions: The dietary prescription for patients with chronic kidney disease should take into consideration not only the absolute phosphorus value of food consumed, but also the phosphorus to protein ratio of each food and the total amount of phosphorus in the diet. The more "natural" a diet is, the more likely that the patient will reach an acceptable phosphorus to protein ratio of less than 16mg/g, which does not increase mortality. There is clearly a need for an educational program on nutrition and phosphorus sources in which food ratio tables could be a useful tool for the multidisciplinary teams caring for renal patients.
INTRODUCTION
Hyperphosphatemia in patients with chronic kidney disease (CKD) contributes to the development of bone mineral metabolism disorders, constituting an independent risk factor for morbidity and mortality in patients on dialysis.1-4
Deteriorated renal function provokes retention of certain substances such as phosphorus, as an adaptive mechanism to the functional loss of nephrons in the context of glomerular-tubular balance. Phosphorus retention can start in early stages of CKD (as a probable occurrence in stage 1 and definitely in stage 2), progressing to hyperphosphaturia and hyperphosphatemia in stages 4 and 5.5,6
Diet restrictions to limit phosphorus intake must be started when serum levels of parathyroid hormone (PTH) start to increase (stage 2) and/or when serum phosphorus levels are elevated, regardless of stage.5 Restricted phosphorus diets are an appropriate measure to take in stages 1 and 2 of CKD, since these stages can be associated with phosphorus retention, increased fibroblast growth factor 23 (FGF-23), and hyperphosphaturia.6
Serum phosphorus levels may also be elevated in stages 4 and 5 of CKD, requiring phosphorus restrictions (if these have not already been put into place) in order to control serum phosphorus, FGF-23, and PTH levels.5 In stage 5 (patients on dialysis), increased serum phosphorus levels are one of the main health complications. One of the primary treatment strategies for this condition is restricting the consumption of foods rich in phosphorus, without compromising proper consumption of proteins.6
The treatment strategies classically used to control phosphorus levels include diet restrictions, decreased intestinal absorption rates through the use of chelating agents, and phosphorus purifying techniques in renal replacement therapy (if therapy has already been started). Despite this, it is difficult to maintain proper serum phosphorus levels, with the possible complication of vascular calcifications, a direct cardiovascular risk factor associated with increased morbidity and mortality rates.7
Hyperphosphatemia has been associated with difficulty in reducing phosphorus intake while maintaining adequate protein intake, difficulties in adequately purifying dietary phosphorus from the blood in standard haemodialysis (HD) regimens (and to a lesser degree, peritoneal dialysis [PD]), and improper compliance for various reasons with phosphate binder prescriptions.2
A complete understanding of the different phosphorus sources (organic and inorganic) is essential for the clinical and dietary management of patients with CKD.7 This involves an awareness of the different possible phosphorus sources, the bio-availability of each, and the importance of estimating phosphorus/protein ratios, which facilitate proper phosphorus control while ensuring sufficient protein intake.
The close relationship between phosphorus and protein content in common foods makes it difficult to plan a diet restricted in phosphorus without placing a restriction on protein intake, especially protein from animal sources. It is difficult to establish a diet of less than 1000mg/day of phosphorus due to the high protein needs involved, as well as the large quantities of phosphorus present in processed foods.8 In stage 5 of dialysis, reduced phosphorus intake should be accompanied by adequate protein intake and an optimal dialysis regimen.5
Taking into account this limitation, dietary phosphorus should be as low as possible, while ensuring adequate protein intake.5
The K/DOQI guidelines recommend a daily phosphorus intake of 10-12mg per gram of protein, or a mean value of 12-16mg phosphorus/g of protein.9 In order to achieve this goal, the patient must select foods that are good sources of protein but that contain the lowest content possible of phosphorus. One method for determining dietary phosphorus intake is by utilising this average.5
Dietary phosphorus intake is very commonly underestimated. Food tables do not reflect the phosphorus contained in additives. These variations in phosphorus content make it difficult for nutritionists or health care personnel to accurately estimate phosphorus levels in foods.7 In addition, food producers are not obligated to present phosphorus content in food labels.10
Since protein intake is an important component in the treatment of patients with CKD, and since foods rich in protein are also sources of organic phosphorus, the most appropriate method for estimating phosphorus intake is the Phosphorus (mg)/protein (g) ratio of a given food. In this manner, we can ensure provision of the necessary protein content associated with the lowest possible phosphorus content.5,7,11,12
The K/DOQI guidelines recommend using this ratio because of several advantages5,7,12:
- The ratio is independent of the portion consumed.
- The ratio refers to both phosphorus and protein content, both of which are important in the nutrition of CKD patients.
- The ratio is high for foods with high phosphorus content in additives, but with the same amount of protein.
- Its use allows for consuming foods with an adequate ratio, when assessing these foods based solely upon phosphorus content would exclude them from the diet of a patient with CKD.
