Introducción: Estudios recientes indican que los beneficios en la supervivencia con hemodiafiltración en línea posdilucional (HDFOL-post) se logran si el volumen de infusión (Vinf) es superior a 20 l por sesión, cifra que no es fácil lograr por los problemas que genera la hemoconcentración. Hoy día contamos con técnicas automáticas que logran un mayor rendimiento minimizando el número de alarmas como el Ultracontrol® (UltraC). Objetivo: El objetivo ha sido, en una primera parte, evaluar el UltraC para conocer qué rendimiento logra (expresado como la fracción de filtración [FF] y el Vinf) y los problemas que presenta y, en una segunda parte, estudiar su funcionamiento con cuatro dializadores diferentes. Material y métodos: Primera parte. Nueve pacientes fueron transferidos a HDFOL-post con UltraC. Se recogieron todas las sesiones correspondientes a los tres primeros meses con HDF-OL y al mes previo en HD. Segunda parte. 18 pacientes en tratamiento crónico con HDFOL-post fueron sometidos a diálisis una semana con cada uno de estos dializadores: FX1000, FX800, Polyflux210 y Elisio 210H. Resultados: Primera parte. En 3 pacientes surgieron problemas asociados a PTM y Psist inadecuadas que se resolvieron pasando a control-presión. Los valores medios obtenidos fueron: Qb máximo 441 (21) (rango 350-490) ml/min, Vinf 26,3 (3,3) l/sesión, FF 30,6% (2,5), KT 59,9 (5) l/sesión, y aumento del KT del 12% respecto al de HD. Segunda parte. Polyflux210 fue el dializador que precisó menos retiradas de UltraC. Las presiones recogidas tanto PTM como Psist fueron distintas y determinaron la necesidad de retirada del sistema. El KT fue adecuado. Conclusiones: a) El sistema UltraC alcanza FF del 30% consiguiendo Vinf adecuados con mínimas alarmas, y b) Dializadores con prestaciones depurativas adecuadas pueden no ser útiles para realizar HDF-OL con UltraC porque sus condiciones flujodinámicas generan alarmas que impiden la aplicación automatizada aunque el rendimento final sea semejante.
Introduction: Recent studies indicate that the survival benefit with post-dilution on line hemodiafiltration (OL-HDF-post) are achieved if the infusion volume (Vinf) is greater than 20L per session, a goal that is not easily achieved due to hemoconcentration problems. Today we have automated techniques to achieve higher performance minimizing the number of alarms as Ultracontrol® (Ultrac). The objective in the first part of study was to evaluate the UltraC performance (expressed as the filtration fraction (FF) and Vinf) and which problems it presents, and in the second part, to study its performance with four different dialyzers. Material and methods: 1st period. Nine patients were transferred to OL-HDF-post with UltraC. The first 3 months on OL-HDF all sessions were recorded and compared with hemodialysis sessions in the previous month. 2nd part: 18 patients on chronic OL-HDF-post were dialyzed for a week with each of these dialyser: FX1000, FX800, Elisio210H and Polyflux210. Results: 1st period: In 3 patients, problems associated with inappropriate pressures emerged. In 3 patients there were problems associated with inadequate PTM and Psist that resolved changing to pressure control. Mean values were: maximum Qb 441 (21) (range 350-490) ml/min, Vinf 26.3 (3.3) l/session, FF 30.6 (2.5)%, KT 59.9 (5) l/session. KT increase of 12% compared to HD. 2nd part: Polyflux210 required less UltraC withdrawals than the others. Different PTM or Psist were found and determined the need for removal of the system. The KT was adequate. a) The UltraC system reaches FF of 30% with minimal alarms and Vinf higher than 20 l. b) Structural characteristics of dialysers can limit their use with UltraC although they managed to desirable KT and Vinf in a manual way.
