The recent conceptualization of the cardiovascular-kidney-metabolic (CKM) syndrome by the American Heart Association (AHA) opens an opportunity for a multidisciplinary and lifelong approach in the risk stratification, early prevention, and treatment of the vicious circle generated by the interaction of cardiovascular, renal and metabolic risk factors and aggravated by the development of cardiovascular diseases (including their full spectrum: heart failure, atrial fibrillation, coronary heart disease, stroke, and peripheral arterial disease), chronic kidney disease or type 2 diabetes mellitus, with the excess or dysfunctional adiposity as the trigger. Three publications offer the rational basis of a conceptual decalogue and action plan and a new cardiovascular risk stratification equation since the age of 30 that includes measures of renal function/damage, among others, to promote effective cardiovascular, renal, and metabolic prevention. In Spain, we must leverage this momentum to adapt these new concepts to our reality with greater and improved collaboration between primary care and the specialties involved in CKM syndrome, including the formation of multidisciplinary units for the optimal management using a patient-centred approach.
La reciente conceptualización del síndrome cardiovascular-reno-metabólico (CRM) por la American Heart Association (AHA) abre una oportunidad al abordaje multidisciplinar y desde etapas tempranas de la vida en la estratificación del riesgo, la prevención y el tratamiento precoz del círculo vicioso generado por la interacción de factores de riesgo cardiovasculares, renales y metabólicos y agravado por el desarrollo de enfermedades cardiovasculares (incluyendo todo su espectro: insuficiencia cardíaca, fibrilación auricular, enfermedad coronaria, accidente cerebrovascular, y enfermedad arterial periférica), enfermedad renal crónica o diabetes mellitus tipo 2, con la adiposidad excesiva o disfuncional como sustrato del problema. Un trío de publicaciones ofrecen las bases racionales de un decálogo conceptual y de acción, con nuevas herramientas de estratificación de riesgo cardiovascular desde los 30 años de edad y que incluyen medidas de función/daño renal, entre otras, que permitan una eficaz prevención cardiovascular, renal y metabólica. En España debemos aprovechar este impulso para adaptar los nuevos conceptos a nuestra realidad con una mayor y mejor colaboración entre atención primaria y las diversas especialidades implicadas, incluyendo la creación de unidades multidisciplinares para un manejo óptimo y centrado en el paciente.
Chronic kidney disease (CKD) is highly prevalent all around the world, with a high burden for patients and healthcare systems and high morbidity and mortality,1 especially from cardiovascular (CV) causes.2 In Spain, its prevalence is as high as 15% of the population, and it is even higher in subjects with cardiovascular disease (CVD) or with the accumulation of CV risk factors, including obesity, diabetes mellitus and components of metabolic syndrome.3
CVD often occurs concomitantly with metabolic disease, including type 2 diabetes mellitus and obesity, and with CKD.3 Cardiorenal syndrome - the close bidirectional relationship between the heart and kidneys4,5 - and cardiometabolic syndrome, in which excess adiposity is associated with systemic inflammation, insulin resistance, as well as components of metabolic syndrome, which are associated with an increased CV risk,6,7 are widely recognised. More recently, it has been described the association between metabolic syndrome and CKD8 and there is a growing awareness that metabolic disorders, particularly those associated with excess adiposity (above all, visceral adiposity and ectopic fat in other organs), play a key pathophysiological role in heart-kidney interactions.9 In this sense, CKD is a key mediator of the relationship between metabolic risk factors and CVD, especially heart failure (HF).10 This is intensified by an increasing prevalence, as well as a frequent overlap between CVD, kidney disease and metabolic disorders,11,12 which are associated with an increase in morbidity and mortality, especially from CV causes, and the risk increases in proportion to increasing multimorbidity.13 For all these reasons, considering cardiometabolic syndrome and cardiorenal syndrome as separate entities does not seem appropriate, and there is growing recognition of the overlap between the two and the need to create a broader construct.
In this context, a recent presidential statement from the American Heart Association (AHA) published in Circulation defines the adverse interaction between these conditions as cardiovascular-kidney-metabolic syndrome (CKM).14 Having more than one of these conditions multiplies morbidity and mortality, particularly from CV causes.15 This advisory defines CKM syndrome as a spectrum of diseases associated with excessive or dysfunctional adiposity and proposes its staging, with the intention of predicting its risk of CV events, preventing and even reversing it, and addressing it throughout life, from childhood to adulthood. The scientific evidence supporting this declaration is published in a separate article.16 More recently it has been published, a CV risk calculator that includes, among other items, measures of renal function (estimated glomerular filtration rate [eGFR]) and kidney injury (urine albumin/creatinine ratio [uACR]).17 Together, these publications provide a framework for holistically and equitably improving CKM health in the general population, from childhood and youth through adulthood, with a particular emphasis on prevention.
