Los estudios que han analizado la supervivencia entre hemodiálisis y diálisis peritoneal han sido hasta ahora heterogéneos, con resultados a favor de una u otra técnica, y en muchos casos, confusos, lo que depende también de numerosos factores. Por dicho motivo, es necesario conocer si existen diferencias reales entre las dos modalidades, para situar a la evidencia científica como pilar fundamental en la elección del tratamiento, junto con las circunstancias clínicas de los pacientes concretos, sus preferencias y estilo de vida. Una revisión comparativa de la supervivencia entre técnicas de diálisis no puede eludir unas características o atributos metodológicos básicos, como ser de diseños adecuados, como los estudios observacionales de registros con grandes cohortes, con poblaciones incidentes y no prevalentes, con análisis por intención de tratar, análisis de supervivencia y análisis multivariantes con ajustes de las principales comorbilidades. Se han revisado los nueve estudios clásicos (poblaciones incidentes previas al año 2002) principales, que presentan unas conclusiones similares: globalmente no existen grandes diferencias entre las técnicas, con un comportamiento similar tanto en los grandes registros como en las cohortes prospectivas. Cuando se realizan una estratificación y un ajuste por comorbilidades, la diálisis peritoneal presenta un pronóstico equivalente o mejor en los grupos de pacientes no diabéticos, menos comórbidos y más jóvenes, prácticamente en todas las publicaciones, y la hemodiálisis en los diabéticos, de mayor edad y más comórbidos. De la misma forma, se detallan los resultados de los estudios recientes (que incluyen poblaciones incidentes posteriores al 2002), que llegan a la conclusión de que existe un comportamiento similar para la supervivencia entre hemodiálisis y diálisis peritoneal. De igual manera, la edad y la comorbilidad del paciente influyen en los resultados de forma casi idéntica a lo publicado en los estudios anteriores. En la última década hemos asistido en una mejora del pronóstico vital de los pacientes tratados en diálisis, más importante en los pacientes en diálisis peritoneal, tanto en EE.UU. como en Europa, Australia y también en España (análisis propio en Andalucía). Finalmente, y por medio de análisis multivariantes propios, podemos afirmar que la supervivencia del paciente en diálisis se ve mucho más influida por las condiciones al inicio de la técnica, como la edad, la presencia de diabetes o la enfermedad cardiovascular, que por el tipo de técnica en sí.
Studies that have analyzed survival between hemodialysis and peritoneal dialysis have showed heterogeneous outcomes for both techniques, and often confusing, also dependent on many factors. For this reason, it is necessary to know if there are real differences between the two treatments, to put the scientific evidence as a fundamental pillar in the choice of treatment, along with the clinical circumstances of individual patients, preferences and lifestyle of these. A comparative review of survival among dialysis techniques cannot avoid a basic methodological characteristics or attributes, such as appropriate designs such as observational studies with large cohorts, with incidents and no prevalent populations, with "intent to treat analysis "survival analysis and multivariate analysis with adjustments to the main comorbidity. We studied the nine classical main studies (incidents before 2002), presenting similar conclusions: there are no major differences between the techniques outcomes. When performing a stratification and adjustment for comorbidities, peritoneal dialysis has a equivalent or better prognosis in the nondiabetic group, less comorbidity and younger, almost all the publications, and hemodialysis in diabetics, older and more comorbid groups. The recent studies (including incidents after 2002), concluding a similar behavior for the survival HD: DP. Similarly, age and comorbidity influence the patient's outcomes almost identical to previous studies. In the last decade has seen an improvement in the prognosis of patients on dialysis, more pronounced in PD patients, both in the U.S., and Europe, Australia and in Spain (Andalusia analysis also). Finally, by multivariate analysis, we can show that patient survival on dialysis is much more influenced by conditions at the beginning of the treatment, as age, presence of diabetes or cardiovascular disease, rather than the type of technique of dialysis.
A CONFUSING SITUATION
We are aware that medical factors are not the main determining factors for choosing which dialysis technique to use, which are funding and the unit’s or centre’s knowledge and experience. However, we must find out the actual differences in survival outcomes for each of the methods,1 so that scientific evidence can be used to support treatment choices, along with the patient’s clinical circumstances, preferences and lifestyle.