- The ratio singles out foods with excessive phosphorus content and low protein content.
The disadvantage of using the phosphorus/protein ratio and absolute phosphorus levels is that these methods do not provide information regarding bio-availability or intestinal absorption of phosphorus that is derived from different types of foods. However, these remain useful tools for dietary management and education of patients with CKD.7,12
Brazilian medical guidelines recommend expanding the consumption of foods with the lowest possible phosphorus/protein ratio and minimising the consumption of foods that contain phosphorus in the form of additives (phosphoric acid, polyphosphates, and pyrophosphates).11
Risk of death is greater in patients on HD who maintain a total dietary phosphorus/protein ratio above 16mg/g.13
Evidence also exists that nutritional education regarding additives commonly found in foods produces a significant reduction in phosphataemia values among patients on HD.3 A food education programme would provide better awareness at the moment of selecting foods based on phosphorus/protein ratios, thus achieving a better control of phosphorus values, general nutritional parameters, and bone mineral metabolism in patients with CKD.14
Food tables have been published in the medical literature providing phosphorus/protein ratios.2,5,7,8,12,15-17 However, until now, no phosphorus/protein tables have been elaborated based on food consumption in Spain.
OBJECTIVES
To estimate the phosphorus/protein ratio of foods commonly consumed by the Spanish population and to establish the usefulness of these ratios in the selection of foods by CKD patients.
METHOD
We created phosphorus/protein ratio food tables using the information provided by two different sources regarding the nutritional composition of foods:
- The Spanish database of food contents (BEDCA), which forms part of the EuroFir network of excellence and has been approved by the Spanish Ministry of Science and Innovation and the Ministry of Health and Public Policy.18
- The Mataix Verdú food tables elaborated by the University of Granada.19
Chemical composition was determined based on 100g of raw food. In order to facilitate the analysis, we formed different food groups. Based on the value of phosphorus (milligrams) and protein (grams) in each food, the phosphorus/protein ratio was estimated. The tables do not include phosphorus content in additives, since the primary food content sources have not analysed phosphorus levels in additives.
We did not eliminate foods with a high phosphorus/protein ratio in order to establish a comparison between the different foods in each group.
We also included the potassium and sodium content of each food, since these are other basic dietary components that these patients must monitor. The tables include the content of raw foods, not taking into account processing techniques that might decrease potassium levels.
DISCUSSION
Appropriate serum phosphorus levels decrease morbidity and mortality rates in renal patients (cardiovascular risk and bone mineral metabolism disorders), which indicates the need for treatment strategies to ensure proper control of this parameter. The basic strategy is to apply multiple educational approaches (food plans + correct use of phosphate binders, etc.), along with the most appropriate dialysis technique, whether HD or PD, as well as choosing the optimal phosphate binder for compliance with the prescription.
In terms of dietary phosphorus sources, there are two different forms of phosphorus that have different implications for phosphataemia: organic phosphorus and inorganic phosphorus.
Organic phosphorus is found naturally in protein-rich foods, both from animal and plant sources. Organic phosphorus is hydrolysed in the intestinal tract and then absorbed as inorganic phosphorus.8 In general, only 30%-60% of organic phosphorus is absorbed, depending on the digestibility of the nutrients, the dietary bio-availability of the phosphorus, the level of activation of gastrointestinal vitamin D receptors, and the presence or absence of components that could bind to phosphorus or interfere with their absorption, such as aluminium or nicotinic acid.7,8,12
Phosphorus derived from animal proteins is stored within the cells, and is easily hydrolysed and absorbed. The primary phosphorus sources of this kind are red meats, poultry, fish, eggs, and dairy products. Animal-derived phosphorus is more digestible than phosphorus derived from plant sources.7,12
Organic phosphorus in plants is found in seeds, nuts, and legumes, in contrast to fruits and vegetables, which have only trace amounts of this mineral.7
Unlike phosphorus from animal protein sources, which is stored within the cells, phosphorus derived from plant protein sources is stored as phytic acid or phytate. Humans do not possess the enzyme phytase, making plant-derived phosphorus relatively unavailable biologically, usually less than 50%.7,8,12
In individuals without CKD, if the same quantity of phosphorus is ingested from both animal and plant protein sources, urine phosphorus excretion is greater in diets rich in animal protein, which would indicate that in patients with CKD, a greater intake of plant-derived protein would not necessarily cover all the protein needs of the patient, but this would aid in improving the control of phosphorus levels. However, there are certain considerations to take into account. Firstly, the biological quality of plant-derived protein is inferior to that of animal-based protein, and so in individuals with protein deficiencies, this type of diet might provide insufficient protein. It is also important to point out that we have yet to elucidate the effects that probiotics could have on phosphorus levels due to the presence of the enzyme phytase, which could influence the absorption of phosphorus from plant-derived sources.7
Inorganic phosphorus is the primary component found in several food additives that are used in the processed foods industry.20 Common sources of inorganic phosphorus are bottled drinks, frozen foods, breakfast cereals, processed cheeses and cheese spreads, instant products, precooked meals, sausages, crackers, pastries, cola products, etc.3,7,10,11,21
Inorganic phosphorus is not bound to proteins, and is found in the form of salts (polyphosphates, phosphoric acid) that are easily dissociated, making this form of phosphorus quickly absorbed in the intestines.20 Between 90% and 100% of inorganic phosphorus is absorbed by the intestines, as compared to 40%-60% of organic phosphorus naturally found in foods.4,7,10,12,22
In this manner, additives have a greater impact on hyperphosphatemia than a similar quantity of naturally derived organic phosphorus.3,23,24
Sullivan et al. observed a significantly greater difference between Phosphorus values obtained from chemical analysis and those from food tables if comparing the same foods that were treated with additives. The authors concluded that food tables do not reflect the true phosphorus content of these foods, since they do not take into account the phosphorus contained in additives. In addition, the lists of ingredients found in fast foods are often incomplete, making it difficult to identify the phosphorus content derived from additives. A simple awareness of foods that contain Phosphorus does not allow for a precise estimation of the true content of this element.4 As a result, total avoidance of processed foods is ideal.