The declaration details its top 10 highlights that includes the following notable aspects:
Definition of cardiovascular-kidney-metabolic syndromeCKM syndrome is defined as a systemic disorder characterised by pathophysiological interactions between metabolic risk factors, CKD and the CV system that lead to multi-organ failure and an increased risk of CV events. CKM syndrome includes both individuals at risk for CVD, owing to the presence of metabolic risk factors, CKD, or both, and individuals with existing CVD that is potentially related to or complicates metabolic risk factors or CKD. The risk of developing CKM syndrome and its adverse outcomes is further influenced by unfavorable lifestyle conditions and lack of self-care, which are facilitated by certain health policies, the economic situation and environmental factors.14
It is therefore a progressive, multi-organ syndrome that includes a broad spectrum, both those at risk of CVD and kidney disease, as well as those with CVD and/or established kidney disease, and which considers the negative feedback connections between obesity-diabetes, CKD and CVD in its broad sense (heart failure, coronary heart disease, cerebrovascular accident, atrial fibrillation and peripheral arterial disease) and which lead to poor health outcomes,14,18 including a poorer patient quality of life.19,20
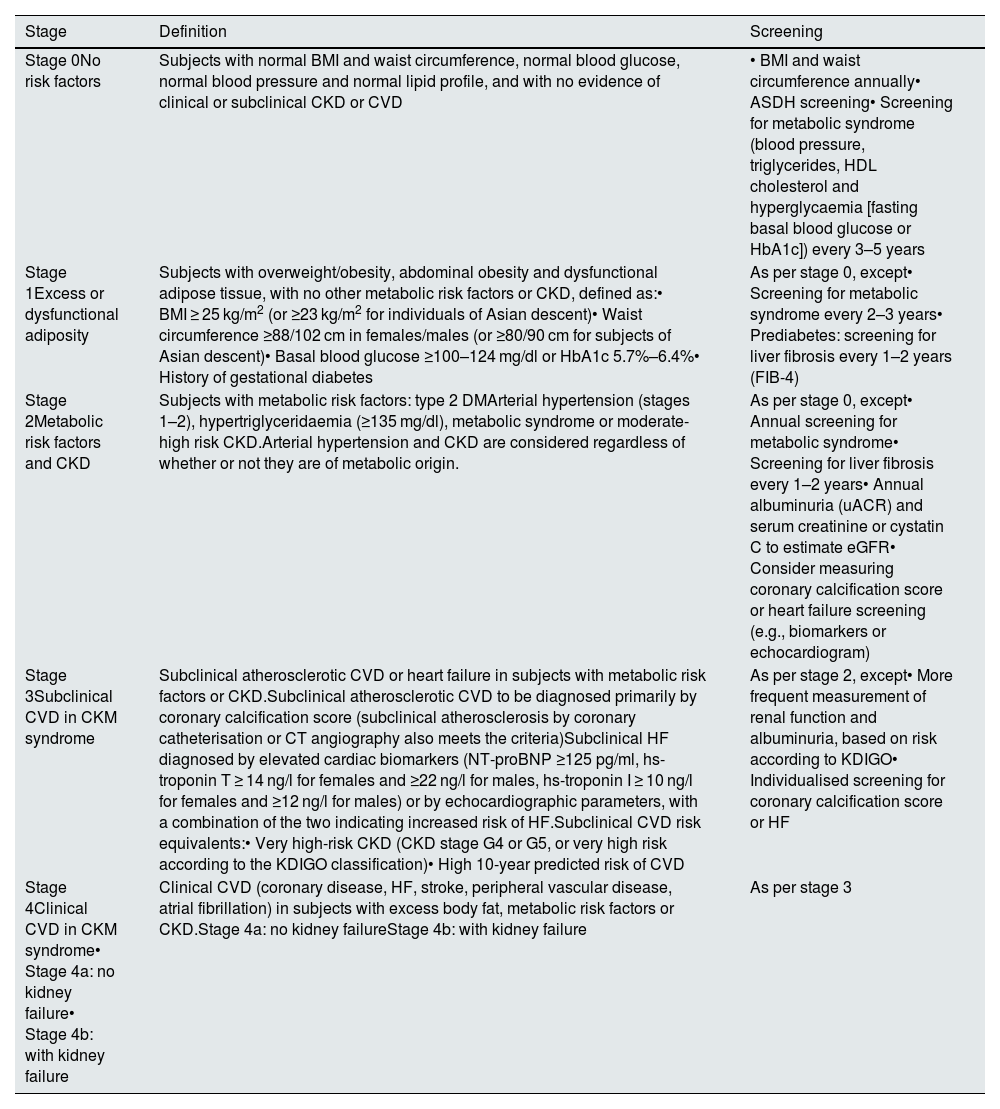
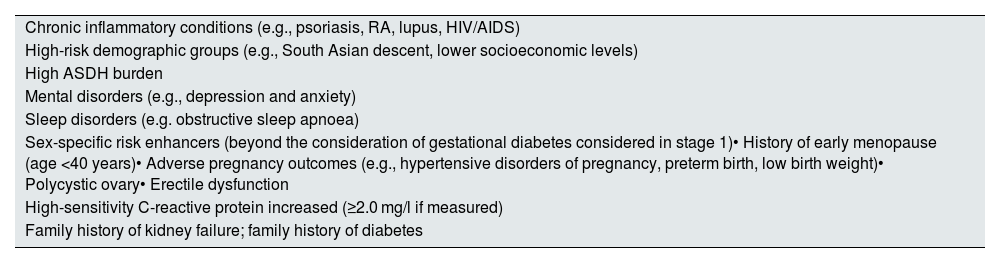
Staging of CKM syndromeThe advisory declaration also proposes classifying CKM syndrome into four stages, reflecting the pathophysiology, risk spectrum and opportunities for prevention and optimal treatment across the continuum of CKM syndrome (Table 1). Factors that increase the risk and influence the probability of progression throughout the stages of CKM syndrome are also considered (Table 2).
Stages of CKM syndrome: definitions and screening proposals.
