Infective endocarditis presents a 25% mortality. Acute kidney injury (AKI) develops in up to 70% of the cases. The aim of this study is to evaluate the predictive value of AKI in mortality due to endocarditis and to assess its associated factors.
MethodsUnicentric and retrospective study including all patients with in-hospital diagnosis of endocarditis between 2015 and 2021. Epidemiological data and comorbidities were collected at baseline. During admission, renal function parameters, infection-related variables and mortality were collected. Using adjusted multivariate models, LRA predictive value was determined.
ResultsOne hundred and thirty-four patients (63% males, age 72±15 years) were included. Of them 94 (70%) developed AKI (50% AKIN-1, 29% AKIN-2 and 21% AKIN-3). Factors associated to AKI were age (p=0.03), hypertension (p=0.005), previous chronic kidney disease (p=0.001), heart failure (p=0.006), peripheral vascular disease (p=0.022) and glomerular filtration rate (GFR) at baseline (p<0.001). GFR at baseline was the only factor independently associated to AKI (OR 0.94, p=0.001).
In-hospital deaths were registered in 46 (34%) patients. Of them, 45 (98%) patients had developed AKI. AKI was independently associated to mortality through diverse multivariate models. GFR loss (OR 1.054, p<0.001) and GFR at baseline (0.963, p=0.012) also predicted mortality during admission.
ConclusionsAKI development and its severity (GFR loss and AKIN severity) impacts in in-hospital mortality due to infective endocarditis.
La endocarditis infecciosa presenta una mortalidad del 25%. La lesión renal aguda (LRA) se desarrolla en hasta el 70% de los casos. El objetivo de presente estudio es determinar el impacto pronóstico de la LRA en la endocarditis y los factores asociados a la misma.
Materiales y métodosEstudio retrospectivo unicéntrico que incluyó a todos los pacientes ingresados por endocarditis entre 2015 y 2021. Basalmente se recogieron datos epidemiológicos y comorbilidades. Durante el ingreso, se recogieron datos de evolución de la función renal, variables asociadas con la propia infección y el desenlace de la misma. A través de modelos multivariables, se analizó la capacidad predictiva de la LRA en la mortalidad.
ResultadosSe incluyó a 134 pacientes (63% varones, edad media 72±15 años) de los que 94 (70%) presentaron una LRA (50% AKIN-1, 29% AKIN-2 y 21% AKIN-3). Los factores asociados a presentar una LRA fueron la edad, la hipertensión arterial, tener una enfermedad renal crónica, el FGe basal, padecer insuficiencia cardiaca y enfermedad vascular periférica. El único predictor independiente para presentar una LRA fue el FGe basal (OR 0,94, p=0,001).
Fallecieron 46 (34%) pacientes, de los que en 45 (98%) se desarrolló una LRA. A través de diversos modelos multivariantes ajustados, la LRA predijo independientemente la mortalidad. Asimismo, la pérdida de FGe (OR 1,054, p<0,001) y el FGe basal (0,963, p=0,012) se asociaron independientemente a fallecer durante la hospitalización.
ConclusionesEl desarrollo de una LRA y su gravedad, es decir, la pérdida de FGe y la puntuación en la escala AKIN, impactan en el pronóstico de una endocarditis infecciosa.
Infective endocarditis is a infrequent pathology with an estimated incidence in Spain of 3.1–3.7 cases per 100,000 inhabitants.1 Predisposing factors include rheumatic valve diseases, which are clearly decreasing in developed countries, degenerative valve diseases, diabetes mellitus, cancer, recreational intravenous drug use and congenital heart disease.2 Despite its low incidence and scientific advances in detection and treatment, its prognosis is poor: mortality rates are as high as 25%.3
Impaired renal function is a common complication of infective endocarditis, reaching up to 70% incidence in some populations.4 The importance of acute kidney injury (AKI) to any infectious process lies on the mechanisms that generate inflammatory dysregulation, microvascular disorders and changes in adaptive cellular programming, all of which aggravate the clinical situation.5 Regarding the endocarditis-AKD binomial, the published data are heterogeneous, given the irregular definition of AKI and the lack of etiological signals such as sepsis, nephrotoxicity, glomerular pathology or need for surgery.6–8 For all these reasons, there is no consensus on managing AKI.
