The objective of this protocol is to know which tests are needed to study an anemia in a patient with chronic kidney disease, the differential diagnosis of renal anemia, to know and correct other deficiency anaemias, and the criteria for referral to Nephrology or other specialties of the anemic patient with chronic kidney disease.
El objetivo del protocolo es conocer qué estudios deben solicitarse ante una anemia en un paciente con enfermedad renal crónica, el diagnóstico diferencial de la anemia renal, conocer y corregir otras anemias carenciales y los criterios de remisión del paciente anémico con enfermedad renal crónica a Nefrología u otras especialidades.
Anemia is a frequent complication of chronic kidney disease (CKD) and it is associated with a decrease in the quality of life of patients, it causes an increase in morbidity and mortality and accelerates the rate of progression of CKD. In patients with CKD, anemia is defined as the situation in which the concentration of hemoglobin (Hb) in the blood is below 2 times the SD of the mean Hg of the general population, corrected for age and sex.
The main cause of anemia in CKD is the inadequate production of endogenous erythropoietin, a hormone that acts on the differentiation and maturation of the red blood cells precursors. Other contributing factors have been recognized in recent years as a impaired response of the bone marrow to erythropoietin caused by uremic toxins, inflammation, decreased availability of iron for erythropoiesis and increased levels of hepcidin, a shortened of red blood cells (RBC) half-life or vitamin deficiencies (vitamin B12 or folic acid), among others.1
In CKD anemia may occur at early stages (CKD stages 2 and 3, of the KDIGO guidelines). The Hb levels decreases when the estimated glomerular filtration rate (eGFR) is around 70ml/min/1.73m2 (men) and 50ml/min/1.73m2 (women). However anemia is more common in CKD stage 4 (even earlier in diabetic patients) and worsens as CKD progresses. In advanced stages of CKD and in the dialysis population anemia is present in as high as 90% of patients.2,3
The presence of anemia in patients with mild to moderate reduction in eGFR can be interpreted as of renal origin, however other factors may be contributing, In this cases It is important to identify iron deficiency anemia, which is the most frequent cause of anemia – especially in patients receiving antiplatelet or anticoagulant treatments – or of other types of anemia such as deficiency of vitamin B12 or folic acid. Sometimes both types of anemia, renal and iron deficiency may coexist.
Objectives of the present manuscript- -
Recognize that in patients with reduced eGFR (<60ml/min/1.73m2) there may be anemia, whose frequency increases with the severity of the disease (stage ≥4) and, therefore, a blood count should be requested periodically.
- -
To learn which additional tests should be requested in case of anemia in a CKD patient, to rule out other concomitant causes of anemia (especially iron deficiency).
- -
To know what and how to correct other deficiencies (especially iron deficiency) before classifying anemia as a of renal origin and be referred to a Nephrologist.
- -
Establish when a CKD patient with anemia should be referred to the nephrologist for prescription of intravenous iron or erythropoiesis stimulating agents (ESA) and when the patients should be referred to other specialties (Hematology, Internal Medicine or others).
- -
To know the targets for Hb, iron and others parameters in anemic CKD patients with and without ESA treatment.
The following threshold values for Hb (Hb <13g/dl in men, Hb <12g/dl in women) make the diagnosis of anemia, but do indicate the need for treatment. In case of unexplained low Hb level it is advisable to confirm this low value before starting a diagnostic work up.4
Diagnosis of anemia of chronic kidney diseaseCharacteristicsThe anemia associated with CKD is usually normocytic and normochromic and without iron deficiency (ferritin >100ng/ml and transferrin saturation index [TSAT], >20%). If other parameters are found to be abnormal other causes of anemia should be suspected.
It should be kept in mind that the diagnosis of renal anemia is a diagnosis by exclusion, that is, when a patient has CKD and anemia and other causes have been excluded.
When to start the evaluation of anemia in chronic kidney disease?The patient should undergo evaluation for anemia as soon as the Hb is reduced (Hb <13g/dl in men or <12g/dl in women),5 or at least, and according to the consensus document on CKD6:
- •
When the value of Hb is <11g/dl in premenopausal women and prepubertal patients.
- •
When the value of Hb is <12g/dl in adult men and postmenopausal women.
According to the KDIGO guidelines, hemoglobin levels should be measured in patients with CKD5:
- a)
In patients WITHOUT known anemia, Hb levels should be measured when clinically indicated (development of anemia symptoms: asthenia, dyspnea, tachycardia, etc.) and:
- •
At least once a year in patients with CKD stage 3 (eGFR 60–30ml/min/1.73m2).
- •
At least 2 times a year in patients with CKD stage 4–5 who are not on dialysis (eGFR <30ml/min/1.73m2).