| Stage | Definition | Screening |
|---|---|---|
| Stage 0No risk factors | Subjects with normal BMI and waist circumference, normal blood glucose, normal blood pressure and normal lipid profile, and with no evidence of clinical or subclinical CKD or CVD | • BMI and waist circumference annually• ASDH screening• Screening for metabolic syndrome (blood pressure, triglycerides, HDL cholesterol and hyperglycaemia [fasting basal blood glucose or HbA1c]) every 3–5 years |
| Stage 1Excess or dysfunctional adiposity | Subjects with overweight/obesity, abdominal obesity and dysfunctional adipose tissue, with no other metabolic risk factors or CKD, defined as:• BMI ≥ 25 kg/m2 (or ≥23 kg/m2 for individuals of Asian descent)• Waist circumference ≥88/102 cm in females/males (or ≥80/90 cm for subjects of Asian descent)• Basal blood glucose ≥100–124 mg/dl or HbA1c 5.7%–6.4%• History of gestational diabetes | As per stage 0, except• Screening for metabolic syndrome every 2–3 years• Prediabetes: screening for liver fibrosis every 1–2 years (FIB-4) |
| Stage 2Metabolic risk factors and CKD | Subjects with metabolic risk factors: type 2 DMArterial hypertension (stages 1–2), hypertriglyceridaemia (≥135 mg/dl), metabolic syndrome or moderate-high risk CKD.Arterial hypertension and CKD are considered regardless of whether or not they are of metabolic origin. | As per stage 0, except• Annual screening for metabolic syndrome• Screening for liver fibrosis every 1–2 years• Annual albuminuria (uACR) and serum creatinine or cystatin C to estimate eGFR• Consider measuring coronary calcification score or heart failure screening (e.g., biomarkers or echocardiogram) |
| Stage 3Subclinical CVD in CKM syndrome | Subclinical atherosclerotic CVD or heart failure in subjects with metabolic risk factors or CKD.Subclinical atherosclerotic CVD to be diagnosed primarily by coronary calcification score (subclinical atherosclerosis by coronary catheterisation or CT angiography also meets the criteria)Subclinical HF diagnosed by elevated cardiac biomarkers (NT-proBNP ≥125 pg/ml, hs-troponin T ≥ 14 ng/l for females and ≥22 ng/l for males, hs-troponin I ≥ 10 ng/l for females and ≥12 ng/l for males) or by echocardiographic parameters, with a combination of the two indicating increased risk of HF.Subclinical CVD risk equivalents:• Very high-risk CKD (CKD stage G4 or G5, or very high risk according to the KDIGO classification)• High 10-year predicted risk of CVD | As per stage 2, except• More frequent measurement of renal function and albuminuria, based on risk according to KDIGO• Individualised screening for coronary calcification score or HF |
| Stage 4Clinical CVD in CKM syndrome• Stage 4a: no kidney failure• Stage 4b: with kidney failure | Clinical CVD (coronary disease, HF, stroke, peripheral vascular disease, atrial fibrillation) in subjects with excess body fat, metabolic risk factors or CKD.Stage 4a: no kidney failureStage 4b: with kidney failure | As per stage 3 |
ASDH: adverse social determinants of health; BMI: body mass index; CKD: chronic kidney disease; CVD: cardiovascular disease; DM: diabetes mellitus; HbA1c: glycosylated haemoglobin; HF: heart failure; uACR: urine albumin-creatinine ratio.
Risk factors in CKM syndrome.14
| Chronic inflammatory conditions (e.g., psoriasis, RA, lupus, HIV/AIDS) |
| High-risk demographic groups (e.g., South Asian descent, lower socioeconomic levels) |
| High ASDH burden |
| Mental disorders (e.g., depression and anxiety) |
| Sleep disorders (e.g. obstructive sleep apnoea) |
| Sex-specific risk enhancers (beyond the consideration of gestational diabetes considered in stage 1)• History of early menopause (age <40 years)• Adverse pregnancy outcomes (e.g., hypertensive disorders of pregnancy, preterm birth, low birth weight)• Polycystic ovary• Erectile dysfunction |
| High-sensitivity C-reactive protein increased (≥2.0 mg/l if measured) |
| Family history of kidney failure; family history of diabetes |
These factors increase the likelihood of progression through the stages of CKM syndrome with the associated risks of cardiovascular disease and kidney failure.
ASDH: adverse social determinants of health; CKM: cardiovascular-kidney-metabolic; HIV/AIDS: human immunodeficiency virus/acquired immunodeficiency syndrome; RA: rheumatoid arthritis.
Stage 0. No CKM syndrome risk factors. With the primary goal of prevention (preventing the development of CKM syndrome factors) by achieving and maintaining good cardiovascular health from the early stages of life.
Stage 1. Excess adiposity (overweight or increased waist circumference) or dysfunctional adiposity (clinically manifested as glucose intolerance or prediabetes) in the absence of other CKM risk factors. Excess visceral adiposity, frequently associated with ectopic fat deposition in certain tissues (liver, heart, skeletal muscle, pancreas or kidneys associated with the development of insulin resistance, systemic inflammation and oxidative stress that contribute to the development of metabolic risk factors and CKD. This stage includes women with gestational diabetes who are at significant risk of future diabetes. The objective is the identification and treatment of excess/dysfunctional adiposity for the prevention of CKM and CKD risk factors.
Stage 2. Metabolic risk factors, specifically hypertriglyceridaemia (≥135 mg/dl), hypertension (stages 1 and 2), diabetes or metabolic syndrome; or moderate- to high-risk CKD according to the stratification of the 2012 KDIGO guideline on CKD,21 equivalent to mild-moderate CKD from the European Society of Cardiology (ESC) 2021 guidelines.22,23 It includes arterial hypertension due to causes other than obesity/metabolic syndrome and CKD due to causes other than diabetes or hypertension. The role of lifestyle changes and treatment of modifiable risk factors is emphasised here.
Stage 3. Subclinical CVD (usually detected by imaging procedures or subclinical HF detected by biomarkers or echocardiogram abnormalities) in subjects with CKM syndrome or risk equivalents; specifically high risk of CVD according to the CKM syndrome risk algorithm or very high-risk CKD (according to the KDIGO guidelines), equivalent to severe CKD according to the 2021 ESC guidelines, including, but not limited to, CKD stages G4 and G5.22,23 With the aim of delaying or stopping the progression to clinical disease with preventive measures.
Stage 4. Clinical CVD, including the entire spectrum of CVD (coronary heart disease, cerebrovascular disease, peripheral vascular disease, arrhythmias [atrial fibrillation] and HF) in subjects with CKM syndrome. In turn, they are subclassified into:
- none-
Stage 4a: no kidney failure.
- none-
Stage 4b: with kidney failure.
Differentiation based on the specificities of management, especially of HF, ischaemic heart disease and atrial fibrillation in the latter population.
The goal here is to treat CV complications in the context of CKM syndrome to reduce morbidity and mortality.
CKM risk factor screening and cardiovascular risk assessmentThe advisory review suggests that CKM risk factor screening should be conducted throughout life, starting as early as childhood, and suggests that its frequency and intensity should increase as the stages of CKM syndrome progress, in order to improve prevention and treatment strategies, both in young subjects and in adults. For example, pediatricians can detect and classify the risks of CKM syndrome from birth, and can even include prenatal factors (maternal obesity or hypertension). Early identification of overweight/obesity, or markers of metabolic syndrome (arterial hypertension, dyslipidaemia and hyperglycaemia) in the population are also advised. The objective of this early staging is to be able to promote modifications in social, behavior, and biological risk factors for CKM syndrome from childhood onwards, since excessive adiposity from early age has been associated with a higher risk of CKM syndrome, CKD and CVD.24–26
Early years of life- •
Annual screening of overweight/obesity.
