Chronic kidney disease (CKD) affects 9% of the adult population in Spain.1,2 The majority of patients with CKD are managed by primary care physicians,3–6 and early detection is essential for adopting the measures required to slow its progression.7,8 At the primary care clinics, the physician includes in the electronic medical record the diagnosis of chronic kidney disease (CKD) manually when the estimated glomerular filtration rate (GFR) is lower than 60ml/min/1.73m2. The objective of the study is to determine, in patients with a GFR<60ml/min/1.73m2, whether documenting a diagnosis of CKD in the record encompasses different attitudes with respect to the prevention and treatment of CKD.
The study was performed in the 16 primary care teams from the Muntanya Primary Care Service (SAP) in Barcelona, belonging to the Catalan Health Institute (ICS), where 212,321 adult patients were covered for health care in 2012. Patients with a minimum of 2 estimated glomerular filtration rates (eGFRs) using the CKD-EPI formula lower than 60ml/min/1.73m2 in 2012 were enrolled. We identified two groups of patient depending of whether to diagnosis of CKD had been recorded in the medical history. A between-groups comparison was performed using the chi-squared test for qualitative variables and Student's t test for quantitative variables. A level of statistical significance of 5% (p≤0.05) was accepted.
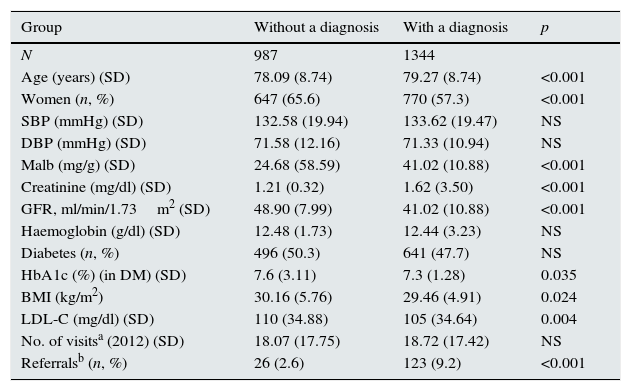
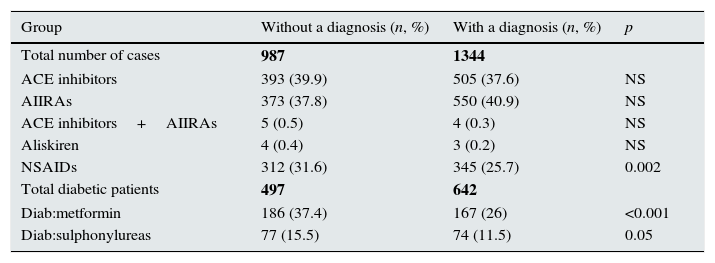
In 2331 patients, at least 2 eGFR measurements <60ml/min/1.73m2 were recorded. The diagnosis of CKD had been recorded in 1344 patients (57%), but not in 987 patients (43%). Table 1 summarises the patients’ characteristics. The patients with a recorded diagnosis of CKD had a lower eGFR and greater albuminuria. The proportion of diabetics was similar in the two groups. Body weight, LDL cholesterol and glycated haemoglobin in patients with diabetes were lower in the group of patients with a diagnosis of CKD. Table 2 summarises the treatment in both groups. The use of renin–angiotensin system inhibitors was similar in the both groups. By contrast, the use of non-steroidal anti-inflammatory drugs was lower in patients with the diagnosis of CKD. In diabetic patients the use of metformin and sulphonylureas was also lower in the group with a diagnosis of CKD.
Sociodemographic data and mean baseline values.