INTRODUCTION
On-line haemodiafiltration (OL-HDF) is the most complete haemodialysis (HD) technique currently available, since it is capable of eliminating a significant amount of low, medium, and large molecular weight uraemic toxins, with direct relation to the volume of convective transport achieved.1 Traditional HD, in contrast, only eliminates small molecules and a small amount of mid-sized molecules. These cleansing benefits have a monetary cost similar to high-flux HD.
Recent studies have demonstrated significant improvements in the survival of patients that achieve a high number of convective transport litres per OL-HDF session. The results from the DOPPS2 observational study showed that patients on OL-HDF with more than 15l/session had a 35% higher survival rate than those with a lower rate. In 2011, two different randomised studies were presented. In the CONTRAST study,3 patients that achieved more than 20.3l/session had a higher survival rate (hazard ratio [HR]: 0.66), primarily by reducing the rate of cardiovascular mortality (HR: 0.66; P=.03) (HR=0.41). The Turkish HDF Study,4 which demonstrated that the convective transport volume necessary to reduce mortality was situated at a volume of infusion (Vinf) of 17.4l/session (HR: 0.54; P=.02). These results indicate that a Vinf value greater than 20l should be the goal for post-dilutional OL-HDF (post-OL-HDF), in the absence of an established ceiling value above which no greater value is obtained.
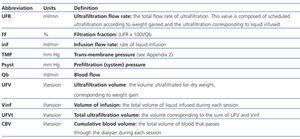
The difficulty in reaching these volumes in post-OL-HDF lies in the technical problems that haemoconcentration causes. In order to avoid this issue, a maximum ratio of 25% between the ultrafiltration flow rate (UFR) and the blood flow (Qb) rate is deemed safe, this ratio being the filtration fraction (FF), see Appendix 1 for an explanation of abbreviations. In this manner, Qb is a limiting factor for achieving the target Vinf, along with the length of the session. For example, if the actual Qb is 250ml/min for a 240min session, Vinf would be 15l, far below the goal of 20l/session. Currently, as a result of optimising Qb and the length of dialysis sessions, we have automated post-dilutional OL-HDF techniques that aid in reaching optimal convective transport values. Despite the importance of these systems, they are poorly represented in the medical literature (for example, the Fresenius® system).5
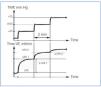
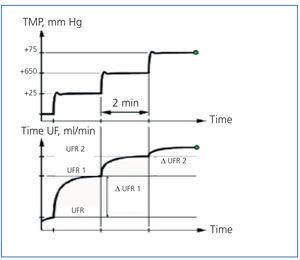
Gambro® has developed an automatic post-OL-HDF system called Ultracontrol® (UltraC). It is based on a pressure-control system that allows for establishing the trans-membrane pressure (TMP), see Appendix 2. In the pressure-control system, TMP is constant and the infusion flow (inF) varies, generally decreasing based on the conditions of the membrane and dialyser as the dialysis session progresses. With UltraC, biosensors detect changes induced in the UFR when TMP increases (Figure 1). If the increase in UFR is significant, the change is maintained; if the increase in TMP does not favour an increase in UFR, then that pressure is the one established. In a traditional volume control system, UFR is fixed, and when this level is high, the pressure will increase, generating alarms and other problems throughout the dialysis session. As such, the fundamental advantage to an automated treatment of this type is that the post-OL-HDF produces better results without generating TMP alarms or coagulations in the dialyser.
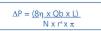
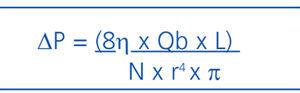
In post-OL-HDF, not only must the rheological characteristics of the patient’s blood be taken into account, but also the hydraulic condition of the dialyser. These characteristics are determined by the membrane as well as the capillary and dialyser design, since these are the factors that determine the pressures maintained throughout the dialyser. As observed in the Hagen-Poiseuille formula (Appendix 3), the internal radius of the capillary (raised to the fourth power) is a determining factor, since small changes in diameter produce large changes in pressure.6 As such, the design of the dialyser is fundamental for a technique such as the UltraC to work properly, with the goal of optimising effectiveness, avoiding alarms, and facilitating the work of the nursing staff.