- •
At least every 3 months in patients with stage 5 dialysis (CKD-5D) in hemodialysis (HD) or peritoneal dialysis (PD)
- b)
In patients WITH anemia and not treated with ESA, Hb levels should be measured when clinically indicated and:
- •
At least every 3 months in patients with CKD stage 3–5 who are not on dialysis (CKD-ND) or stage 5D on PD.
- •
Monthly in patients with CKD 5D in HD.
- c)
In patients WITH anemia receiving ESA, Hb levels should be measured when clinically indicated and:
- •
Monthly in the correction phase.
- •
In the maintenance phase: in patients with CKD-ND (not in dialysis) at least every 3 months and in patients with CKD-5D (in Hemodialysis) monthly and every 2 months in patients with CKD-5D (in Peritoneal Dialysis).
- •
The initial study of anemia suspected to be of renal origin should always include5:
- -
Complete blood count with hemoglobin, red cell indices (MCV, MCH), leukocyte (and differential count) and platelet count.
- -
Absolute reticulocytes.
- -
Parameters of Iron metabolism: iron, ferritin, transferrin and trasnferrin saturation index (TSAT).
- -
Vitamin B12 and folic acid.
In patients with CKD-5D in Hemodialysis, it is recommended that samples be obtained immediately before the dialysis session and on the medweek day of the week.
Treatment of anemia in chronic kidney diseaseThe treatment of anemia associated with CKD is based on iron administration and ESA.
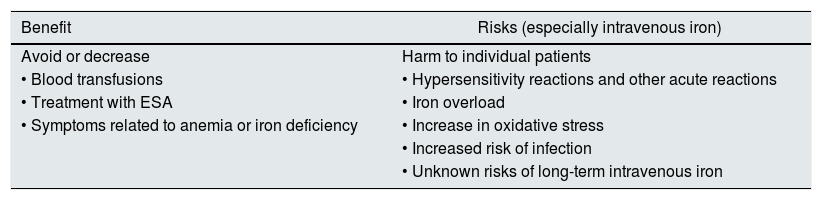
Indications of Iron therapyIron deficiency is frequent in patients with CKD and may cause anemia and hyporesponsiveness to ESA-EPO, so it must be corrected to ensure optimization of erythropoiesis. The administration of iron may produce an increase in Hb levels (even in the absence of evidence of iron deficiency) and, in some patients it allows to achieve the target Hb level. Iron parameters should be corrected before and during the treatment AEE, in order to achieve an adequate response that may even allow a reduction in the doses of doses of AEE EPO. However, although the risk-benefit balance is favorable, it should not be forgotten that iron therapy presents potential risks (especially intravenously) (Table 1).
Risk-benefit balance of iron therapy.
| Benefit | Risks (especially intravenous iron) |
|---|---|
| Avoid or decrease | Harm to individual patients |
| • Blood transfusions | • Hypersensitivity reactions and other acute reactions |
| • Treatment with ESA | • Iron overload |
| • Symptoms related to anemia or iron deficiency | • Increase in oxidative stress |
| • Increased risk of infection | |
| • Unknown risks of long-term intravenous iron |
- •
Absolute deficiency: depletion of iron reserves. Serum ferritin concentration <100ng/ml and TSAT <20%.
- •
Functional deficiency: TSAT <20% and a normal/high ferritin concentration. In this case the iron requirements for erythropoiesis in the bone marrow exceed the capacity for iron release from the reticulo-endothelial system.
- a)
Absolute iron deficiency (ferritin <100ng/ml and TSAT <20%).
- b)
To increase Hb concentration before initiation of ESA if the TSAT is <25% and ferritin <200ng/ml in CKD-ND (or ferritin ≪300mg/ml in CKD-5D).
- c)
In patients with CKD receiving ESA to increase the Hb levels or to reduce the dose of ESA if TSAT <30% and ferritin <300ng/ml.
Objective: ferritin 200–500ng/ml; IST ∼30%.
During treatment with iron, a TSAT of 30% and a ferritin of 500ng/ml should not be intentionally exceeded in patients with CKD-ND, or with ERC-5D.4 Iron parameters should be determined at least after 15 days of the last intravenous dose of iron; otherwise the values obtained may not be reliable.
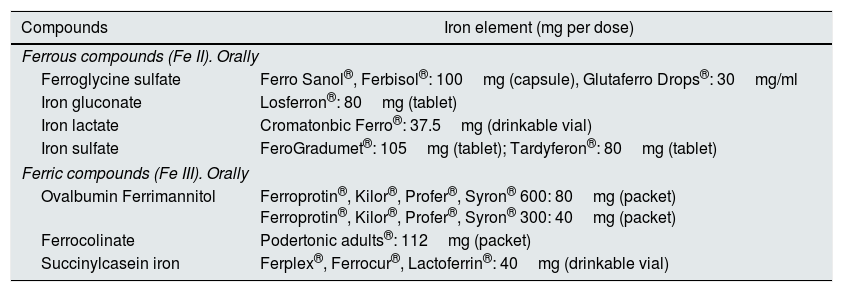
Oral iron administrationIn patients with CKD who are not on dialysis or peritoneal dialysis, it is preferable to start treatment with oral iron. The doses prescribed in an adult patient will be around 200mg/day of elemental iron divided into 2–3 doses (preferably ferrous salts for better absorption), and preferably in fasting conditions.