| Group | Without a diagnosis | With a diagnosis | p |
|---|---|---|---|
| N | 987 | 1344 | |
| Age (years) (SD) | 78.09 (8.74) | 79.27 (8.74) | <0.001 |
| Women (n, %) | 647 (65.6) | 770 (57.3) | <0.001 |
| SBP (mmHg) (SD) | 132.58 (19.94) | 133.62 (19.47) | NS |
| DBP (mmHg) (SD) | 71.58 (12.16) | 71.33 (10.94) | NS |
| Malb (mg/g) (SD) | 24.68 (58.59) | 41.02 (10.88) | <0.001 |
| Creatinine (mg/dl) (SD) | 1.21 (0.32) | 1.62 (3.50) | <0.001 |
| GFR, ml/min/1.73m2 (SD) | 48.90 (7.99) | 41.02 (10.88) | <0.001 |
| Haemoglobin (g/dl) (SD) | 12.48 (1.73) | 12.44 (3.23) | NS |
| Diabetes (n, %) | 496 (50.3) | 641 (47.7) | NS |
| HbA1c (%) (in DM) (SD) | 7.6 (3.11) | 7.3 (1.28) | 0.035 |
| BMI (kg/m2) | 30.16 (5.76) | 29.46 (4.91) | 0.024 |
| LDL-C (mg/dl) (SD) | 110 (34.88) | 105 (34.64) | 0.004 |
| No. of visitsa (2012) (SD) | 18.07 (17.75) | 18.72 (17.42) | NS |
| Referralsb (n, %) | 26 (2.6) | 123 (9.2) | <0.001 |
DM, diabetes mellitus; GFR, glomerular filtration rate; HbA1c, glycated haemoglobin; BMI, body mass index; LDL-C, LDL cholesterol; Malb, microalbuminuria; NS, p>0.05; DBP, diastolic blood pressure; SBP, systolic blood pressure.
a Any visit to the site for any reason has been counted.
b Referrals to the Nephrology Department of the referral hospital.
Treatment differences according to group.
| Group | Without a diagnosis (n, %) | With a diagnosis (n, %) | p |
|---|---|---|---|
| Total number of cases | 987 | 1344 | |
| ACE inhibitors | 393 (39.9) | 505 (37.6) | NS |
| AIIRAs | 373 (37.8) | 550 (40.9) | NS |
| ACE inhibitors+AIIRAs | 5 (0.5) | 4 (0.3) | NS |
| Aliskiren | 4 (0.4) | 3 (0.2) | NS |
| NSAIDs | 312 (31.6) | 345 (25.7) | 0.002 |
| Total diabetic patients | 497 | 642 | |
| Diab:metformin | 186 (37.4) | 167 (26) | <0.001 |
| Diab:sulphonylureas | 77 (15.5) | 74 (11.5) | 0.05 |
NSAIDs, non-steroidal anti-inflammatory drugs; AIIRAs, angiotensin II receptor antagonists; Diab, diabetic; ACE inhibitors, angiotensin converting enzyme inhibitors; NS, p>0.05.
Bold values represent the number of patients.
The main observation of the present study is that a diagnosis of CKD is made late and that the diagnosis is not shown in the medical history of approximately 40% of patients with an eGFR<60ml/min/1.73m2. Despite the greater severity of kidney disease, patients with a diagnosis of CKD recorded had less overweight and better control of LDL cholesterol and glycated haemoglobin (in diabetic patients). The use of non-steroidal anti-inflammatory drugs was lower in the group of patients with a diagnosis of CKD. Metformin and sulphonylureas were used less often in diabetic patients with a diagnosis of CKD. Taken together, these results suggest that a diagnosis of CKD is associated with a more proactive attitude aimed at decreasing risk factors for cardiovascular problems and for progression of kidney disease and also with greater prevention of acute renal failure. These findings raise the question of whether automatically including a diagnosis of CKD in the medical history of patients with an eGFR<60ml/min/1.73m2 might foster a more proactive attitude in the treatment of these patients.9,10 However, these results should be interpreted with caution since this is a retrospective study and therefore does not allow causal relationships to be established. Conforming or refuting this hypothesis would require a prospective randomised study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Carme Nebot. Servei d’atenció primària Muntanya Dreta.
Pilar Algueró. Centre d’atenció primària Turó.
Maribel Colas. Centre d’atenció primària Turó.
Joan Atmetlla Andreu. Centre d’atenció primària Xafarinas.
Dolors Llauradó. Centre d’atenció primària Turó.
Araceli Martín. Centre d’atenció primària Ciutat Meridiana.
Andrea Sánchez Callejas. BASIQ. Unitat d’Avaluació, Sistemes d’Informació i Qualitat.
Francisca Benavides. Centre d’atenció primària Rio de Janeiro.
Eladio Fernández-Liz. Area del Medicament Àmbit Barcelona Ciutat.
Daniel Serón. Servei de Nefrologia. Hospital Universitari Vall d’Hebrón. Barcelona.
Eugenia Espinel. Servei de Nefrologia. Hospital Universitari Vall d’Hebrón. Barcelona.
The names of participants in the study are available on Appendix.
Please cite this article as: Espinel E, Benavides F, Feijóo MV, Fernández-Liz E, Cossio Y, Serón D, et al. Registro del diagnóstico de insuficiencia renal crónica en la historia clínica electrónica y su influencia en el manejo terapéutico. Nefrología. 2016;36:315–317.