With this perspective, the objective of our study was to evaluate the UltraC as a post-OL-HDS technique. Firstly, we sought to assess the output of this unit, expressed as FF and Vinf, testing whether FF exceeded the value of 25% from the traditional system and if Vinf was higher than 20l. Secondly, we analysed how the UltraC adapts to four different dialysers.
MATERIAL AND METHOD
We performed a prospective, observational study in two parts. In both, all patients received treatment three days per week with a mean duration of 240 minutes per session (range: 225-300 minutes)
The abbreviations used and their definitions are summarised in Appendix 1.
Part one. Evaluation of FF and Vinf achieved using UltraC
We examined 9 patients (7 men and 2 women, mean age of 60 [13] years, mean weight of 76 [9] kg) that had been undergoing high-flux HD treatment for more than 3 months, and that were transferred to post-OL-HDF due to medical indications. We compiled all high-flux HD sessions corresponding to the previous month and the first three months on OL-HDF. All patients had an arteriovenous fistula as a vascular access point.
All patients were dialysed on machines using UltraC, AK200US®. We used the same high-flux dialyser as when patients were on HD (Polyflux210H®), as well as the same Qb, Qd, duration of sessions, and all other dialysis characteristics. The value used for Qb was the maximum value allowed by the vascular access, without allowing pressure in the arterial line to drop below 220mm Hg.
During each session, the following variables were collected: Qb ml/min, CBV (l/session), UFV (l/session), maximum inF (ml/min), Vinf (l/session), UFVt (l/session), KT (l/session, ionic dialysance), TMP (mm HG), Psyst (mm Hg), and all complications derived from the technique used and coagulation that occurred during the first three months of treatment.
We evaluated whether FF was superior to the rate of 25% reached in the traditional volume-control technique, and if Vinf was greater than 20l.
Part two. Usefulness of UltraC using different dialysers
We evaluated 18 patients (17 men and 1 woman, mean age of 66 [75] years) that had been undergoing chronic post-OL-HDS treatment for more than 3 months on AK200US® machines. Vascular access was achieved using a tunnelled catheter in three.
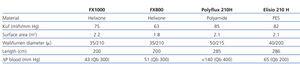
All patients underwent dialysis for one week using each of the different dialysers mentioned in Table 1, while maintaining all other dialysis parameters constant.
In each session, the following variables were measured: Psyst, TMP, Vinf, KT, the number of times the UltraC had to be withdrawn, filter coagulations, and haemoglobin and protein levels from the first week.
In both parts of the study, we calculated FF.
In all cases, the nursing staff connected the UltraC system at the start of the post-OL-HDF session, fixing the alarm systems for TMP>300 or Psyst>700mm Hg. When an alarm was triggered and the problem was not resolved, UltraC was withdrawn and the patient was transferred to a pressure-control system, which maintained the TMP at a fixed level at values that ensured a Psyst<700mm Hg and an appropriate inF.
Statistical analysis
All data were registered in a database for statistical analysis using SPSS software, version 15.0. We presented data as means and standard deviations (SD). We compared groups using paired sample analyses (paired t-test and Friedman).
RESULTS
Part one. Evaluation of FF and Vinf achieved using UltraC
In six patients, UltraC worked without incidents, and technical problems arose in three patients, two of which were associated with Psyst greater than 700mm Hg, and one of which was due to a TMP greater than 300mm Hg. These three patients were transferred to pressure-control systems. After this adjustment, the number of incidents per session in all nine patients was <5%.
The results obtained in all nine patients during the first and third months are compiled in Table 2.