The amount of phosphorus contained in animal-derived protein sources varies.2,7 We must also point out that phosphorus from non-protein sources varies widely and is generally high.2
Phosphorus/protein ratios vary widely between different protein sources, which would suggest that phosphorus intake can be reduced while still maintaining an adequate protein intake.2
Dairy products are a challenge for nutritionists.25 In the case of milk, there is virtually no difference in terms of phosphorus content between whole milk, 2%, or skim milk, all of which have a high ratio (Table 1). However, 2% milk is recommended, since this has the lowest phosphorus/protein ratio and the lowest potassium content as compared to whole or skim milk, and provides a good source of fat-soluble vitamins. Despite the fact that soy milk has a lower phosphorus/protein ratio than 2% cow’s milk (14.68mg/g vs. 26.56mg/g), soy milk may also contain phosphorus additives.25
Different types of cheese can contain a wide range of phosphorus levels, which may be organic or inorganic in nature depending on the processing methods used.7 Cottage cheese and spreadable cheeses are good options, especially for patients whose calorie and protein requirements are high (Table 1).
Egg whites, which are sources of protein with a high biological value and a protein digestibility corrected amino acid score (PDCAAS) of 97%,26 have an ideal Phosphorus/protein ratio (1.42mg/g protein), and also do not contain cholesterol, making this a healthy source of protein for patients on dialysis. In contrast, egg yolks have a high ratio and contain large quantities of cholesterol (Table 1).7,12,18
Red meat, pork, and poultry all have low quantities of phosphorus (mean 9.2mg/g protein) along with large quantities of high-quality protein, making these, along with egg whites, optimal sources of dietary protein.18
When choosing meat products for inclusion in the daily diet, patients should be careful about precooked or cured meats, and those with additives. Oftentimes, fresh meats are injected with a solution of water, sodium, Phosphorus, potassium, and antioxidants.15 This type of meat provides the consumer with a quick solution for daily food planning. In addition, additives maintain the integrity of the meat during cooking. Phosphate salts help maintain good colour, retain moisture, and prevent the meat from going rancid, which means that meats with these additives have a longer shelf life and present a more appealing image to consumers. However, these meats provide high quantities of sodium and phosphorus.8 Currently, there is no practical way of knowing the exact amount of added phosphate present in these meats. Nutritional labelling does not require a description of phosphorus content or the type of phosphate salt used in food processing, making this information the sole property of food producers.27
The phosphorus/protein ratio varies for fish, crustaceans, and other seafood (ranging from 7.53mg/g to 23mg/g), and guidelines recommend consuming only those foods with a ratio <16mg/g. Salmon has always been considered as a fish with a high absolute phosphorus content. However, it has an acceptable ratio of 13.58mg/g, lower than flounder or pout (Table 1).18 Frozen fish is pre-treated with a sodium polyphosphate solution prior to freezing in order to prevent the loss of protein during the thawing process, and this added phosphorus content should be taken into account when purchasing foods.8
Whole eggs, legumes, breakfast cereals, milk, cheese, yogurt, nuts, and precooked foods tend to have a high ratio (Table 1, Table 2, and Table 3). However, phosphorus contained in legumes and nuts comes in the form of phytic acid, and so is associated with a decreased rate of intestinal absorption. Even so, we must keep in mind the high potassium content of legumes, nuts, and certain cereals, which creates the need for including potassium content information in food tables.18
Ham, which is widely consumed in Spain, does have acceptable ratios (3.64-12.57mg/g), although food tables do not include the phosphorus content of food additives that are found in this type of meat (known as “hidden phosphorus”). If these additives are taken into account, it is probable that the ratio would increase along with a higher biological availability of the phosphorus contained.18
Sauces, baked goods, and cereals contribute to phosphorus intake while providing only minimal amounts of protein with poor biological value (Table 2 and Table 3). Within the group of baked goods, the lowest ratios are found in cookies without toppings and Maria brand cookies, which can be recommended as an occasional replacement for bread.
