Renal amyloidosis is one of the most severe complications of familial Mediterranean fever (FMF). Colchicine has reduced the incidence of this complication, which now only appears in untreated, under-treated and resistant patients, but it is usually ineffective in patients with advanced amyloidosis. Here we report a patient with FMF and biopsy-proven amyloidosis who presented with nephrotic syndrome despite colchicine treatment. Anakinra (an interleukin-1β inhibitor) was started and a dramatic complete remission of nephrotic syndrome was observed in the following months. Anakinra can be an effective treatment for FMF patients with severe secondary amyloidosis.
La amiloidosis renal es una de las complicaciones más graves de la fiebre mediterránea familiar (FMF). La colchicina ha reducido la incidencia de esta complicación, que ahora solo aparece en pacientes no tratados, tratados de manera insuficiente o resistentes al fármaco. No obstante, la colchicina se ha mostrado poco eficaz en pacientes que inician el tratamiento cuando la amiloidosis ya está presente. En este trabajo presentamos el caso de un enfermo con FMF y amiloidosis renal secundaria diagnosticada mediante biopsia renal que desarrolló un síndrome nefrótico completo a pesar del tratamiento con colchicina. Por la mala evolución del cuadro se decidió iniciar tratamiento con anakinra (un inhibidor de la interleucina 1β). En los meses posteriores a la instauración del fármaco el enfermo presentó una mejoría progresiva del síndrome nefrótico, hasta alcanzar la remisión completa. La función renal permaneció estable. Los inhibidores de la interleucina 1β pueden ser un tratamiento efectivo de la FMF en pacientes con amiloidosis renal secundaria.
Familial Mediterranean fever (FMF) is a hereditary inflammatory disease with an autosomal recessive pattern.1 It is caused by mutations in the MEFV gene, which codes for the protein pyrin. The abnormal synthesis of this protein leads to the dysregulation of various pathways involved in the control of inflammation (such as synthesis of interleukin-1β, activation of nuclear factor κβ, and apoptosis),2,3 which produces a sustained inflammatory state in patients with the disease. Clinically, FMF manifests as recurrent self-limiting episodes of fever and polyserositis. This maintained inflammation can lead to secondary amyloidosis (AA), which is one of the most devastating complications of this disease.4,5 Several studies have demonstrated the effectiveness of colchicine in the treatment of FMF, in reducing the frequency and severity of inflammatory episodes in affected patients and preventing the onset of AA.6,7 However, colchicine is not effective in patients with clinical manifestations of AA, particularly if there is renal amyloidosis.8,9 Anakinra, an interleukin-1β inhibitor, has been shown to be beneficial in the treatment of FMF, reducing the number of episodes of the disease.10 In this article we describe the first case of a patient with FMF and nephrotic syndrome (NS) secondary to AA with complete remission of NS after starting treatment with anakinra.
Clinical caseWe present the case of a 76-year-old man diagnosed in 1995 with FMF, on the basis of symptoms of recurrent, self-limiting episodes of abdominal pain and fever. Following this diagnosis, he was prescribed treatment with colchicine at a dose of 0.5mg every 12h, and he remained asymptomatic in subsequent years. In November 2010, the colchicine was stopped by his general practitioner, after which the patient started to experience episodes of polyarthralgia, chest pain, and abdominal pain. In January 2011 the patient was referred to our centre for investigation. On examination in clinic, the patient was afebrile, with a blood pressure of 95/71mmHg and a heart rate of 83 beats per minute. The only finding of note was mild ankle oedema. Investigations revealed a serum creatinine of 1.33mg/dL, serum albumin of 2.14g/dL, cholesterol of 285mg/dL, and triglycerides of 295mg/dL. Proteinuria was 6.1g/day. Urinary sediment showed 15 red blood cells per field. Other investigation parameters, including leukocytes, platelets, and haemoglobin, were normal. Mantoux test was negative.
Given the suspicion that the patient was experiencing new episodes of FMF, he was restarted on colchicine, and a genetic study was performed, which showed the M694 V mutation in the MEFV gene. Due to the presence of NS, a renal biopsy was performed: on optical microscopy, amorphous deposits were seen at a glomerular and vascular level. The deposits were Congo red positive. Electron microscopy revealed the presence of randomly arranged, unbranched fibrils measuring 8–10nm, characteristic of amyloidosis.
