Dear Editor,
We read with great interest the prepublished article in your journal by Montañés et al.1 for two reasons. The first, due to its current nature; it has only been a few months since formulas to estimate glomerular filtration rate (eGFR) were published, based on CKD-EPI study (Chronic Kidney Disease Epidemiology Collaboration).2 The second reason is that our group is working, albeit more modestly, along the same lines.
In our project “Knowing Diabetes Numbers” we collected measurements of fasting plasma glucose and HbA1c (FPGHbA 1c) from September 2008 to February 2009 that were performed in the Department of Biochemistry of the Hospital of La Línea de la Concepción, where tests are carried out for the hospital and the six primary care centres (PC).
After excluding the 362 results that came from the outpatient nephrology clinic, 4,820 FPG-HbA1c results were collected (from patients with a mean age of 64 ± 14 years), 55% were made in women and 74% came from PC. Of these, creatinine was also requested in 3,461 (72%), the albumin/creatinine ratio was requested in 1,397 (29%), and a specific request for eGFR was made in only 80 (less than 2%). Subsequently, we calculated the eGFR in the 1,953 requests in which data were available for age, sex, and creatinine using the classical MDRD formula (coefficient 186),3 since the laboratory uses the modified kinetic Jaffé method (Beckman) without traceability to isotope dilution mass spectrometry (IDMS).4,5
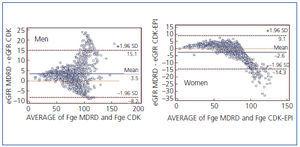
Our results in men were of CKD grade 3 in 13.2% and grades 1-2 in 1.6%. In women, 20% with grade 3 and 3.3% with grades 1-2. These data match the most recently reported data on prevalence of kidney disease in patients with diabetes.6 By applying CKD-EPI, 1.2% of women and 2.5% of men had worsened grading (Table 1). If we apply the Bland-Altman graphic method, the results differ from those of Montañés et al.,1 since there is an average discrepancy of 3.5ml/min (4.4%) favouring MDRD in men and 2.6ml/min (1.7%) favouring CKD-EPI in women (Figure 1). However, our concordance study (intraclass correlation coefficient and Lin coefficient) is greater than 98%.
These differences may be explained by the application of the classical formula (coefficient 186) rather than MDRD-IDMS (coefficient 175) and for the unequal population studied: PC versus the nephrology referral centre, 55% women vs. 30% and 81% with grades 4-5 vs. 63%.
However, on the other hand, the differences are so small that we can say that the new CKD-EPI formulas are tools that are as useful as MDRD and we hope that they will allow us to raise awareness and increase eGFR requests in primary care.
Table 1. CKD grade classification by MDRD
Figure 1. Bland Altman method for concordance between MDRD and CKD-EPI