- •
Blood pressure monitoring starting at three years of age, annually without risk factors, or at each visit if there are risk factors, such as overweight/obesity, diabetes, CKD or structural heart disease.
- •
Mental and behavioural health. Screening for adverse social determinants of health (ASDH) in every child, as they have been associated with worse CKM outcomes.27,28
- •
Fasting lipid profile between nine and 11 years of age, and then between 17–21 years.
- none-
At two years, if there is a family history of early CVD or familial hypercholesterolaemia.
- none-
- •
Additionally, basal blood glucose/oral glucose tolerance test/HbA1c, or AST starting at 9–11 years in children with overweight/obesity, at risk of developing type 2 diabetes mellitus or fatty liver.
- none-
If normal, repeat every two-three years in children with obesity or overweight in the presence of another additional risk factor.
- none-
At this point, it should be noted that this is a North American proposal aligned with the American Academy of Pediatrics, and that recommending universal screening in children does not seem to be included in the paediatric guidelines in Europe/Spain, except in children with CV risk factors and/or family history of monogenic lipid disorders, since it cannot be extrapolated the presence of obesity/diabetes and/or CVD in the United States and Spain.
From 21 years of age- •
Screening for adverse social determinants of health.
- •
BMI and waist circumference annually.
- •
Screening for components of metabolic syndrome (arterial hypertension, hypertriglyceridaemia, low HDL cholesterol and hyperglycaemia).
- none-
Annually in stage 2 CKM syndrome.
- none-
Every two-three years in stage 1 or history of gestational diabetes.
- none-
Every three-five years in subjects with stage 0 CKM syndrome.
- none-
- •
Screening for advanced fibrosis related to fatty liver every one-two years if diabetes, prediabetes or ε two metabolic risk factors using the FIB-4 index.
- •
Urine albumin creatinine ratio (uACR), as well as serum creatinine/cystatin C for KDIGO CKD staging.
- none-
Annually in CKM syndrome stage 2 or higher.
- none-
More frequently the higher the risk according to KDIGO.
- none-
- •
Coronary artery calcification score (CACS) is a reasonable measurement in subjects with intermediate 10-year CV risk in order to guide intensification of preventive measures.
- •
Screening for subclinical HF (echocardiogram and/or cardiac biomarkers) probably based on the risk score according to age, comorbidities and CV risk (not yet defined), as proposed by the ADA or the Cardiology guidelines, given the higher risk of its development in subjects with CKM syndrome.29,30
Starting at the age of 30, it is proposed to begin estimating the risk of CVD and, if necessary, to start cardioprotective therapies in accordance with the guidelines with a view to returning the CKM syndrome stage. This is especially important as early detection and management can maximise the benefit of cardiorenal protection, especially among the younger population.31,32
Special emphasis is placed on the periodic measurement of kidney function and damage in subjects with stage 2 or higher CKM syndrome (subjects with CKD, diabetes, hypertension or metabolic syndrome). This applies both to the eGFR, and particularly to the measurement of albuminuria, through the uACR in the population at risk, to improve the estimation of the risk of CKD and CVD (especially heart failure), which is consistent with the recent KDIGO initiatives for early identification and management of CKD.33 In this regard, the cost-effectiveness of kidney function/injury measures has recently been demonstrated, based on the additional cardiorenal benefit of new sodium-glucose cotransporter type 2 (SGLT-2) inhibitors.34 It should be noted that the 2021 ESC guidelines already incorporated the determination of kidney function and albuminuria at the same level of relevance as lipids, blood glucose and blood pressure in the stratification of CV risk.22
The presidential advisory also proposes considering measuring CACS and cardiac biomarkers, and performing echocardiogram in these high-risk subjects, as discussed previously.14
Prevention and treatment in CKM syndrome: importance of the original causeAccording to the presidential advisory, excess or dysfunctional adiposity is the underlying cause of the organic lesions associated with CKM syndrome14 and should therefore be addressed through lifestyle changes and weight loss to prevent progression and facilitate regression through the stages of CKM syndrome. Obesity is associated not only with metabolic syndrome, but also with increased morbidity and mortality, even in subjects without metabolic syndrome.35,36 In contrast, weight loss is associated with improved CV and renal prognosis in obese or overweight subjects.37–39 In fact, the advisory also mentions other obesity-related complications, such as hepatic steatosis, sleep apnoea or even the risk of cancer.14
Ectopic fat can be a local source of mediators that can cause damage in the affected organs through compression. This can occur in the heart (fat deposits in the pericardium and epicardium, particularly when deposited in the epicardium), promoting the onset of arrhythmias, myocardial dysfunction and coronary atherosclerosis,40 as well as at the intra- and perirenal level, which contributes to hypertension.41
The development of metabolic dysfunction-associated steatotic liver disease (MASLD; previously called non-alcoholic fatty liver disease) further amplifies systemic inflammation and insulin resistance. The release of pro-oxidant and pro-inflammatory mediators into the systemic circulation exacerbates the pathological processes involved in atherosclerosis and myocardial injury.40 In the kidney, it exacerbates glomerulosclerosis, tubular inflammation and renal fibrosis.42
MASLD and CKD constitute two global public health problems, since the former affects almost 30% of the general adult population.43 Both are chronic diseases and are expected to increase dramatically in the foreseeable future and are closely associated with poor outcomes, premature mortality, decreased quality of life and high social costs.39,43,44 A recent meta-analysis of 13 observational cohort studies (including over 1.2 million individuals) demonstrated that MASLD was significantly associated with an up to 1.5-fold increased risk of incident CKD over a mean follow-up time of 10 years.45
The AHA advisory’s position on obesity is not new and is consistent with previous proposals by endocrinologists advocating abandoning the glucocentric approach and primarily addressing obesity in the management of subjects with type 2 diabetes,46 and with the relevance that the new type 2 diabetes guidelines attach to obesity management,47 which supports the value of the advisory.