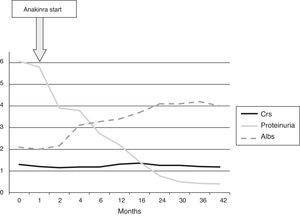
After establishing a diagnosis of NS secondary to AA, the dose of colchicine was increased to 1mg/12h, and enalapril was started to reduce proteinuria. These measures led to arterial hypotension and a deterioration in renal function, therefore enalapril was stopped. The NS worsened, requiring an increased dose of diuretics to control oedema, therefore in February 2011 it was decided to start treatment with anakinra at a dose of 100mg/day. Proteinuria began to decrease from the second month of treatment, and the patient had a partial remission of NS in the fifth month, as shown in Fig. 1. Complete remission of NS was achieved after 30 months of treatment (proteinuria<0.5g/day). At the most recent follow-up (42 months after starting anakinra), proteinuria was 0.4g/day, serum creatinine was 1.18mg/dL, and serum albumin was 4g/dL. The clinical progress of the patient has been good, with no new episodes of FMF. The patient has had no adverse effects related to the anakinra treatment.
DiscussionSecondary amyloidosis is a typical complication in patients with chronic inflammatory disorders.11 Familial Mediterranean fever is the classic hereditary inflammatory disease, and AA is one of its most important complications. The use of colchicine in FMF was increased after the publication of several studies demonstrating that it could prevent further episodes of the disease, and therefore reduce the risk of developing AA.7–9 Until colchicine was established as the first line treatment in patients with FMF, 60% of patients with this disease developed AA. Currently, thanks to the widespread use of colchicine, this prevalence has decreased to 7%.7 However, the effectiveness of colchicine is limited in patients with established amyloidosis.10 This limited response is particularly significant in patients with amyloidosis with renal involvement. Colchicine can stabilise or improve the condition when proteinuria is below the nephrotic range, but a poor response has been described in patients with established NS (proteinuria>3.5g/day and albumin<3g/dL).9–11 In addition, some patients are intolerant (2–3%) or resistant (5–10%) to colchicine.12 In these patients, and in those with advanced AA, the therapeutic options are limited.13 As mentioned in the introduction, mutations in the gene coding for pyrin leads to an inappropriate activation of interleukin-1β, which seems to be key in the pathogenesis of FMF.3 This discovery means that interleukin-1β inhibitors are a therapeutic option in patients with this disease.10,12
In the literature, 30 cases have been described of patients with FMF treated with anakinra. In 20 of them, there were no findings of AA, and treatment with anakinra was started because of a persistent inflammatory activity not controlled with colchicine.10,13–21 In the other 10 cases, renal amyloidosis was demonstrated. Of those 10 patients, 6 were on a long-term dialysis programme22–25 and 2 had received a transplant26,27 at the time of starting anakinra. These 8 patients were prescribed anakinra for the control of FMF inflammatory attacks. Only 2 patients23,28 were treated with anakinra with the aim of controlling glomerular proteinuria secondary to AA, and neither of these cases were in the nephrotic range. Both cases had a good clinical outcome, with renal function and proteinuria remaining stable after starting anakinra. In the 30 cases described, anakinra reduced or stopped inflammatory episodes, and very few adverse events were reported.
This is the first case described in the literature showing complete remission of NS secondary to amyloidosis secondary to FMF following treatment with anakinra. Starting anakinra prevented further episodes of the disease, and a progressive decrease in proteinuria, remaining below 0.5g/day from 30 months (complete remission). Renal function also remained stable. Although a follow-up renal biopsy would have been very needed to corroborate a reduction in amyloid deposit in the kidney, given the good clinical progress in this patient, it was decided not to perform this procedure. Anakinra may be a safe, effective, therapeutic alternative in patients with AA secondary to FMF with significant renal involvement; without treatment, these patients would probably progress to end-stage renal failure. It is likely that early treatment could lead to better outcomes. However, the cost of the drug and its possible adverse effects (increased infections, particularly respiratory and tuberculosis, and neutropenia)29 should influence appropriate patient selection before starting treatment is essential. More clinical information is needed to confirm our findings.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Sevillano ÁM, Hernandez E, Gonzalez E, Mateo I, Gutierrez E, Morales E, et al. Anakinra induce la remisión completa del síndrome nefrótico en un paciente con fiebre mediterránea familiar y amiloidosis. Nefrologia. 2016;36:63–66.