The main problems associated with oral iron therapy in CKD are gastrointestinal intolerance, problems of intestinal absorption or lack of compliance, which may require the patient to be sent to the hospital to receive iron intravenously (Table 2).
Available oral iron compounds.
| Compounds | Iron element (mg per dose) |
|---|---|
| Ferrous compounds (Fe II). Orally | |
| Ferroglycine sulfate | Ferro Sanol®, Ferbisol®: 100mg (capsule), Glutaferro Drops®: 30mg/ml |
| Iron gluconate | Losferron®: 80mg (tablet) |
| Iron lactate | Cromatonbic Ferro®: 37.5mg (drinkable vial) |
| Iron sulfate | FeroGradumet®: 105mg (tablet); Tardyferon®: 80mg (tablet) |
| Ferric compounds (Fe III). Orally | |
| Ovalbumin Ferrimannitol | Ferroprotin®, Kilor®, Profer®, Syron® 600: 80mg (packet) Ferroprotin®, Kilor®, Profer®, Syron® 300: 40mg (packet) |
| Ferrocolinate | Podertonic adults®: 112mg (packet) |
| Succinylcasein iron | Ferplex®, Ferrocur®, Lactoferrin®: 40mg (drinkable vial) |
In patients with CKD-not on dialysis, intravenous iron administration is indicated if:
- •
Targets of Iron parameters are not achieved with oral iron therapy for 3 months or when there is intolerance to oral iron or malabsorption.
- •
In patients with severe anemia and iron deficiency in whom a rapid Hb response is required.
- •
Patients with chronic inflammatory processes showing functional iron deficiency (TSAT <20% with normal-elevated ferritin), especially if they require ESA.
In most patients with CKD-5D in hemodialysis, since given their high requirements it is considered unlikely that they reach iron targets using oral iron, so they will need treatment with intravenous iron.
In patients with CKD-5D in peritoneal dialysis who present absolute or functional iron deficiency, especially if they receive ESA.
Since intravenous iron therapy requires its administration in a hospital center, its indication is a reason for referral to a nephrologist.5
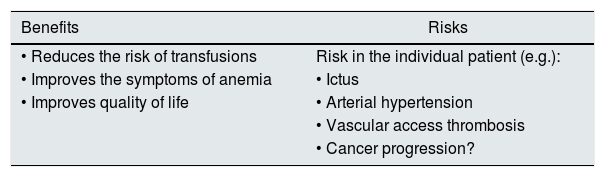
Indication of treatment with ESA-EPO in chronic kidney diseaseIf after ruling out or correcting other causes of anemia, the patient has adequate iron parameters and Hb is ≤10g/dl, the patient should be referred to Nephrology to assess the treatment with ESA (consider a value of Hb <11g/dl if the patient is young, active or with symptoms of anemia). ESAs are included in the group of outpatient hospital dispensing drugs.
The nephrologist should assess the benefits and risks of treatment with ESA in an anemic patient with CKD. As a general rule, in CKD adult patients treated with ESA, the Hb targets should be between 10 and 12mg/dl and always assessing symptoms and comorbidities. The total correction of anemia (Hb ≥13g/dl) during treatment with ESA-EPO is not indicated, since this Hb level it is not associated with an improvement in prognosis while there is an increased risk of adverse effects (hypertension, stroke, thrombosis of the vascular access, cancer progression, etc.)4,5 (Table 3).
The goal of Hb level will be individualized in each patient according to their age, degree of activity and the associated comorbidities, however Hb values ≥13g/dl should not be intentionally reached.