Some factors have been shown to have an impact on the prognosis of infective endocarditis, the most prominent being those related to the baseline situation, mainly cardiovascular comorbidity. However, although renal function impairment is a common complication of infective endocarditis, its prognostic predictive power remains unknown.
The aim of this study is to assess the impact of AKI on mortality in patients hospitalized for infective endocarditis, and to investigate the factors associated with AKI.
MethodsPatientsThis is a single-center, observational, retrospective study, which included all patients with infective endocarditis between January 2015 and December 2021. Inclusion criteria were the need for hospitalization with a principal diagnosis of infective endocarditis according to Duke criteria9 and age of majority. Patients were excluded if: the current episode was a readmission (defined as a new hospitalization in less than 30 days after the previous one); they had a history of infective endocarditis, those who were lost to follow-up via transfer to another center, patients with multiple infections at admission, those in whom endocarditis had occurred as a complication during hospitalization or patients with stage 5 chronic kidney disease (CKD) on a renal replacement therapy program or with kidney transplant.
ObjectivesThe primary objective of this study was to determine the prognostic impact of renal function impairment in patients with infective endocarditis. Secondary objectives included the determination of factors associated with AKI, the description of clinical characteristics (presentation, complications, microorganisms involved) in infective endocarditis and the association between AKI severity and prognosis.
VariablesWe collected epidemiological variables (age, sex) and comorbidities (hypertension as defined by the International Society of Hypertension,10 diabetes mellitus, as per the American Diabetes Association (ADA) guidelines,11 dyslipidemia per the Kidney Disease: Improving Global Outcomes (KDIGO) Guidelines,12 history of ischemic heart disease, stroke and heart failure per the European Society of Cardiology (ESC) guidelines13). Regarding renal function, CKD and its stages were defined according to the KDIGO Guidelines.14 Glomerular filtration rate (GFR) was estimated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
During hospitalization, data were collected on valve involvement (type of valve affected and whether it was native or prosthetic), echocardiographic data on the infection, the responsible microorganism, development of bacteremia and persistent bacteremia, prescribed antibiotic therapy, evolution of infectious parameters and renal function (serum creatinine on admission and at peak) and outcome during admission. Using the data on renal function, the severity of AKI was established based on the Acute Kidney Injury Network (AKIN) scale.15 This scale uses an analytical criterion based on serum creatinine and urine flow to determine the stage, with higher stages corresponding to greater severity:
- none-
Stage 1: increase of 1.5–1.9 times the baseline creatinine value or increase of more than 0.3mg/dL or urine flow of less than 0.5mL/kg/h for more than six hours.
- none-
Stage 2: increase of 2–2.9 times the baseline creatinine value or the presence of urine flow of less than 0.5mL/kg/h for more than 12h.
- none-
Stage 3: increase of more than three times the baseline creatinine value, creatinine value of more than 4mg/dL or need for renal replacement therapy; or urine flow of less than 0.3mL/kg/h in 24h or anuria for 12h.
The etiology of AKI was established based on histological parameters, whether a renal biopsy had been performed, data collected in the clinical history and an a posteriori assessment by two nephrologists (among the authors of this study) who categorized AKI as functional, acute tubular necrosis, acute interstitial nephritis and multifactorial. The definition of etiology was based on urinary parameters and the evolution of AKI. Multifactorial causes included cases that could not be biopsied but had at least two diagnostic routes consistent with AKI.
Statistical methodsVariables are expressed as mean or median as measures of centralization and standard deviation or interquartile range as measures of dispersion. We compared parametric variables using the χ2 test for qualitative variables, Student's t-test for dichotomous and quantitative qualitative variables, ANOVA for non-dichotomous and quantitative qualitative variables, and Pearson's test for correlations between quantitative variables. In the case of non-parametric variables, we used Fisher, Mann-Whitney, Kruskal-Wallis and Spearman tests, respectively. Final variables (AKI and mortality) were analyzed by univariate and multivariate logistic regression, adjusted for confounding or relevant factors in different associative models. Statistical analyses were performed using SPSS 26.0®. Graphs were drawn using GraphPad 9.0® (GraphPad Software, San Diego, California, USA, www.graphpad.com). A value of p<0.05 was considered statistically significant.