Education and support in the implementation of healthy lifestyles can help improve CKM health in both individuals and the population. In this sense, the adoption of the AHA Life’s essential 8 on preventive measures is proposed,48 which includes diet, physical activity, nicotine exposure, sleep hygiene, body mass index, lipids, blood glucose and blood pressure. In Spain, the Mediterranean diet is associated with improvement of metabolic syndrome, CV and renal risk,49–51 and physical exercise reduces visceral fat in obese or overweight individuals.52
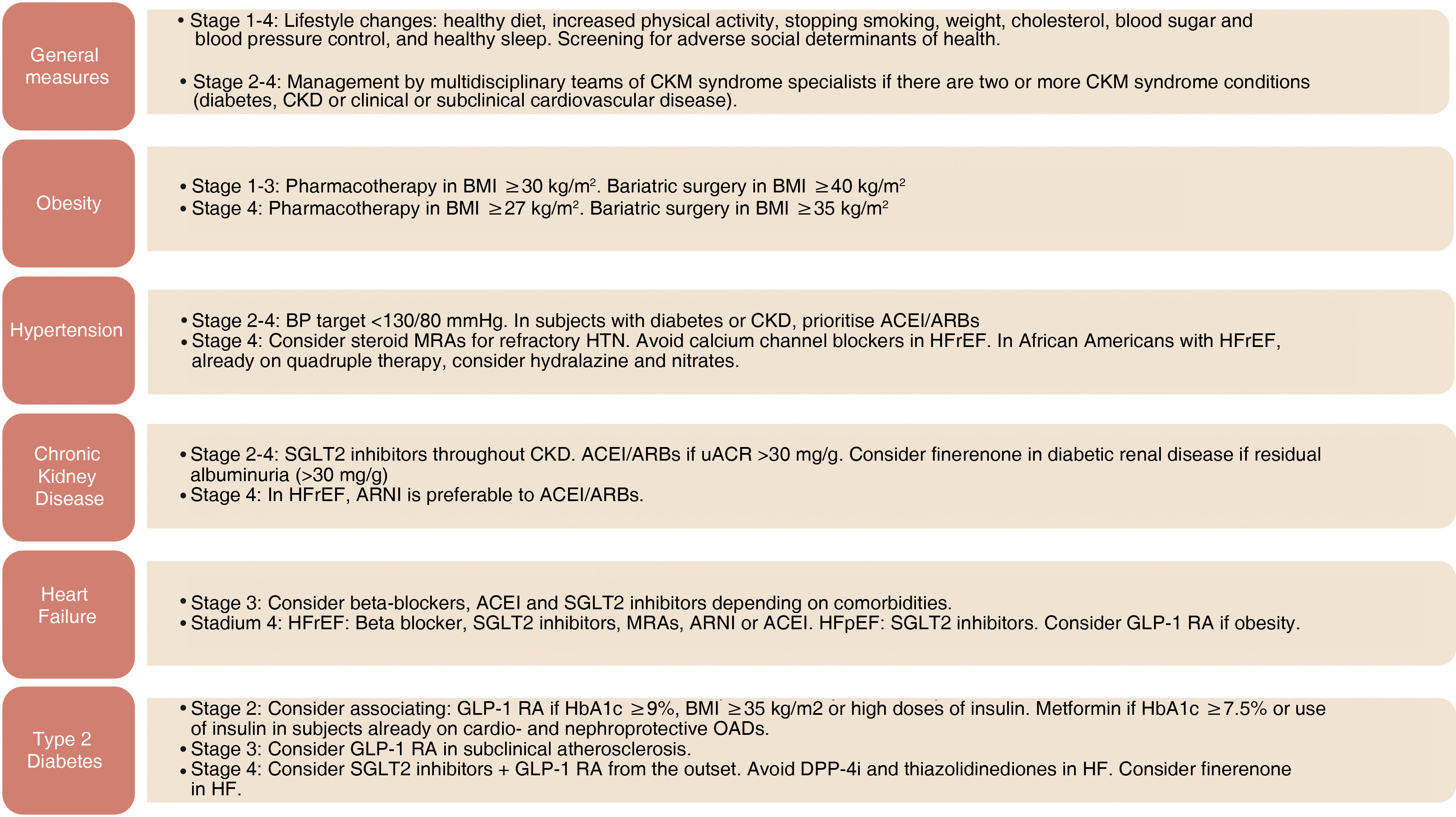
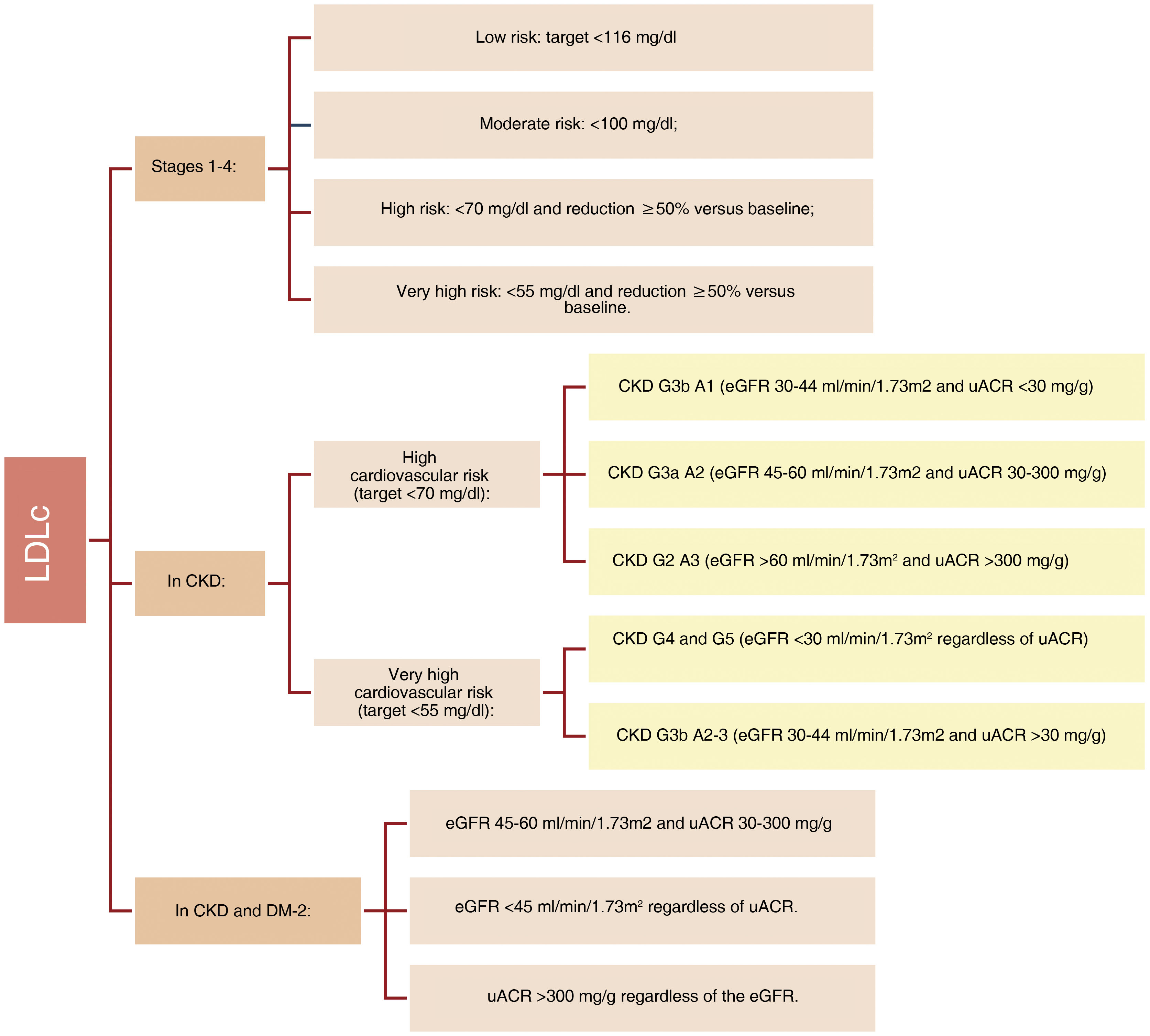
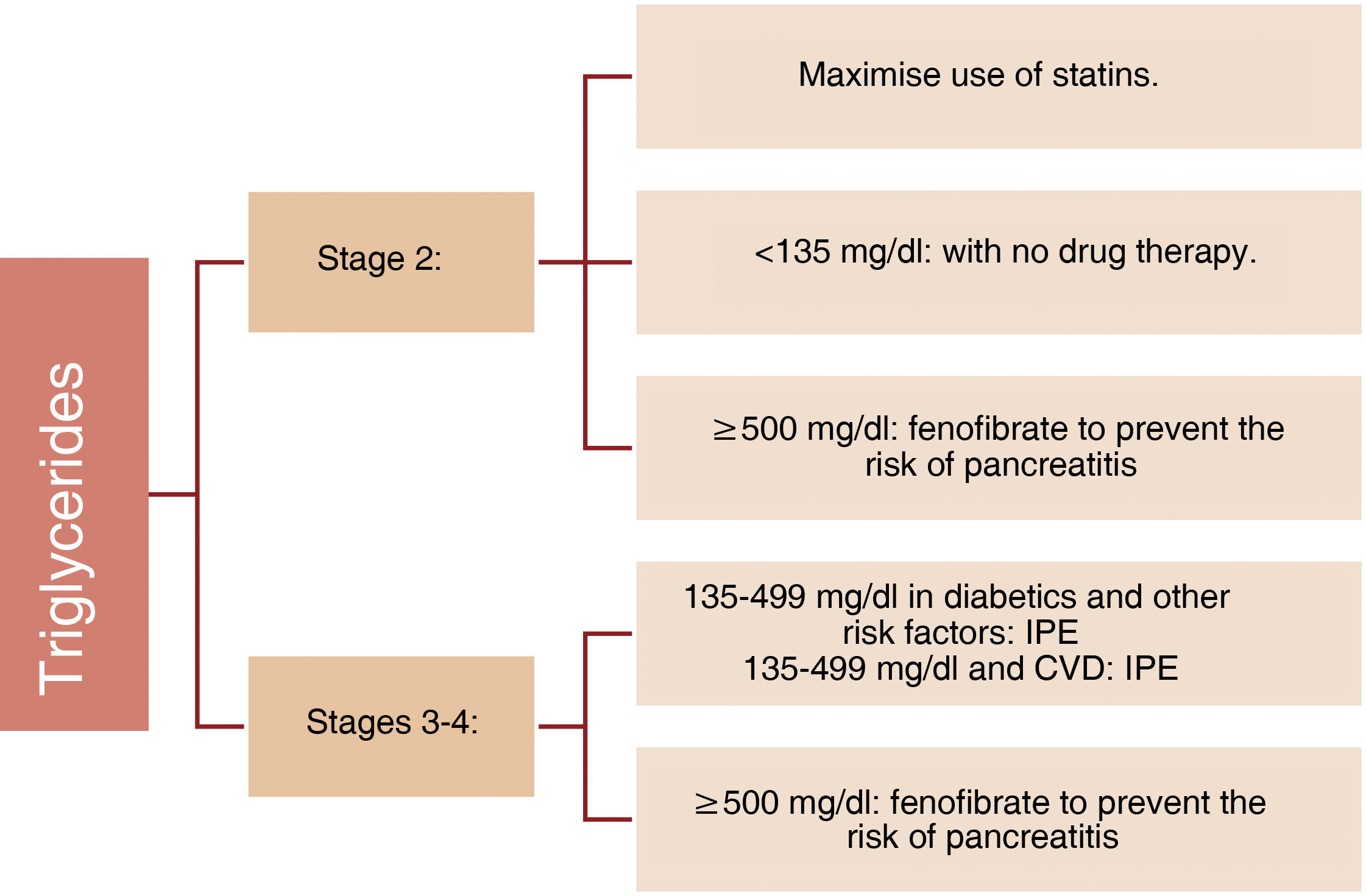
The advisory also provides guidance on the appropriate use of cardio- and nephroprotective therapies based on the components of metabolic syndrome, type 2 diabetes or presence of CKD (e.g., angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, statins, ezetimibe, PCSK9 inhibitors, SGLT-2 inhibitors, glucagon-like peptide-1 receptor agonists [GLP-1 RAs] and mineralocorticoid receptor antagonists [MRA] [finerenone]). It also proposes algorithms for the appropriate selection of new treatments (e.g., SGLT-2 inhibitors in CKD starting at moderate risk, in heart failure or in type 2 diabetic subjects with high risk of HF, or GLP-1 RAs in diabetic subjects with uncontrolled hyperglycaemia (haemoglobin A1c ≥9%), high doses of insulin or severe obesity (body mass index ≥35 kg/m2) to reduce the risk of CKD progression and the development of associated CVD. It is also advised to consider the combined use of SGLT-2 inhibitors and GLP-1 RAs in diabetic subjects with multiple CKM risk factors in the context of CVD or predicted high risk of CVD (Figs. 1–3).14
Management of LDL cholesterol in the different stages of CKM syndrome.
