Antecedentes: A pesar de los resultados discrepantes en estudios españoles sobre costes de diálisis, se asume que la diálisis peritoneal (DP) es más eficiente que la hemodiálisis (HD). Objetivos: Analizar los costes del concierto de HD y DP en Galicia y su valor añadido, los del transporte sanitario para HD y la relación en diálisis peritoneal continua ambulatoria (DPCA) con bicarbonato entre el coste del concierto y el del fungible utilizado. Métodos: El coste de los conciertos y del personal se obtuvo de publicaciones oficiales. Los de DP y del transporte sanitario se calcularon con datos del servicio de salud de un mes, extrapolados a un año. El del fungible de DPCA fue facilitado por proveedores. El valor añadido se estimó con las inversiones generadas por cada concierto tratando 40 pacientes. Resultados: Expresados por paciente/año, los costes medios del tratamiento fueron 21.595 y 25.664 € en HD y DP, respectivamente; los del trasporte sanitario oscilaron entre 3.323 y 6.338 € y los del concierto y fungible de DPCA fueron 19.268 y 12.057 €, respectivamente. El valor añadido fue superior con el concierto de HD, destacando los puestos de trabajo generados. Conclusiones: No puede generalizarse la afirmación de que el coste de DP, muy influenciado por la prescripción, es inferior al de HD. Convendría revisar el coste adicional al fungible en el concierto de DPCA. El valor añadido generado por los conciertos de diálisis debería considerarse en futuros estudios y en la planificación sanitaria. Se necesitan más estudios controlados para conocer mejor esta cuestión.
Background: Despite the discrepancy in results from Spanish studies on the costs of dialysis, it is assumed that peritoneal dialysis (PD) is more efficient than haemodialysis (HD). Objectives: To analyse the costs and added value of HD and PD outsourcing agreements in Galicia, the medical transport for HD and the relationship between the cost of the agreement and the cost of consumables used in continuous ambulatory peritoneal dialysis (CAPD) with bicarbonate. Methods: The cost of the outsourcing agreements and the staff was obtained from official publications. The cost of PD and medical transport were calculated using health service data for one month and extrapolating it to one year. The cost of CAPD consumables was provided by the suppliers. The added value was calculated from the investments generated for each agreement treating 40 patients. Results: Expressed as patient/year, the mean costs for treatment were €21 595 and €25 664 in HD and PD, respectively. Medical transport varied between €3323 and €6338, while those of the CAPD agreement and consumables were €19 268 and €12 057, respectively. The added value was greater with the HD agreement, especially considering the jobs created. Conclusions: One cannot generalise that the cost of PD, which is significantly influenced by prescriptions, is lower than that of HD. It would be appropriate to review the additional cost to consumables in the CAPD agreement. The added value generated by dialysis agreements should be considered in future studies and in health planning. More controlled studies are needed to better understand this issue.
INTRODUCTION
The cost of renal replacement therapy (RRT) accounts for a very large percentage of the total cost of health services in Spain, despite being needed by a very small percentage of users of the health system.1,2 As such, it is very important to use all of the resources assigned to this treatment as efficiently as possible.
In 2009 in Galicia, 46.10% of patients on RRT had a functioning kidney transplant (KT), some 45.4% were on haemodialysis (HD). Of them, 35% underwent HD in public centres and 65% were outsourced to centres with special agreements with the Health Department. Some 8.5% were treated with peritoneal dialysis (PD), according to the Chronic Kidney Disease Registry of Galicia (data from 2009). These percentages are similar to the mean data in Spain from the same year, with percentages of 47.51%, 47.67%, and 4.82%, respectively,3 except for the higher proportion of PD patients in Galicia.
In Spain, treatment with HD in public centres is financed from the budget that the public health system assigns to the hospital where the dialysis unit is located. In outsourced HD, the public health system charges a company with this responsibility in exchange for a predetermined reimbursement from the government. The provision of PD also takes place through an outsourcing agreement in which the public health system pays a company for the materials necessary for the treatment and a home delivery for the patients. This reimbursement is a fixed daily rate, also pre-established, for each type of treatment –continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD) with a cycler of approximately 15 litres– with a supplement for using special liquids: polyglucose or bicarbonate. In this type of outsourcing agreement, the public health system is responsible for financing health personnel and the necessary hospital facilities for training and supervising the therapy, in contrast to the HD agreement in which the companies contracted are required to do everything necessary to administrate and control treatment.