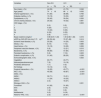
ResultsBaseline characteristicsA total of 134 patients (85 males [63%], mean age 72±15 years) were included. Baseline, 43 patients (32%) had chronic kidney disease distributed as follows: eight (19%) stage 2 patients, 16 (37%) stage 3a patients, 14 (33%) stage 3b patients and five (11%) stage 4 patients. Baseline estimated glomerular filtration rate (eGFR) was 76 (58–92) mL/min/1.73m2 (Table 1).
Baseline characteristics of included patients.
| Variables | All (n=134) | NoAKI (n=40) | AKI (n=94) | p |
|---|---|---|---|---|
| Sex (male), n (%) | 85 (63) | 29 (72) | 56 (60) | 0.175 |
| Age (years)a | 72±15 | 65±17 | 75±13 | 0.003 |
| Arterial hypertension, n (%) | 89 (66) | 19 (47) | 70 (74) | 0.005 |
| Diabetes mellitus, n (%) | 33 (25) | 9 (22) | 24 (25) | 0.828 |
| Dyslipidemia, n (%) | 65 (49) | 16 (40) | 49 (52) | 0.257 |
| Chronic kidney disease, n (%) | 43 (32) | 5 (12) | 38 (40) | 0.001 |
| CKD stage, n (%): | 0.489 | |||
| 1 | 0 (0) | 0 (0) | 0 (0) | |
| 2 | 8 (19) | 1 (20) | 7 (18) | |
| 3a | 16 (37) | 1 (20) | 15 (39) | |
| 3b | 14 (33) | 3 (60) | 11 (29) | |
| 4 | 5 (11) | 0 (0) | 5 (13) | |
| Basal creatinine (mg/dL)b | 0.99 (0.81–1.23) | 0.86 (0.71–1.08) | 1.01 (0.88–1.28) | 0.003 |
| eGFR by CKD-EPI (mL/min/1.73m)2,b | 76 (58–92) | 95 (81–106) | 68 (55–84) | <0.001 |
| Ischemic heart disease, n (%) | 34 (25) | 6 (15) | 28 (30) | 0.085 |
| Stroke, n (%) | 15 (11) | 3 (7) | 12 (13) | 0.552 |
| Heart failure, n (%) | 31 (23) | 3 (7) | 28 (30) | 0.006 |
| Peripheral vascular disease, n (%) | 17 (13) | 1 (2) | 16 (17) | 0.022 |
eGFR, estimated glomerular filtration rate; CKD, chronic kidney disease; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; AKI, acute kidney injury.
Of the 134 cases of endocarditis, 90 (67%) occurred on the native valve. The most frequent valve involvement was aortic (46%) followed by mitral (43%). The most common organisms involved were gram-positive cocci (Staphylococcus aureus in 21%, Enterococcus faecalis in 18% and Staphylococcus epidermidis in 13%). In 59 patients (44%) some type of embolic complication was evident (27% multiple embolisms, 44% stroke). In 12 patients (9%) there was persistent bacteremia (Table 2). Surgical intervention was performed in 62 (47%) patients.
Characteristics of infective endocarditis in included patients.