CKD: chronic kidney disease; DM-2: type 2 diabetes; eGFR: estimated glomerular filtration rate; LDLc: LDL cholesterol; uACR: urine albumin-creatinine ratio.
Modified from Ndumele et al.14
Management of triglycerides in the different stages of CKM syndrome.
CVD: cardiovascular disease; IPE: icosapent ethyl.
Modified from Ndumele et al.14
Clinical management of the remaining comorbidities in the different stages of CKM syndrome.
ACEI: angiotensin-converting enzyme inhibitors; ARBs: angiotensin II receptor blockers; ARNI: angiotensin receptor/neprilysin inhibitor; BMI: body mass index; BP: blood pressure; CKD: chronic kidney disease; CKM: cardiovascular-kidney-metabolic; DPP-4i: dipeptidyl peptidase 4 inhibitors; eGFR: estimated glomerular filtration rate; GLP-1 RA: GLP-1 receptor agonists; HbA1c: glycosylated haemoglobin; HTN: arterial hypertension; HF: heart failure; HFpEF: heart failure with preserved ejection fraction; HFrEF: heart failure with reduced ejection fraction; MRAs: mineralocorticoid receptor antagonists; OADs: oral antidiabetics; SGLT-2 inhibitors: sodium-glucose cotransporter type 2 inhibitors.
Modified from Ndumele et al.14
The advisory emphasizes that collaborative and comprehensive care strategies, including value-based and volume-based models, that support interdisciplinary care,53 can help to reduce the fragmentation of current healthcare based on subspecialty “silos” and improve treatment and clinical outcomes for patients with multiple comorbid conditions within CKM syndrome.54 It also proposes the generation of multidisciplinary teams, which, together with community associations, can help to mobilise resources to provide a more effective response.14 The advisory proposes that these multidisciplinary units should provide protocolized guidance coordinated with primary care to subjects with two or more CKM syndrome conditions (diabetes, CKD or clinical/subclinical CVD) with referrals to subspecialists for high-risk subjects. This aspect is important, particularly with regard to Nephrology, given the limited knowledge and confidence of primary care in the management of CKD patients.55 As such, this strategy may improve the care of CKM syndrome patients in primary care56 with the support of multidisciplinary teams, which can allow for more fluid communication than currently exists between primary care and nephrology and other involved specialties.
In this sense, coordination between the different scientific societies (primary care, nephrology, cardiology, endocrinology) is warranted, together with patient associations and health authorities to establish a strategy to address CKM syndrome and that includes preventive initiatives, early diagnosis and treatment along the entire CKM syndrome spectrum.
The advisory also highlights the need for equitable access to specialised treatment, new drugs and bariatric surgery for these subjects, especially the most vulnerable.
Importance of adverse social determinants of healthGiven the increased prevalence of CKM syndrome among individuals with ASDH, defined as economic, social, environmental and psychosocial factors that affect health over the life course and negatively impact CKM syndrome management and outcomes, the advisory emphasises screening for ASDH, proposes validated tools for its detection, incorporates ASDH into risk prediction and provides these subjects with equitable access to resources to enable the attainment of healthy lifestyles as part of the clinical care model for subjects with CKM syndrome. In Spain, these social conditions are also associated with less healthy lifestyles,57,58 so it seems appropriate to consider them here as well, although with tools validated in Spain. In fact, the Spanish Ministry of Health has recently published the ASDH that should be included in the digital medical record to facilitate the biopsychosocial, family and community approach.59
Risk assessment in CKM syndrome: CV risk calculatorThe new CV risk calculator is the result of a paradigm shift regarding CVD risk since metabolic diseases, including obesity, diabetes and CKD, multiply the risk of developing CVD. Therefore, the new calculator has included these conditions together with traditional risk factors, such as smoking, blood pressure and cholesterol levels. For the first time, the risk of heart failure is included in the calculation of the total risk of CVD and can be calculated separately, reflecting its high prevalence in subjects with diabetes and/or CKD. Furthermore, instead of evaluating risk factors according to race, as has classically been the case, the new models do not take race into consideration, opting instead to consider the ASDH to estimate the risk of CVD.17
This initiative goes beyond those of the Chronic Kidney Disease Prognosis Consortium (CKD-PC), which at one time created “corrections” that incorporated renal function measurements to improve the prediction of CV risk for the risk equations: the American Pooled Cohort Equation (PCE) and the European Systematic COronary Risk Evaluation (SCORE).60
Owing to the fact that few young people have a high 10-year risk of CVD, the new equation includes 30-year risk estimates from the age of 30 onwards, which is particularly useful for early counselling and prevention. However, assessment of absolute risk at 10 years, together with relative risk reduction with specific treatments, remains essential for considering the benefits and risks of these treatments in older subjects.
The inclusion of new predictive variables, such as kidney function (eGFR) and albuminuria (uACR), HbA1c, and ASDH, and the expansion of included CV events (e.g., HF) may help clinicians prevent CVD earlier and more comprehensively, by recommending lifestyle changes along with treatments to modify traditional CVD risk factors during early adulthood, as well as considering the possibility of metabolic diseases and CKD developing as subjects grow older.
One limitation of this equation is that it is designed for North American subjects, so a similar initiative in Europe (Spain) would be desirable.