From a purely technical point of view, one can consider that both PD and HD are effective and safe for providing RRT4 with several details that fall outside of the objectives of this particular study. As long as no contraindications exist, a major consensus exists for recommending the use of the RRT method chosen freely by the patient, after receiving adequate and complete information regarding the advantages and inconveniences of the existing methods. It is also widely accepted that nephrology departments should provide both options for RRT, HD and PD, in order to provide the best option in any situation of clinical, personal, and occupational circumstances.
There is also a consensus among nephrologists regarding the importance of having the most efficient possible RRT in order to contribute to the sustainability of the treatment of chronic kidney disease. However, we still today have very little information regarding the true costs of RRT and which method of dialysis is the most efficient. In this sense, several studies have been published in Spain in recent years, using various methodologies, which compare the costs between hospital HD in public centres and PD, with disparate results. In some studies, HD appears to be a more economically feasible option than PD,5,6 and in others, it seems more costly,7,8 and in one of them, the cost of APD is higher than HD, with CAPD being cheaper than the latter, although with a similar cost to outsourced HD.9 Another study found that if only the technique is considered, CAPD is more expensive than HD.10
In spite of these contradicting results, there is a tendency to believe that PD is cheaper and more efficient than HD. In light of this opinion, a group of professionals a few years ago formed the group for the economic evaluation of renal replacement therapy (Grupo para la Evaluación Económica del Tratamiento Sustitutivo Renal), which has carried out several studies on the importance of developing PD for the sustainability of RRT, and recently headed the creation of the support group for the development of peritoneal dialysis in Spain (Grupo de Apoyo para el Desarrollo de la Diálisis Peritoneal en España) with the objective of increasing the use of this therapy, which they consider under-exploited and more efficient than HD, so as to improve the sustainability of the treatment of chronic kidney disease.
Since our perception of the efficiency of the different RRT based on our own experience was different from the opinion that PD is a cheaper option than HD, which resulted from a previous study regarding the costs of dialysis performed in our health area6 and the conflicting data available in the literature, we decided to analyse the costs of dialysis in our autonomous region with the following objectives:
1. To compare the costs of treatment with outsourced PD and HD, since this is the most widely used option of HD, and in order to avoid the confounding variables resulting from the different methodologies used in assigning costs in hospital HD programmes.
2. To evaluate the costs of health transport for HD, and to analyse their influence on the costs of outsourced HD agreements.
3. To analyse the total cost of consumables necessary for carrying out treatment with CAPD, and to calculate the difference between these costs and those of an outsourcing agreement.
4. To analyse the added value provided by outsourcing agreements for both types of dialysis in a health area.
METHOD
We carried out our study in the autonomous region of Galicia, in the North-eastern region of Spain, divided into four administrative provinces, with a total population of 2800 000 inhabitants.
The costs of outsourced HD were obtained from the rates (current in June 2010) paid by the health department for HD agreements using bicarbonate in dialysis centres, published in the Official Gazette of Galicia (Diario Oficial de Galicia).11
The costs obtained for PD were:
1. Rates of the agreement, current in June 2010, that were paid by the health department for the different techniques involving PD and its supplements, published in the Official Gazette of Galicia.11
2. The costs associated with the necessary personnel for maintaining a PD programme, calculated using the ratios of health personnel/patient (one nephrologist per 35 patients and one nurse per 20 patients) recommended by the guidelines established by the Spanish Society of Nephrology (S.E.N.) for clinical practice in peritoneal dialysis12 and using the costs in Galicia in June of 2010, including social security, incurred by the medical and nursing staff with a mean experience of 15 years. These data were facilitated by the human resources department at the University Hospital Complex of Vigo, and based on the Official Gazette of Galicia regarding the salaries of statutory staff.13
3. The costs of the peritoneal catheter and extensions, not included in the dialysis agreement and borne by public hospitals, according to the supplies department of the University Hospital Complex of Vigo.
4. The data regarding the true use of CAPD, automated PD, and special liquids in Galicia, facilitated by the provincial sections of the Galicia Health Department for the four different provinces. These data correspond to the month of October 2010 and have been extrapolated 12 months in order to calculate the yearly cost.
The cost of health transport in HD patients has been obtained from the data available for the four provincial sections of the health department regarding the rates paid for HD health transport in October 2010, which were extrapolated 12 months in order to estimate the annual consumption rate.