| Variables | All (n=134) | No LRA (n=40) | LRA (n=94) | p |
|---|---|---|---|---|
| Type of valve affected (native), n (%) | 90 (67) | 33 (82) | 57 (61) | 0.016 |
| Valve affected, n (%): | 0.692 | |||
| Mitral | 57 (43) | 17 (42) | 40 (43) | |
| Aortic | 61 (46) | 18 (45) | 43 (46) | |
| Aortic and mitral | 9 (7) | 4 (10) | 5 (5) | |
| Tricuspid | 4 (3) | 1 (3) | 3 (3) | |
| Pulmonary | 3 (2) | 0 (0) | 3 (3) | |
| Bacteremia, n (%) | 113 (84) | 30 (75) | 83 (88) | 0.069 |
| Responsible micro-organism, n (%): | 0.171 | |||
| Staphylococcus aureus | 28 (21) | 5 (12) | 23 (24) | |
| Others | 29 (22) | 10 (25) | 19 (20) | |
| Enterococcus faecalis | 24 (18) | 8 (20) | 16 (17) | |
| Staphylococcus epidermidis | 17 (13) | 2 (5) | 15 (16) | |
| Unidentified | 12 (9) | 7 (17) | 5 (5) | |
| Streptococcus viridans | 9 (7) | 4 (10) | 5 (5) | |
| Streptococcus bovis | 4 (3) | 0 (0) | 4 (4) | |
| Fungal | 3 (2) | 0 (0) | 3 (3) | |
| Streptococcus sanguinis | 2 (1) | 1 (2) | 1 (1) | |
| Escherichia coli | 2 (1) | 1 (2) | 1 (1) | |
| Coxiella | 2 (1) | 1 (2) | 1 (1) | |
| Staphylococcus hominis | 1 (<1) | 1 (2) | 0 (0) | |
| HACEK | 1 (<1) | 0 (0) | 1 (1) | |
| Persistent bacteremia, n (%) | 12 (9) | 2 (5) | 10 (11) | 0.509 |
| Embolic complication n (%) | 59 (44) | 17 (42) | 42 (45) | 0.851 |
| Echocardiographic data n (%): | 0.240 | |||
| Vegetation | 103 (77) | 35 (87) | 68 (72) | |
| Abscess/pseudoaneurysm | 17 (13) | 2 (5) | 15 (16) | |
| Prosthetic dehiscence | 1 (<1) | 0 (0) | 1 (1) | |
| No findings | 13 (10) | 3 (8) | 10 (11) |
HACEK: Hemophilus species, Aggregatibacter actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, Kingella kingae; AKI: acute kidney injury.
Of the patients included, 94 (70%) had AKI, of which 47 [50%] had AKIN-1, 27 [29%] had AKIN-2 and 20 [21%] had AKIN-3. The etiology of AKI was functional in 72 patients (77%), secondary to acute tubular necrosis in 11 (12%) patients, due to tubulointerstitial nephritis in one patient (1%) and due to multiple causes in nine (10%) patients. We only had data from one renal biopsy, which demonstrated tubulointerstitial nephritis as the etiological cause of AKI; in the remaining cases the diagnosis was clinical.
The median reduction of eGFR by CKD-EPI was 40 (range: 16–61)%. Percentage loss of eGFR correlated positively with baseline eGFR (r = −0.226, p=0.009) (Fig. 1). During hospitalization, 56 (42%) patients required admission to the Intensive Care Unit (ICU) and 25 patients (19%) required renal replacement therapy (RRT). RRT was more frequent in patients requiring ICU (p<0.001) (Table 3). Other factors associated with the need for ICU admission were being male (p=0.046), age (p=0.032), peripheral vascular disease (p=0.010), needof surgery (p<0.001), development of AKI (p<0.001), severity of AKI (p<0.001), and etiology of AKI (p<0.001) (Table 3).
Spearman correlation between baseline eGFR and eGFR loss by CKD-EPI (r = −0.226, p=0.009).
eGFR, estimated glomerular filtration rate; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; OR, odds ratio; 95% CI, 95% confidence interval.
Perdida FGe (%): Loss of eGFR (%)
FGe por CKD-EPI (ml/min/1,73m2): eGFR (%) CKD-EPI (ml/min/1,73m2)
Factors associated with the need for admission to the Intensive Care Unit (ICU).