The mean values obtained during these three months were: maximum Qb: 441 (21) ml/min (range: 350-490), CBV: 96.2 (7.7) l/session, UFV: 3.2 (0.8) l/session, Vinf: 26.3 (3.3) l/session, UFVt: 29.5 (3.4) l/session, FF: 30.6 (2.5) %, maximum TMP: 190.8mm Hg (range: 125-301), maximum Psyst: 496.5 (94.6) mm Hg. KT was 12% higher than in high-flux HD (53.8 [5.1] l/session vs 59.9 [5] l/session).
Part two. Usefulness of UltraC using different dialysers
The mean values and ranges of Hb and proteins were, respectively, 12.1 (10.5-13.7) and 6.4 (5.9-7.3) g/dl. Maximum Psyst and TMP values appear in Table 3. Results were significantly different from those using the Elisio dialyser.
The UltraC had to be withdrawn in all sessions in nine, eight, four, and two patients when using the Elisio, FX 1000, FX800 and Polyflux dialysers, respectively. The dialyser that required the fewest transfers from UltraC to pressure-control systems was the Polyflux machine, followed by FX and Elisio. The mean number of sessions in which UltraC had to be withdrawn appears in Table 4.
Despite the switch to pressure-control, the use of all dialysers produced adequate values of Vinf and KT (Table 3), with no differences in the number of coagulations of the system. The highest values were achieved using the FX1000 dialyser, and the lowest values using the FX800.
DISCUSSION
Our study shows how the UltraC automated system can achieve infusion volumes of 26l and FF far greater than 25% in four hours of dialysis, with only a small number of alarms, which facilitates the application of this technique and ensures good quality of the dialysis provided. If we add to these values the UF used to maintain dry weight, the convective transport volumes reach 30l per session. With this volume, patients clearly surpass the 20l value which, according to previously cited studies, implies benefits to survival using these convective techniques.
UltraC periodically measures TMP and adjusts UFR, which provides an “individualised” treatment in which the dialysis machine adapts to each patient and the changes that are produced throughout the session. This adjustment produces a maximum Vinf that is superior to the value reached using traditional OL-HDF, in which a blood flow percentage is predetermined (with UltraC, we can reach an FF of almost 30% Qb).
The information provided by measuring Psyst is essential. The use of Psyst would cause TMP to be overestimated and would result in a reduced margin of error for this technique. Its use as an external source of information provides clues as to the changes within the dialyser throughout the session that might lead to coagulation, and allows us to anticipate events that would not be detectable with TMP alone. The measurement of Psyst favours earlier response by the nursing staff to avoid continuous alarms, coagulation of the system, and to achieve proper Vinf.
Only one study by Teatini et al describes the efficacy of using the UltraC system and its practical use.7 This study clearly shows the advantages of using a system such as UltraC, although the Vinf values reached are lower than we achieve in daily clinical practice, since they worked with Qb values lower than 300ml/min. In this publication, the role of Psyst in the functioning of this system is not well elaborated, with results for only one dialyser, which is an unusual situation in the daily practice of dialysis units, where various dialysers are commonly used. The results from this study, with the Vinf values reached, made us reflect on the need to take into account all the elements that we can modify to reach Vinf values greater than 20l. Although we may be using a very good technique, it might not be profitable if it does not reach the Qb values necessary for a high UFR.8
There is also very little in the medical literature dedicated to other automated systems such as the Fresenius® system, which facilitates an automatic inF prescription if total protein and haematocrit values are specified. With this application, we can also achieve a greater inF, with increased convective transport while maintaining the same risk of alarms, which lends greater support to these automated systems.5
The second part of our study shows that although we obtained adequate KT and Vinf values in all dialysers, the number of alarms was slightly different between systems. These alarms required the transfer from UltraC to pressure-control systems, which increases the work load needed and underlines the importance of choosing the best dialyser for the technique used. The Polyflux dialyser, which is also designed by Gambro, was the design that produced the fewest number of alarms and was best adapted to the technique, as expected. In contrast, the Elisio dialyser design, with a tighter and longer fibre diameter that is optimal for a high-flux HD unit and pressure-control systems, is not well-suited for use with UltraC. As mentioned previously, the AK-200US provides an additional piece of information in the form of Psyst, and the Elisio dialyser resulted in extremely high Psyst values even in the first hour of the dialysis session, requiring a switch to pressure-control dialysis even though TMP values were not high. These Psyst alarms were a consequence of the design of the dialyser, since the Hagen-Poiseuille equation states that a smaller fibre radius induces higher pressure. In contrast, in other dialysers such as the Polyflux, Psyst continued to increase throughout the session, which indicated changing conditions within the filter and anticipated the possible partial or total coagulation of the filter. In this manner, Psyst offers information in addition to TMP, which aids in preventing complications. In other machines, such as the 5008, Psyst is integrated into the value of TMP, although this information is not provided to the user.