The prices for consumables used for CAPD were obtained from the Fresenius Medical Care catalogue 2010 regarding public retail prices plus VAT, and for the initial materials provided and monthly small consumables, we used the data provided by the company, and the costs of acquisition paid by the University Hospital Complex of Vigo. We estimated a mean technique survival of three years in order to calculate the yearly costs.
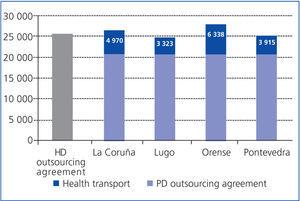
We defined added value for the health system as an economic growth produced as the consequence of establishing a dialysis outsourcing agreement, and estimated these values based on the investment made and positions made available by an agreement for the treatment of 40 patients on PD or HD, at a centre with 2 daily shifts, using the health personnel/patient ratios recommended by the S.E.N. guidelines for clinical practice in peritoneal dialysis12 and haemodialysis14 centres.
RESULTS
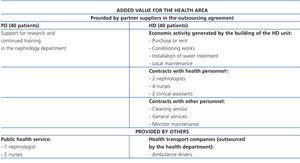
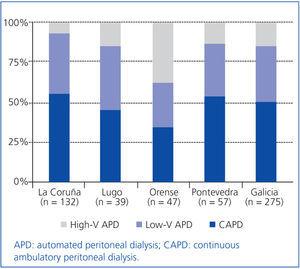
In October 2010, 275 patients were registered in Galicia on PD programmes, 50% of which were on CAPD, 35% on low-volume APD, and 15% on high-volume APD, with marked differences between the different provinces (Figure 1). In this group, 49% used supplements with polyglucose, and 64% used dialysate with bicarbonate (Figure 2).
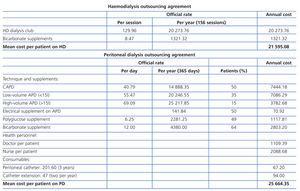
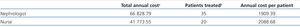
The mean cost of treatment per patient and per year in Galicia under the HD and PD agreements was 21 595.08€ and 25 664.35€, respectively (Table 1). This table also shows the rates of the agreements from June 2010 for outsourced HD at a dialysis centre and for PD. Table 2 shows the annual costs per patient on PD with one nephrologist or one nurse with 15 years of experience (data from June 2010).
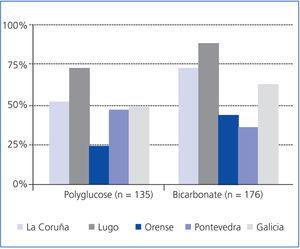
The costs of health transport for HD ranged between 3323€ in the province of Lugo and 6338€ in Orense. The influence of these values on overall costs of treatment can be observed in Figure 3.
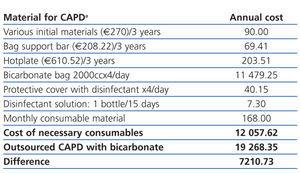
Table 3 shows the costs (June 2010) of the consumables necessary for CAPD treatment with four exchanges per day of 2000ml and the use of bicarbonate, the cost of outsourcing the technique and the differences between them.
Table 4 shows the added value for the health area generated by the companies in the DP and HD outsourcing agreements for the treatment of 40 patients.
DISCUSSION
In this study we have shown that if we only take into consideration purifying treatment, the cost of PD in Galicia with the current prescription model is higher than outsourced HD. If we include the cost of health transport for HD, the costs of PD are lower in two provinces, although they remain higher than outsourced HD in the other two.
We can also observe that if we only consider CAPD, the cost would be lower than in outsourced HD. This could possibly explain why PD appeared to be a cheaper option in the first comparative studies of health costs, as the majority of patients were being treated with CAPD without special liquids. However, with the current use of APD and these liquids, it is obvious that the total costs associated with PD are higher than HD, in our case, by 18%.
This study also concludes, as observed in other published studies,10 that the possible economic advantages of PD, if any, are not due to the fact that this technique is cheaper than HD, but rather the effect of adding other concurrent costs to those of purifying treatments, primarily health transport and erythropoietic agents. This will have to be re-evaluated using updated values, due to the more efficient management of health transport, and the lower costs and needs for these agents, given their price decrease and the lower target values for haemoglobin, as well as the use in HD of more biocompatible membranes and dialysates with a higher purity.
In our case, if the criteria for financing health transport were unified (the costs are currently quite different between provinces, which is difficult to explain simply in terms of geographical and communication differences) for improving their efficiency, and if the tendency to increase the use of APD and special liquids continues, the cost of an outsourced PD agreement will surpass that of an HD agreement with health transport in all provinces.