Chocolate is another important source of phosphorus, with an average ratio of 230mg/100g of food (Table 3).18
Cola drinks contain high amounts of inorganic phosphorus, in addition to phosphate salt additives used to improve flavour.8
The low bio-availability of the phosphorus contained in vegetable proteins is an advantage when designing a diet with a low phosphorus intake.8 In a plate of 50g of white rice and 50g of lentils, there is approximately 16g of protein and 180mg of phosphorus. However, only 30% of the phosphorus would actually be absorbed (54mg). In contrast, the same quantity of meat-derived protein would provide more phosphorus. For example, 100g of flounder would contain 16g of protein and 260mg of phosphorus, and 16g of protein from chicken breast would contain approximately 140mg of phosphorus. For this reason, a mixed diet is recommended in which an average 60% of the phosphorus contained in food is actually absorbed.
A diet primarily based on fast food and processed meats as the major sources of protein would involve a greater intake and uptake of phosphorus than a similar diet based on fresh, unprocessed foods, which contain only naturally occurring forms of phosphorus.8
It would be a major advantage for patients with CKD to have information provided on nutrition labels regarding the added phosphorus content of each food. However, in the absence of this information, wary consumers should closely read the ingredients list on food labels and choose only those foods that do not contain phosphorus-based additives.2,8
Techniques such as submerging foods in water or boiling them could also help reduce phosphorus content.8,28
Patients with CKD must receive training regarding “hidden sources” of phosphorus, such as precooked meats with additives. This could be facilitated by providing a list of locally found brands and their contents.27 In patient waiting rooms, educational materials could be provided indicating which foods contain hidden sources of phosphorus. Food lists and images provide a useful alternative for nutritional education of patients with CKD.22 The more a patient knows about the foods he/she eats and what they contain, the better the choices made will be.27
These tables do suffer the limitation that, in the absence of information from an analysis of phosphorus contained in additives, the true mineral content of foods that could contain these additives is hard to estimate. However, as a general rule, patients should select natural foods that are not processed and do not contain additives. Analysis of processed foods and the development of tables with corresponding phosphorus/protein ratios would be useful for renal patients, especially when selecting foods during special situations (eating out, social gatherings, etc.).
The dietary recommendations for patients with CKD must be made on an individual basis taking into account nutritional needs, tastes, and feeding habits during daily activities.29 Our efforts to restrict phosphorus intake should be concentrated on limiting foods with phosphorus-based additives, not foods with high protein content.4,20
In order to adequately control phosphorus intake in diet plans, we must implement education programmes and monitor patient compliance with diet restrictions. This requires multidisciplinary teams with an active participation of nutritionists in the care of patients with CKD.5 Specialised nutritionists in CKD should educate and encourage patients to read food ingredient labels with the specific goal of assessing phosphorus content.
To conclude, for patients with CKD, a mixed diet of foods with animal and plant-derived protein sources is recommended, while minimising the intake of processed foods that contain food additives.7 The more “natural” the diet, the easier it will be to reach an acceptable phosphorus/protein ratio (less than 16mg/g).
Diet restrictions for patients with CKD must take into account not only the absolute value of phosphorus contained in the food in question, but also the phosphorus/protein ratio contained in each food and the overall diet.7,13
Conflicts of interest
The authors declare that they have no conflicts of interest related to the content of this article.
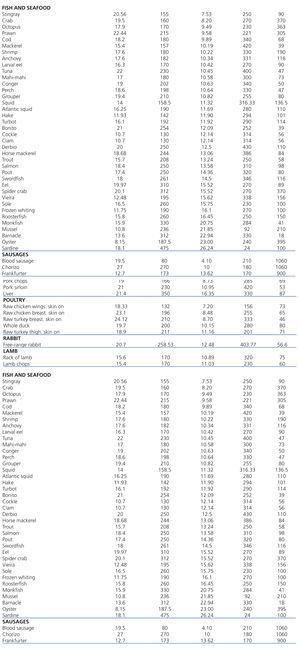
Table 1. Phosphorus/protein ratio per 100g of uncooked food from organic animal sources
Table 2. Phosphorus/protein ratio per 100g of uncooked food from organic plant sources
Table 3. Phosphorus/protein ratio per 100g of uncooked food from sources with inorganic Phosphorus