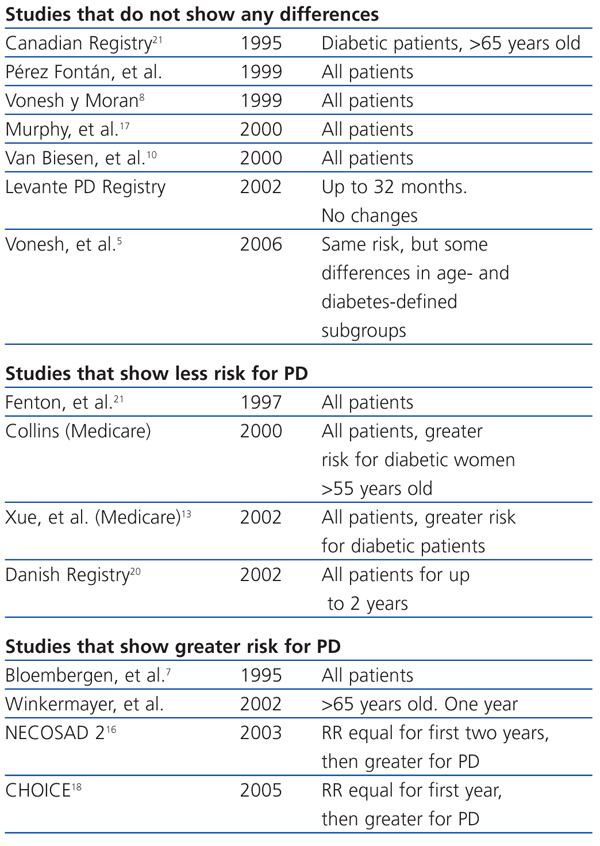
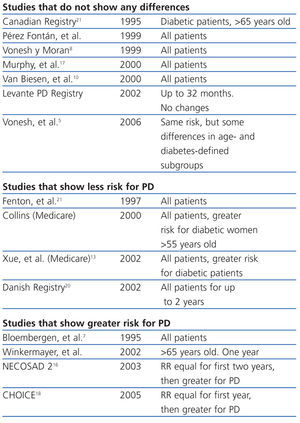
Peritoneal dialysis (PD) and haemodialysis (HD) results have been subject to several studies over recent years. The conclusions from these studies have been heterogeneous and on many occasions confusing, so much so that no significant or very slight differences have been found in favour of one technique or another (Table 1). This is due to multiple factors such as using records from very heterogeneous populations (single centre, multicentre, and even national), different study designs, incident or prevalent populations, and comparisons between studies regarding the necessary comorbidity adjustments.2
Some authors have even started to question how two so different techniques, such as HD and PD, can be compared,3,4 with the type of studies that are available.
As such, all comparative reviews of survival rates for these dialysis techniques must consider the methodological characteristics or attributes that should be included in good studies.5 The second section of this study will discuss this matter.
Therefore, and following this standard practice, we shall discuss at great length the main classic studies’ results (incident populations before 2002), that are well designed and which compare both replacement therapies. We also present the conclusions from new studies (incident populations after 2002) as well from our own research.
METHODOLOGICAL ATTRIBUTES RECOMMENDED FOR STUDIES COMPARING HAEMODIALYSIS AND PERITONEAL DIALYSIS
It is well known that controlled and randomised studies provide the most scientific evidence. However, we have only found one study with these characteristics that compares dialysis techniques in the literature, and it had poor extrapolative results due to an unsuccessful inclusion of patients.6
Following the level of evidence scale, the observational prospective cohort studies would, in principle, have to be well designed to be able to assess the differences between HD and PD in the long term. However, there are very few of them, given that their prospective design would not allow treatment transfers or substantial modifications in techniques, so as not to alter the final result. Furthermore, they need to use large samples, population subgroups, as well as long follow-up, etc.
Therefore, for this type of analysis, observational studies of registries with large cohorts of patients are mostly used. They must take into account certain important considerations.
Incident patient populations should be analysed, because if we include prevalent patients, then early mortality is excluded. This would therefore have an effect on the PD outcome, and would produce a significant bias.7,8
Populations can influence the results depending on their geographical origin, demographic or risk characteristics, health systems, or centres’ experience. Furthermore, results are not easily extrapolated to different populations.9
Statistically analysing these comparisons is complex and includes clinically important interactions, which have already been identified in several studies: the relative risk (RR) for survival-related events between PD and HD changes over time, according to age, diabetes and comorbidity. As such, PD-treated patients are at lower risk during the first years of dialysis, which is more apparent in younger, non-diabetic patients that do not have associated diseases.
Intention-to-treat statistical analysis should be performed to stop transfers from influencing the results. But ideally both intention-to-treat and non-intention-to-treat analyses should be used.