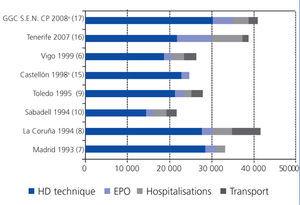
Data similar to ours, showing that PD was more expensive than HD have already been published in studies comparing PD and HD in hospitals,5,6 in which the repercussions that personnel costs incurred by nephrology departments and the use of APD with special solutions have on PD programmes had already been considered. Other studies had already observed higher costs in APD than HD9 and even in CAPD compared to HD, if the purifying treatment was considered alone.10 In contrast, other studies have concluded that PD is more economically feasible than hospital-based HD,7,8 although we must point out that in these studies, the costs of HD were higher than in all other publications on the subject, 65% higher than the mean costs from other studies carried out at the time. Furthermore, in the first of these studies,7 hospital HD was compared only with CAPD, and in the second one8 health transport costs were more than twice as high as reported by other authors. Figure 4 shows the important differences between the cost of public hospital HD and the health transport costs of HD for the different studies published in Spain.6-10,15-17
We believe that the uneven results from the different studies published on the costs of dialysis are due to the difficulty in estimating the costs associated with public hospital HD because of the different methods used to calculate these values (probably with over-estimated general costs in large hospitals, with very different costs of consumables depending on the type of HD performed, and costs of financing, depreciation, and other “hidden” costs [such as continuous training] in the price of consumables) and the different costs of transport in each area. We have tried to avoid all of these confounding elements in our study by comparing outsourced HD with PD.
The avoidance of these confounding elements should not be interpreted as our acceptance that public HD is undoubtedly more expensive than outsourced HD. The recent article by the quality control group of the S.E.N.17 and another previous publication9 would support this hypothesis, but we must also point out that the cost of public HD in the first of these studies was among the highest mentioned in the medical literature (Figure 4), even if it is adequately corrected for inflation. When performing this adjustment of the data, we must take into account that the costs of consumables and erythropoietic agents have stabilised and even fallen, and that salary raises have been lower. We must also point out that in a previous study, we were able to show how proper management can make HD at a public centre competitive with outsourced HD.6 In any case, more studies will be needed with a greater number of centres included in order to clarify this topic.
In spite of the discrepancies referred to in these studies regarding the costs of dialysis, some authors have estimated the future costs of RRT in Spain, based on theoretical models and retrospective data specific to each sample population from other studies performed on various topics with different methodologies and different time periods, areas, and countries with different practices, results, and types of financing. They concluded that PD was more efficient than HD, is underutilised, and its use should be expanded.18,19 Setting aside the methodological difficulties of these two studies, we are in accordance with their last two conclusions, but our data oblige us to re-define the first. In any case, we believe that the economic conditions of treatment should not be a deciding factor in choosing which technique of dialysis to use. Without forgetting the objective of maximum efficiency, the priority criteria should be quality health care and an improved process of the patient choosing which type of RRT is most adequate.20
In order to avoid these contradictory interpretations and results, future comparative studies of costs between different therapies should involve a homogeneous methodology, decided upon by a large group of nephrologists with different experiences and opinions that is financed with public funds. It also might help to avoid a division between HD and PD into two distinct and separate compartments. The two techniques should be considered complementary and equal, eliminating the risk of a possible bias in the approach of this subject by professionals dedicated exclusively to one type of dialysis or the other.
As regards the comparison of the costs of outsourced agreements for CAPD with bicarbonate in Galicia with the consumables needed for the technique, there is a difference of approximately 7210€ per patient per year in favour of the first, more than 37% of the cost of the outsourcing agreement. This value seems excessive for compensating for the administrative costs and the monthly supply of consumables sent to the patient’s house. There is also an important number of patients with three exchanges per day, which would reduce the annual cost of consumables by 2870€. This would mean that the previously mentioned difference would be raised to 10 080€ per patient per year (more than 52% the cost of the outsourcing agreement). We must also keep in mind that the costs of consumables are calculated at the public retail price, which already includes profit margins, and that the health system does not decided on them, which could reduce their amount.
We do not know which criteria were used when determining the rate of the PD outsourcing agreement, but in light of these data, it appears to be based more on the establishment of a price for treating CAPD that was considered “competitive” with outsourced HD than real costs and normal profit margins maintained by the suppliers. As such, it might be necessary to review this rate based on the effective costs of consumables and the process of providing the materials to patients, or to study how this is financed in other countries with lower costs for this therapy with the objective of improving efficiency.