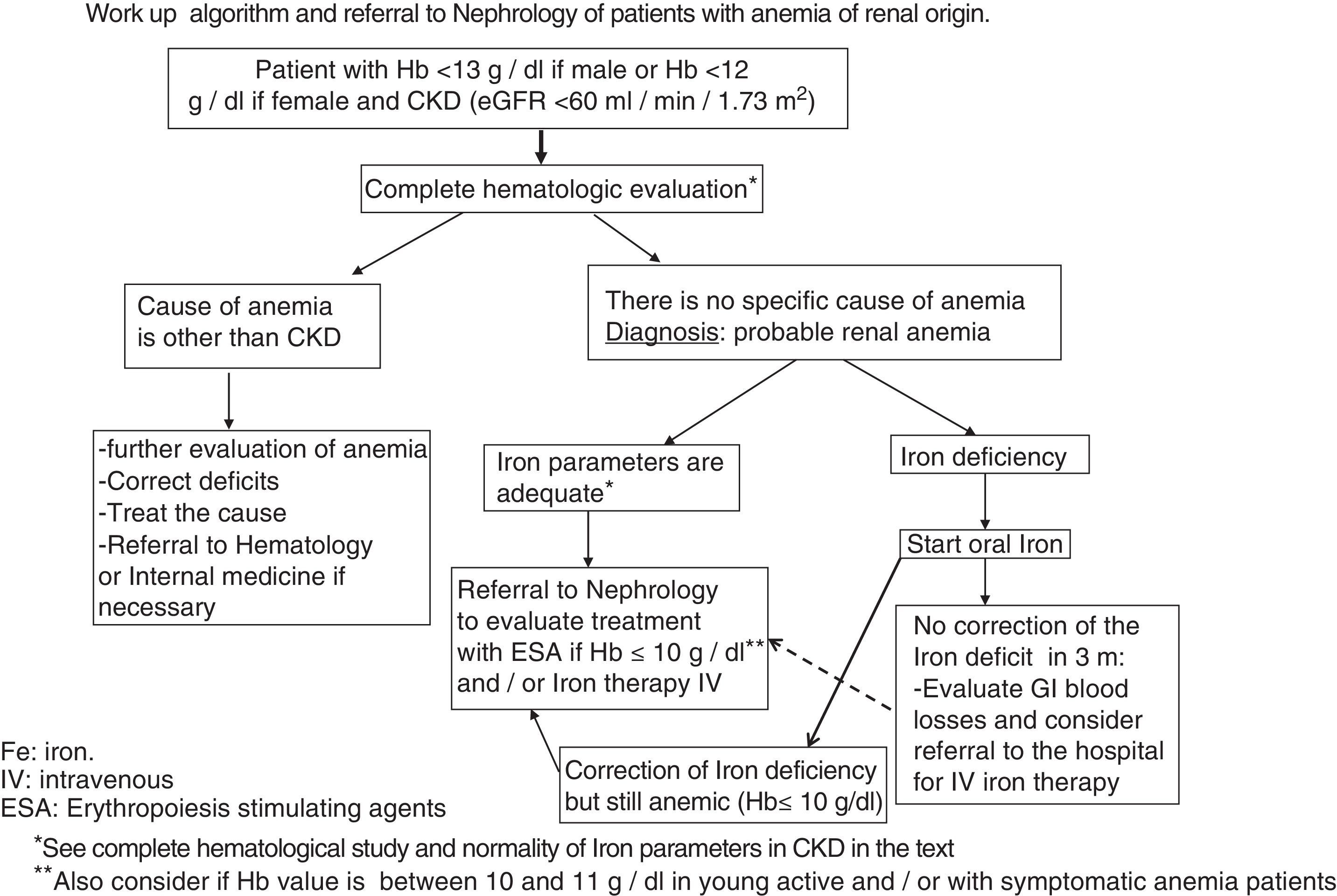
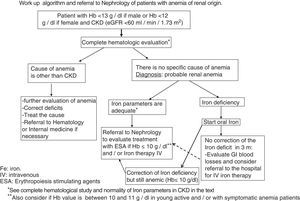
Referral to Nephrology for the management of anemiaThe indications for referral of a CKD patient with anemia should be (Fig. 1):
- •
Indication of intravenous iron therapy (failure/intolerance of oral Iron).
- •
Indication of treatment with ESA.
- •
In the patient treated with ESA with confirmed Hb ≥13g/dl or Hb ≤9g/dl that need dose adjustment.
- -
Anemia is a frequent complication in patients with CKD (eGFR <60ml/min/1.73m2), especially in CKD stage 4 or greater.
- -
The diagnosis of anemia due to CKD is a diagnosis of exclusion, so it is necessary to rule out other causes of anemia, especially iron deficiency.
- -
If after correction of all causes of anemia the patient persists anemic (Hb ≤10g/dl), he/she should be referred to a Nephrology Service to assess treatment with ESA. The patient should be also referred to Nephrology if there is indication of intravenous iron therapy or if the patient is treated with ESA and has Hb ≥13 or ≤9g/dl for dose adjustment.
The authors have no conflicts of interest to declare.
The authors want to acknowledge the different scientific societies for their support and involvement in the implementation of this document.
Please cite this article as: Cases A, Egocheaga MI, Tranche S, Pallarés V, Ojeda R, Górriz JL, et al. Anemia en la enfermedad renal crónica: Protocolo de estudio, manejo y derivación a Nefrología. Nefrologia. 2018;38:8–12.