The most used statistical techniques for these analyses are Kaplan-Meier curves and Cox regression.10,11 The latter allows us to perform multivariate corrections and adjustments for comorbidities, as also occurs for the Poisson regression. All of which reach similar results in studies comparing PD and HD survival outcomes.12
Finally, we must mention that the adjustment for comorbidities must be as wide as possible, and it must include factors that are more widely known for their influence on patient survival, such as older age, diabetes mellitus and cardiovascular disease.13,14 That is why the absence of some of these adjustments in the analysis leads to an important bias and incorrect results.
MAIN RESULTS OF CLASSIC STUDIES (INCIDENT POPULATIONS BEFORE 2002)
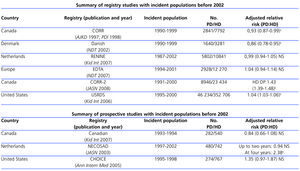
We have analysed nine of the most relevant studies with incident populations before 2002, which fulfil the recommended methodological attributes described, identifying some key results that must be commented on.
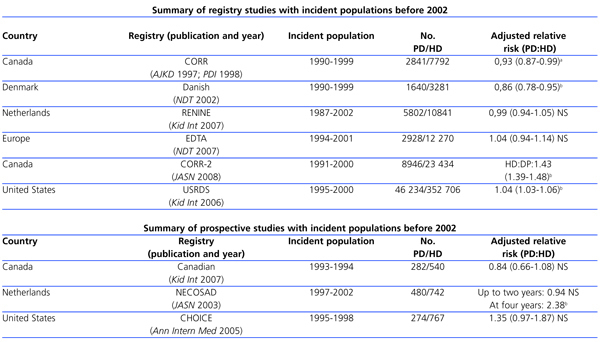
When comparing survival between HD- and PD-treated patients, there are no great overall differences, and large registry-based studies and prospective cohorts behave in a similar manner. Vonesh published a study in 2006 on large registry-based studies (Table 2) which showed that when the differences between the populations are adjusted, the outcomes are very similar among these studies.5,15 The main prospective cohorts (Table 2) are NECOSAD (Dutch),16 the Canadian study by Murphy,17 and the CHOICE study.18 No significant differences are found between the NECOSAD and the Murphy studies and the Dutch and Canadian registries. The CHOICE study presents some very conflicting results compared with the prognosis of the same patient subgroups from the US Medicare population. This could be explained by the low statistical power that this study has, and by the severe bias in choosing participating centres (90% were recruited from a single provider).
When a stratification and adjustment for comorbidities is performed, PD presents an equivalent or better prognosis in groups of younger, non-diabetic patients with a less comorbidities scores, in almost all publications.14,19
However, HD, especially in studies with American populations, and slightly less in Dutch studies, presents a better survival prognosis for older, diabetic patients, with worse cardiovascular diseases. The American registry states that age is relevant to patients over 45 years old and the Dutch register over 60 years old.
When considering the time that patients have been undergoing dialysis treatment, we must point out that all studies show that initial survival is greater for PD. Some analyses15 show that this difference decreases over time, and that HD is more favourable than PD after the first or second year, whereas others show that this initial advantage is maintained over a longer period, and even that there are no significant differences in favour of HD not even at the end of the follow-up, as is shown in the Danish registry20or in the Canadian registry published by Fenton in 1997,21 and later by Yeates in 2008.22
MAIN RESULTS OF RECENT STUDIES (INCIDENT POPULATIONS AFTER 2002)
The ANZDATA23 Registry (Australia and New Zealand registry) has an incident population of 25 287 patients from 1991 to 2005 (HD: 14 733; DP: 10 554). Adjusted for age, sex, body mass index (BMI), diabetes and comorbidity, it shows similar results to other, above mentioned studies that compare HD:PD survival. This registry also shows that PD is better for all diabetic patients and non-diabetic patients, of any age, but only until the second year. In the third and forth year HD has a better prognosis. Similarly, the patient’s age and comorbidities influence the results almost identically to previous studies.
A very recent publication24 from 2011 the European Renal Registry Investigators (ERA-EDTA) analyses comparative survival rates for incident populations from 1999 to 2003, adjusted for age, sex, and underlying kidney disease. Its results are the same: the PD-treated population had a better survival outcome than HD patients, which was maintained until the third year, and HD was slightly better in the forth and fifth years.