| Variables | Non-ICU | UCI | p |
|---|---|---|---|
| (n=78) | (n=56) | ||
| Sex (male), n (%) | 44 (56) | 41 (73) | 0.046 |
| Age (years)a | 74±16 | 68±12 | 0.032 |
| Arterial hypertension, n (%) | 51 (65) | 38 (68) | 0.765 |
| Diabetes mellitus, n (%) | 15 (19) | 18 (32) | 0.087 |
| Dyslipidemia, n (%) | 35 (45) | 30 (54) | 0.320 |
| Chronic kidney disease, n (%) | 25 (32) | 18 (32) | 0.991 |
| CKD stage, n (%): | 0.833 | ||
| 1 | 0 (0) | 0 (0) | |
| 2 | 5 (20) | 3 (17) | |
| 3a | 10 (40) | 6 (33) | |
| 3b | 8 (32) | 6 (33) | |
| 4 | 2 (8) | 3 (17) | |
| Basal creatinine (mg/dL)b | 0.98 (0.81–1.23) | 1.00 (0.80–1.26) | 0.416 |
| eGFR by CKD-EPI (mL/min/1.73m)2,b | 80 (59–94) | 72 (57–89) | 0.414 |
| Ischemic heart disease, n (%) | 20 (26) | 14 (25) | 0.933 |
| Stroke, n (%) | 8 (10) | 7 (12) | 0.685 |
| Heart failure, n (%) | 15 (19) | 16 (29) | 0.206 |
| Peripheral vascular disease, n (%) | 5 (6) | 12 (21) | 0.010 |
| Bacteremia, n (%) | 66 (85) | 47 (84) | 0.914 |
| Persistent bacteremia, n (%) | 5 (6) | 7 (12) | 0.223 |
| Embolic complication, n (%) | 31 (40) | 28 (50) | 0.238 |
| Echocardiographic data, n (%): | 0.202 | ||
| Vegetation | 60 (77) | 43 (77) | |
| Abscess/pseudoaneurysm | 7 (9) | 10 (18) | |
| Prosthetic dehiscence | 1 (1) | 0 (0) | |
| No findings | 10 (13) | 3 (5) | |
| Surgical intervention, n (%) | 19 (25) | 43 (77) | <0.001 |
| AKI, n (%): | 45 (58) | 49 (87) | <0.001 |
| AKIN, n (%): | <0.001 | ||
| AKIN-1 | 32 (71) | 15 (31) | |
| AKIN-2 | 11 (24) | 16 (33) | |
| AKIN-3 | 2 (4) | 18 (37) | |
| Etiology of AKI, n (%): | 0.001 | ||
| Functional | 41 (93) | 31 (63) | |
| NTA | 2 (5) | 9 (18) | |
| NIIA | 1 (2) | 0 (0) | |
| Multifactorial | 0 (0) | 9 (18) | |
| Need for TRS, n (%) | 2 (3) | 23 (41) | <0.001 |
eGFR, estimated glomerular filtration rate; CKD, chronic kidney disease; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; AKI, acute kidney injury; AKIN, acute kidney injury network; AKI, RRT, renal replacement therapy; acute tubulointerstitial nephritis; AKI, acute tubular necrosis; ARN; AIN: acute tubulointerstitial nephritis.
Factors associated with AKI were age (p=0.03), hypertension (p=0.005), chronic kidney disease (p=0.001), baseline eGFR (p<0.001), baseline creatinine (p=0.003), history of heart failure (p=0.006) and peripheral vascular disease (p=0.022) (Table 1). The only independent predictor of AKI was baseline eGFR (odds ratio (OR) of 0.940, 95% confidence interval [95% CI] 0.906−0.975, p=0.001) in a model adjusted for age and comorbidities (hypertension, CKD, stroke, peripheral vascular disease and heart failure).
Factors associated with mortalityDuring hospitalization, 46 (34%) patients died. Of these 46 patients, 45 (98%) had developed some degree of AKI (p=0.001). Factors associated with mortality were age (p=0.012), chronic kidney disease (p=0.002), baseline eGFR (p<0.001), baseline creatinine (p=0.003), history of ischemic heart disease (p=0.003), heart failure (p=0.002), peripheral vascular disease (p=0.002), eGFR at admission (p<0.001), minimum eGFR at admission (p<0.001), and minimum eGFR during the episode (p<0.001), eGFR loss (p<0.001), AKI severity (p=0.003), need for RRT (p<0.001) and need for ICU admission (p<0.001) (Table 4). Different adjusted logistic regression models were constructed in which the independent predictive capacity of AKI for mortality after endocarditis was demonstrated (Table 5). The severity of AKI was associated with mortality, which was higher as the AKIN index increased (Fig. 2). Sensitivity analysis determined that, adjusted for age, sex and eGFR at admission, eGFR loss and baseline eGFR were independently associated with increased mortality (Table 6). At each follow-up point, we found differences in eGFR between patients who died and those who did not (Fig. 3).