As regards the added value for the health system from PD and HD outsourcing agreements, the companies in the PD agreements are limited to the provision and home delivery of the materials needed for the technique and the support for training and research in nephrology departments, whereas, the companies in HD agreements need to invest in the necessary buildings and infrastructure, acquire equipment, dialysis monitors, clinical material and consumables necessary for treatment, provide maintenance to all of this, and hire the personnel needed for daily functioning. Additionally, outsourced HD generates jobs related to health transport.
With all this in mind, HD outsourcing agreements generate an added value for the health system that far surpasses PD agreements, especially because of the economic benefits produced by directly creating jobs (Table 4). We believe that this factor, which is not usually considered in comparative studies of the costs of dialysis, should be taken into account in future studies on the subject, analysing the relationship between the overall cost of a therapy and the added value generated by it, especially by the public health systems in planning and assigning available resources in a more efficient and effective manner.
Limitations
We have expressed PD and health transport costs in an annual basis, extrapolating the data from one month to 12 months, in order to compare them to HD costs and those mentioned in other studies because of the difficulty in collecting data from an entire year, but we do believe that the calculations presented are representative of the true annual consumption.
We estimated mean costs based on the assignment of health personnel recommended in clinical guidelines instead of those actually used, but we believe that the guidelines recommendations are reasonable.
The mean estimated cost does not represent the true cost for a concrete health area, which will also depend on a given percentage of patients on APD in each area, the percentage of use of special liquids, and the actual assignment of human resources to PD, as well as the true costs of health transport.
In order to calculate the human resources necessary for HD outsourcing agreements, we have assumed that each unit will treat 40 patients in two daily shifts.
We did not consider the health transport costs of patients on PD, which is a real issue on many occasions: training (except for upon hospitalisation, which would imply other costs) and travel for consultations and complementary exams when mobility is limited.
Finally, we also have not evaluated hospitalisation costs, those derived from treatment with erythropoietic agents and other hospital drugs, or those of obtaining peritoneal or vascular access points for dialysis and their complications.
CONCLUSIONS
The repeated affirmation that treatment with PD is cheaper than HD cannot be generalised, since this would depend on several factors in each health area: the proportion of patients on CAPD, APD and special liquids, the cost of HD (in hospitals and outsourced centres), and costs associated with treatment (health transport, hospitalisations, and hospital drugs).
There is an important difference between the cost of outsourced CAPD and the public retail price for the consumables required for this therapy, which should be reconsidered.
The relationship between costs and added value for the health area of dialysis outsourcing agreements should be considered in future studies regarding costs and health services planning.
The discrepancies between the different studies published in Spain regarding the comparative costs of PD and HD needs more rigorous studies that can shed more light on this topic.
CONFLICTS OF INTEREST
The companies Baxter, Fresenius, Gambro and Hospal have collaborated and currently collaborate with our unit in several different continuous training activities.
The Instituto Reina Sofía de Investigación Nefrológica (Reina Sofia Institute of Nephrological Research), which belongs to the Fundación Renal Íñigo Álvarez de Toledo (Íñigo Álvarez de Toledo Kidney Foundation), has collaborated and currently collaborates with our unit in financing several different research projects.
ACKNOWLEDGEMENTS
We would like to thank the members of the departments of inspection in the provincial divisions of the Galicia health department for the four different provinces of Galicia, those responsible for the Galician registry of renal diseases, and the human resources department of the University Hospital Complex of Vigo for their vital collaboration in the search for and acquisition of the data necessary for completing this study.
Table 1. Mean annual cost per patient for PD and HD outsourcing agreements in Galicia with the current rates from the Galicia health department in June 2010 (Official Gazette of Galicia, Iss. 190, dated 01/10/2008)
Table 2. Costs for doctors and nursing staff with 15 years of experience, including the costs of social security
Table 3. Cost of the consumables needed for CAPD with bicarbonate and the costs of the outsourcing agreement
Table 4. Added value for the health area generated by PD and HD outsourcing agreements
Figure 1. Prescription of PD in Galicia and provincial distribution
Figure 2. Use of polyglucose and bicarbonate in Galicia and provincial distribution
Figure 3. Mean cost of health transport by province, in Euros per patient and year, and the impact that this has on the mean annual cost of dialysis outsourcing agreements.
Figure 4. Costs of public HD in current prices (without correcting for inflation) in Euros, from studies published in Spain