In any case, although the number of alarms was high with UltraC, forcing a switch to pressure-control systems, the efficacy of the technique was good, since we obtained adequate Vinf and KT values using all dialysers. The differences shown in these parameters in favour of the FX1000 dialyser are attributable to the fact that this dialyser has a larger surface area than the others, and the opposite is true in the smaller FX800. Clearly, the type of dialyser used is a determining factor in these techniques. Small changes in fibre diameter will influence the number of alarms produced, and small changes in surface area will produce changes in KT and Vinf that, although may seem irrelevant, involve an increase in the weekly dialysis dosage administered and, probably, will have long-term effects on survival. These findings make us reflect on the need for maximum payoff from the devices used in daily practice, which can be achieved by understanding the technical specifications and optimal use of each, since the characteristics of these systems are not solely determined by their composition.9 In this manner, although all of the dialysers used in our study were effective from a practical point of view, the dialyser best suited for use with the UltraC system is the Polyflux, and a pressure-control system should be used in the case of other types of dialysers in order to reduce the number of alarms produced.
One last technical aspect of OL-HDF that we would like to comment on is the loss of albumin. This loss depends on the type of dialyser,10,11 but some authors also relate this phenomenon to the application of a high TMP during the first 30 minutes of OL-HDF.12 The UltraC system normally starts with a TMP that increases progressively during the first 30 minutes, in an attempt to avoid this complication.
In addition to the technical objectives of this study, making post-OL-HDF easily applicable is a fundamental step in facilitating its widespread use. As such, the number of alarms produced must be minimised in order to facilitate the work of the nursing staff. From this point of view, UltraC fulfils expectations, since the system is easily transferable to pressure-control when alarms appear, and indicates the proper TMP that needs to be set in order to achieve a proper Vinf.
In conclusion, UltraC is the optimal system for achieving Vinf levels greater than 20l. Dialysers with adequate purifying capabilities may not be useful for use in OL-HDF with UltraC because their flow and dynamic characteristics generate high Psyst values that impede automated use, although the final outcome may be similar. An adaptation of existing dialysers to this technique would aid nursing staff, facilitating an improved and more widespread use of OL-HDF.
Conflicts of interest
Dr. M. Albalate has participated as a speaker in meetings organised by Gambro® y Fresenius®.
Dr. R. Pérez García and Dr. P. de Sequera have participated as speakers in meetings organised by Gambro®, Fresenius® and Bellco®, and work as advisors for FMC.
Acknowledgements
We would like to thank the nursing staff at the Haemodialysis Unit of the Infanta Leonor Hospital.
Table 1. Technical specifications for the dialysers
Table 2. Results from the use of OL-HDF with UltraC for three months
Table 3. Results from the use of UltraC with different dialysers
Table 4. UltraC withdrowal according to the type of dialyser used
Figure 1. Schematic of the functioning of UltraC
Abbreviations and definitions
Functioning of the UltraC system
Hagen-Poiseuille equation