Opportunity for CKM syndrome recognition in Nephrology and limitationsCKD is a growing public health problem, its main risk factors are shared with CVD (diabetes, hypertension, obesity, etc.) and it is a recognised CV risk factor.1–3 However, it is underdiagnosed, especially in measuring albuminuria (uACR) in subjects at risk,61 and under-recognised, especially in the early stages.62,63 In Spain and in our setting, two thirds of subjects with CKD are not diagnosed,64–66 while diagnosis is associated with an improvement in treatment and a delay in CKD progression.67 There is also a lack of recognition of its relevance among health authorities in terms of its prevalence, clinical impact, burden on the health system and even economic and environmental impact, probably because CKD has been associated with advanced stages (categories G4–G5 and renal replacement therapy), which are those managed by Nephrology and whose prevalence is very limited (<1% of the general population), even though they have great clinical, economic and environmental impact.3,68
This advisory emphasizes that kidney health is closely linked to CV health, and acknowledges the relevance of measuring parameters of kidney function and injury (both elevated albuminuria and decreased glomerular filtration rate) within CKM syndrome in CV risk, which can help in recognising CKD as a priority non-communicable disease (as are diabetes mellitus and CVD) and contribute to improving CKM health, reducing long-term CV and renal risk and the consequences of advanced CKD. The implementation of strategies to reduce the risk of CKM (primordial and primary prevention) and risk assessment from early stages, early diagnosis and recognition of CKD, and its early management with the classic and new therapeutic arsenals, can help reduce its high morbidity and mortality, especially CV, of subjects with CKD, as well as reduce the need for renal replacement therapy, and its significant clinical implications (deterioration of quality of life for the subject and their loved ones, on the health system, and environmental implications of advanced CKD or kidney failure).1,64,66 Especially in a context in which an increase in CKD and its care burden is expected in the near future.1 It can also increase awareness of the importance of kidney health and screening in primary care or other specialties, promote widespread and equitable access to cardio-renoprotective drugs and promote education on kidney health in subjects at risk of, or living with CKD.69 It would also be desirable to promote an increase in research into CKD.69
However, it is important to remember that there are causes of CKD unrelated to CKM syndrome, which contribute to it, but which may not be preventable with preventive measures, although they are included in it as they are also associated with an increase in CV risk.14 The non-CV consequences of CKD, which include increased premature mortality from any cause, as seen during the COVID-19 pandemic, should also be remembered.70 Furthermore, within cardiorenal syndrome (CRS) there is a specific subtype of syndrome that differs substantially from CKM syndrome, both in its pathophysiology and in the therapeutic approach: namely, CRS type 2 (kidney disease secondary to chronic heart disease, especially when it is structural or due to storage disease). These subjects have traditionally been left out of most randomised clinical trials where the benefit of the main therapeutic options currently used in subjects with HF and/or CKD has been tested,4 and most drugs with cardiac prognostic benefit (beta-blockers, MRA or angiotensin receptor/neprilysin inhibitor [ARNI]) have shown questionable benefit in these subjects. Management of congestion and therapy aimed at optimising cardiac functional class (implantable cardiac devices, resynchronisation therapy, treatment of storage disease or even heart transplant) usually are the basis of the approach adopted for subjects of this type, and although management of CV risk factors cannot be ignored in these subjects, optimisation of depletive treatment with the occasional need for haemofiltration or peritoneal dialysis when diuretic resistance progresses, can be key in the management of these subjects. In addition, the advisory recognises that, even though the scientific evidence supporting the concept that CKM syndrome increases health risks in general is sound, it acknowledges that certain knowledge gaps do exist, such as the mechanisms that link CKM syndrome to HF or arrhythmias, or the relationship between CVD and the development of CKD. It also recognises gaps in CKM syndrome prevention and treatment strategies that should be the subject of future research. Finally, it should be noted that this presidential advisory focuses on the North American population, so a European/Spanish adaptation and the development of a CV risk calculator would be warranted. This document is not intended to be a guide, in fact aspects characteristic of a specific guide (e.g., criteria for referral to different specialists) are not covered.
ConclusionsThe value of the AHA presidential advisory lies in its comprehensive approach to a complex problem, and it proposes an early, progressive, equitable and multidisciplinary approach, focused particularly on prevention (from primordial to secondary). This advisory unifies many individual concepts that physicians are already familiar with and provides an approach that is easier to implement and communicate among specialists, to subjects and to health authorities. This should allow preventive and treatment measures to be implemented earlier in life and in a more effective way in order to reduce high CV morbidity and mortality and reduce the risk of CKD development/progression to more advanced stages. For Nephrology, it also means the implicit recognition of CKD as a priority non-communicable disease, along with diabetes and CVD. Nephrologists must take advantage of this opportunity to lead the prevention of, and early approach to CKD in the context of CKM syndrome and develop multidisciplinary guidelines/teams for the proper management of these subjects in collaboration with other scientific societies/specialists, with the support of patient associations and the administration; these strategies can lead to improvements of patients, reduce CV and renal risk, and reduce the health, economic and environmental burden of CKM syndrome, especially associated with advanced CKD or kidney failure.
Key points- •
CKM syndrome is a progressive, multi-organ disease that exists as a spectrum ranging from risk to clinical disease.
- •
Excess or dysfunctional adiposity is hypothesised to be the substrate of CKM syndrome. Improving integrated obesity care is essential to prevent the progression of this syndrome.
- •
The risk of CKM syndrome begins early in life and is aggravated by ASDH throughout life.
- •
Periodic albuminuria and kidney function measurements are key elements for predicting incident cardiovascular disease (CVD) in subjects with CKM stage 2 or higher.
- •
New drugs and treatments aimed at treating CKM syndrome should be available for widespread, equitable prescription, with an emphasis on implementation in populations with highest risk of disease progression.
- •
CKM syndrome equates CKD with other conditions recognised as priority non-communicable diseases due to their impact on morbidity and mortality, and initiatives are in place to ensure that it is recognised as such by the WHO.71
This article has been funded by public funds: grants to support the scientific activity of research groups in Catalonia from the Agencia de Gestión de Ayudas Universitarias y de Investigación [University and Research Grants Management Agency] of the Generalitat de Catalunya [Government of Catalonia] (AGAUR 2021-SGR-01118).