In 2010, Weinhandl et al25 published the results from a retrospective cohort of incident patients from 2003 in the USA (n=98 875) comparing the survival rates for both techniques, HD (n=92 187) and PD (n=6688). To do so, they designed a methodology which matched DP patients with their HD pairs according to factors such as age, sex, race, underlying kidney disease, laboratory data and most important comorbidity. Six thousand three-hundred and thirty-seven propensity-matched pairs were therefore obtained and followed until December 2006. Two types of intention-to-treat analyses were performed: one taking into account the type of dialysis on day 0 of replacement therapy, and the other on day 90. Later, subgroups according to age, cardiovascular disease and diabetes were created. In the analysis which considers the technique on day 0, the cumulative death risk at 4 years was 8% less for PD (P<.04). This difference was more important for patients under 65 years, with no cardiovascular disease and diabetes, and similar for patients over this age, with cardiovascular disease and diabetes. In the analysis for survival after 90 days, survival was also greater for PD patients than HD patients, with no statistical significance.
In the last decade we have observed an improvement in the vital prognosis of dialysis-treated patients, especially for PD patients. This is also shown in the Registro Español de Enfermos Renales (Spanish Registry of Renal Patients), in which the gross mortality rate has improved for PD patients in recent years. However, HD rates have not considerably changed, which is also described by Mehrotra et al26 in the USA registry in which prognosis improved significantly for patients treated between 2000-2003, compared to those from 1996-1997, with the same comorbidity and laboratory adjustments.
Likewise, this has been shown for the European population, e.g. in the ERA-EDTA study of 2009, published by Kramer et al27 in which PD survival at 2 years improved by 19% in the second period studied (2002-2006), compared to the first period (1997-2001). However, it continued to remain stable for HD during the same periods. This study is lacking good risk adjustments and stratification. Lastly, in the above mentioned ANZDATA23 Registry the results reported are almost the same.
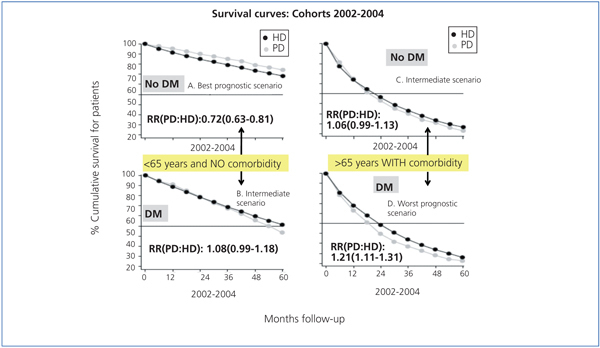
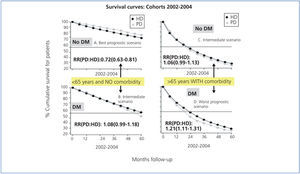
The recent Mehrotra et al28 study of 2010 (USA registry) deserves a more detailed analysis. It compares 3 cohorts related to the periods 1996-1998, 1999-2001 and 2002-2004. For the first time in an American cohort, no significant overall differences in PD and HD survival were detected after five years of follow-up using an intention-to-treat analysis. Subgroups stratified by age, diabetes and comorbidity had similar outcomes: PD had a better prognosis for younger, non-diabetic patients with no comorbidity, and HD was better for those over 65, with comorbidities and diabetes. Both extreme situations presented significance in its advantages for each technique. In the intermediate situations, there are no differences in favour or against either of the dialysis techniques (Figure 1).
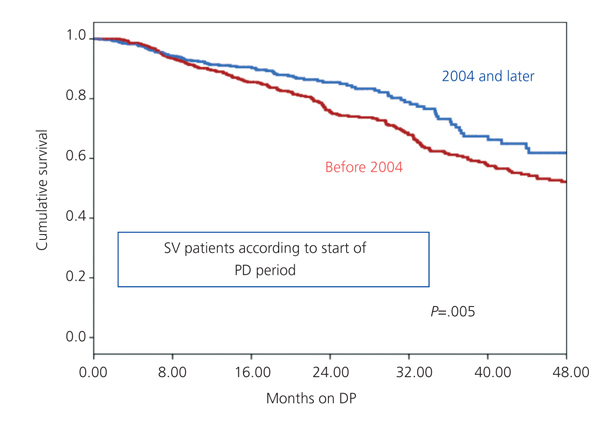
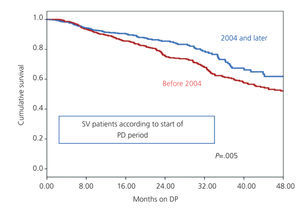
We have also observed this improvement in PD outcomes during recent years for the population treated in Andalusia, with adjustments for age, cardiovascular disease and diabetes. We observed a significantly better survival for incident patients from 2004 to 2008 compared to those from 1999 to 2003 (Figure 2).
