Last decade, the number of patients treated with home haemodialysis (HHD) worldwide has increased considerably1; this is in part due to the clinical benefits of more intensive haemodialysis (HD) regimens in HHD.2–5 In Spain, however, despite a growing interest and modern systems that simplify HHD, the number of patients using HHD has not increased substantially.6 We administered a survey to Spanish nephrologists, sent mainly by e-mail through the Spanish Society of Nephrology, to learn more about the barriers for implementing HHD in Spain.
Between February and November of 2015, we received 142 surveys from 76 different HD units, 60 of them hospital-based and 16 out-of-hospital (mean age of surveyed: 44.69±10.55 years). HHD programmes were available in 32 of these centres (42.1%); 15 (19.73%) offered the option even though they did not have their own HHD unit, and in 29 (38.15%) the patients were not offered this possibility. All the HHD units were hospital-based, with no HHD programmes dependent on peripheral HD centres, in which it was only offered in 18.7% of cases (compared with 73.3% of HHD offerings performed in hospitals). 47% of HHD programmes were started after 2011; 23% between 2006 and 2010; 13% between 2001 and 2005; and 17% before 2000. In all, 60.5% of the nephrology units stated that they would be capable of offering their own HHD programmes within one year's period.
The median number of patients per HHD unit was 2 (range: 0–17); 59.4% of the centres had 2 patients or fewer; and only 12.5% had 6 patients or more. The nephrologist in charge of the HHD programme in 42% of the cases was also responsible for HD; in 32% for peritoneal dialysis (PD); and in 26% for both methods. In 46% of the cases the patients came from HD at the centre; 22% from PD; 25% from outpatient clinics; and 7% from renal transplantation.
We asked the nephrologists for their opinions about any clinical benefits of HHD. We obtained the highest percentage of affirmative responses in regard to quality of life (95.8%), and the lowest in regard to mortality (67.6%). As for anaemia, high blood phosphate levels, blood pressure, nutrition and morbidity, opinion was in favour of HHD in 80.3%, 84.5%, 87.3%, 88% and 76%, respectively. In addition, 85.9% of the surveyed said that HHD could produce economic benefits to the health service. In total, 45.8% of the nephrologists said that living far from the referral centre was a factor favouring implementing of HHD and, did not compete with PD, according to 52.8% of the responses.
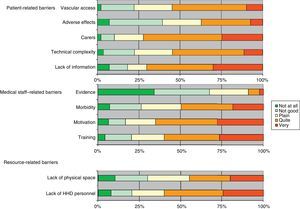
We asked about possible barriers for the development of HHD by dividing them into patient-related factors (lack of information, technical complexity, need for carers, fear of acute adverse effects of the method and difficulty with vascular access); medical staff-related factors (lack of properly trained medical personnel, lack of personnel motivated to perform home methods, consideration of excessive patient morbidity, lack of scientific evidence in favour of HHD); and resource-related factors (lack of equipment to work with HHD, lack of a physical space to conduct training) (Fig. 1).
Next, we divided the barriers according to the size of the HHD unit (Table 1), to see whether they varied depending on whether the nephrologist had more experience with the home method.
Patient-, medical staff- and resource-related barriers by size of centre.
| Type of centre per patient | ||||||||
|---|---|---|---|---|---|---|---|---|
| 3 or more | 2–1 | None | ||||||
| Yes | Yes % | p | Yes | Yes % | p | Yes | Yes % | |
| Lack of information | 31 | 79.5 | 24 | 68.6 | 41 | 65.1 | ||
| Technical complexity | 14 | 36.8 | Sig. | 21 | 61.8 | 38 | 61.3 | |
| Carers | 20 | 51.3 | Sig. | 30 | 85.7 | 48 | 77.4 | |
| Adverse effects | 3 | 7.7 | Sig. | 11 | 31.4 | Sig. | 37 | 58.7 |
| Vascular access | 14 | 35.9 | 19 | 55.9 | 41 | 66.1 | ||
| Training | 30 | 76.9 | Sig. | 17 | 48.6 | 35 | 55.6 | |
| Motivation | 29 | 74.4 | 22 | 62.9 | 38 | 60.3 | ||
| Morbidity | 14 | 35.9 | 16 | 45.7 | 38 | 60.3 | ||
| Evidence | 1 | 2.6 | 3 | 8.6 | 8 | 13.1 | ||
| Personnel | 24 | 61.5 | 16 | 45.7 | Sig. | 42 | 66.7 | |
| Space | 20 | 51.3 | Sig. | 10 | 28.6 | Sig. | 31 | 50.0 |
Sig: statistical significance between types of centre p<0.05.
This survey showed that there is a growing interest in HHD on the part of Spanish nephrologists. The data must be analysed by considering that all surveys are answered mainly by those who are the most interested in the subject being investigated, and therefore we are aware that this real interest in the method may be overvalued and the possible barriers greater than what has been expressed. In any case, it seems that as HHD programmes develop, the initial barriers, which stem from a lack of practical knowledge of the method, are disappearing7,8 and only resource-related barriers remain9,10 (lack of information, training and personnel dedicated exclusively to HHD).
From the HHD Support and Promotion Group in Spain, we must focus our efforts on showing the results obtained in regard to generating HHD programmes, trusting that in the coming years the barriers stated in this survey – and which in many cases prevent this method of treatment from being offered to all patients as one more option to improve their quality of life – may be problems that will be overcome.
Please cite this article as: Pérez Alba A, Slon Roblero F, Castellano Gasch S, Bajo Rubio MA. Barreras para el desarrollo de la hemodiálisis domiciliaria en España. Encuesta a nefrólogos españoles. Nefrologia. 2017;37:665–668.