Better PD results in more recent studies are likely the result of better peritoneal membrane protection as more biocompatible solutions, fewer high glucose concentrations and more adequate doses are used. In addition, centres are better experienced, volumes are better handled and complications, such as peritonitis, are more adequately treated.
As has been mentioned above, and based on multivariate analyses, we can state that the survival of patients on dialysis is much more influenced by the conditions at the start of the technique, (i.e. age, diabetes, cardiovascular disorder) than the type of technique itself.
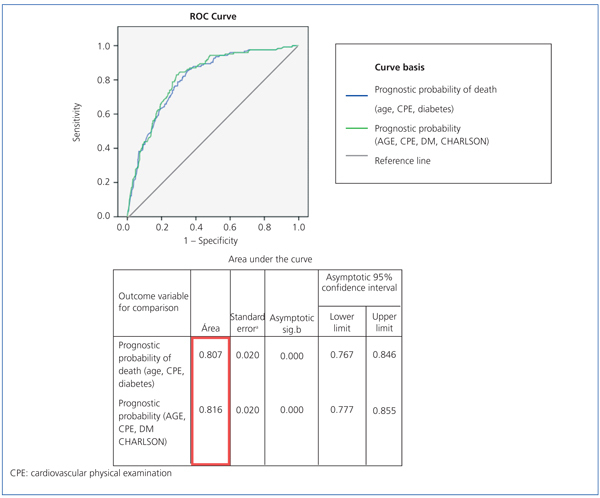
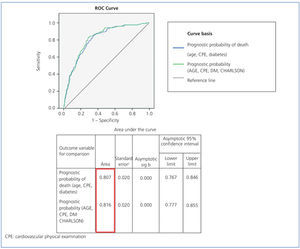
We know that the multivariate regression allows us to determine independent variables that influence the final results separately and that the ROC curves graphically represent the percentage of the phenomenon or the event studied (in this case death) which is explained by the variables considered (area under the curve). Therefore, by comparing different multivariate models created with more or less variables (or different variables) on a same outcome, we are able to find out which better explains the phenomenon. The aim is to find an efficient study and statistical method, i.e. find an adequate percentage to explain the result (always >50%) with the fewest variables possible. Therefore, a model with 3 variables which expresses a very similar percentage to one with 10 or 15 variables would be more efficient.
Using this methodology (Figure 3), we have analysed that the prognostic variable for death created by the group of risk factors present at the start of this technique, (age and cardiovascular disease and diabetes and the other comorbidities considered in the Charlson’s comorbidity index) would explain the 81.6% prediction in the multivariate model in our PD population. The variable created by age and cardiovascular disorder and diabetes would explain 80.7% (a difference of 0.9%).
Therefore, when statistically examining the probability of death, depending on certain independent comorbidity variables, including age (as a continuous variable), cardiovascular disorder and diabetes in this multivariate model is the most efficient technique. We can forget all the other variables included in Charlson’s index, as they would not provide very much information to the final prediction and would make data collection and analysis unnecessarily more complicated.
Therefore, there is very little margin for other variables such as the dialysis type and dose, anaemia, nutrition, etc., factors that undoubtedly influence outcomes, but whose absolute weighing is quite marginal. Furthermore, some are intermediate variables conditioned by the fundamental initial comorbidity.
CONCLUSIONS
Following these reflections, we have to conclude that survival outcomes of these dialysis techniques are equivalent, that their long-term results are similar and that fundamentally, the associated factors are those that have a greater impact on mortality for dialysis patients.29 The health centre’s experience with each therapy,30 and some patient conditions can influence these results, such as age, diabetes, therapeutic adherence, urgent or programmed dialysis, associated comorbidity, dialysis access complications, etc. Factors that determine a shorter survival, both for PD and HD patients, seem to be well defined and are similar for both therapies. Older age, diabetes mellitus and atherosclerosis-induced complications seem definitive31 and would explain, by a wide margin, most of the deaths in multivariate models, being more related to survival than the dialysis technique itself.32 Finally, time seems to have an important and well-demonstrated impact on outcomes, so much so that during the first years, patients with PD have a better prognosis than those undergoing HD, especially younger patients with fewer comorbidities. Furthermore, more recent patient cohorts have also had a very similar prognosis for the two therapies in the medium term, and PD results have improved during the past decade.
Table 1. Heterogeneous conclusions in survival studies comparing haemodialysis and peritoneal dialysis
Table 2. Main results from classic studies
Figure 1.
Figure 2. Improvement in PD prognosis in our environment during recent years
Figure 3. Sensitivity and specificity study using ROC curves (see text.)