Factors associated with mortality from infective endocarditis.
| Variables | RR (95% CI) | p |
|---|---|---|
| Sex (male) | 1.07 (0.49–2.15) | 0.946 |
| Age (per year) | 1.04 (1.01–1.07) | 0.012 |
| High blood pressure (yes) | 1.24 (0.58–2.67) | 0.577 |
| Diabetes mellitus (yes) | 1.13 (0.49–2.56) | 0.777 |
| Dyslipidemia (yes) | 0.73 (0.36–1.51) | 0.400 |
| Chronic kidney disease (yes) | 3.40 (1.58–7.30) | 0.002 |
| Basal creatinine (per mg/dl) | 5.13 (1.74–15.1) | 0.003 |
| Baseline eGFR by CKD-EPI (per mL/min/1.73m)2 | 0.96 (0.95–0.98) | <0.001 |
| Ischemic heart disease (yes) | 3.42 (1.53–7.68) | 0.003 |
| Stroke (yes) | 1.79 (0.61–5.31) | 0.290 |
| Heart failure (yes) | 3.71 (1.61–8.55) | 0.002 |
| Peripheral vascular disease (yes) | 5.86 (1.92–17.9) | 0.002 |
| AKI(yes) | 35.8 (4.72–271) | 0.001 |
| GFR on admission by CKD-EPI (per mL/min/1.73m)2 | 0.96 (0.94–0.98) | <0.001 |
| Minimum eGFR by CKD-EPI (per mL/min/1.73m)2 | 0.92 (0.89–0.95) | <0.001 |
| Loss of eGFR by CKD-EPI (per 10%) | 1.57 (1.29–1.91) | <0.001 |
| Severity of LRA (due to AKIN category change) | 2.35 (1.35–4.11) | 0.003 |
| Need for TRS (yes) | 12.7 (4.36–37.3) | <0.001 |
| Type of valve concerned (native) | 0.75 (0.36–1.60) | 0.463 |
| Bacteremia (yes) | 1.37 (0.50–3.81) | 0.546 |
| Persistent bacteremia (yes) | 2.05 (0.62–6.76) | 0.238 |
| Embolic complications (yes) | 1.12 (1.01–1.25) | 0.045 |
| Surgical intervention (yes) | 0.76 (0.37–1.56) | 0.458 |
| ICU admission (yes) | 3.85 (1.82–8.16) | <0.001 |
RR (95% CI), relative risk (95% confidence interval); AKI, acute kidney injury; AKIN, acute kidney injury network; eGFR, estimated glomerular filtration rate; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; RRT, renal replacement therapy.
Adjusted logistic regression models to determine the independent predictive power of acute kidney injury (AKI) on infective endocarditis mortality.
| Variables | OR (95% CI) | p |
|---|---|---|
| Model 1 (adjusted for age and sex) | ||
| LRA (yes) | 32 (4–245) | 0.001 |
| Model 2 (adjusted for age, sex and baseline eGFR) | ||
| LRA (yes) | 23 (3–181) | 0.003 |
| Model 3 (adjusted for age, sex and comorbidities)a | ||
| LRA (yes) | 28 (4–228) | 0.002 |
| Model 4 (adjusted for age, sex and endocarditis complications)b | ||
| AKI (yes) | 34 (4–273) | 0.001 |
| Model 5 (adjusted for age, sex and ICU admission) | ||
| AKI (yes) | 20 (3–161) | 0.004 |
AKI: acute kidney injury; OR (95% CI): odds ratio (95% confidence interval); eGFR: estimated glomerular filtration rate; ICU: Intensive Care Unit.
Association between AKIN AKI severity and mortality following an episode of endocarditis.
Basal: Basal, Ingreso: Admission, Minimo: Minimum Vivo: Vivo Exitus: Exitus.
eGFR, estimated glomerular filtration rate; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; OR, odds ratio; 95% CI, 95% confidence interval; AKIN, acute kidney injury network.
Logistic regression adjusted for age, sex and eGFR by CKD-EPI at admission for infective endocarditis mortality.
| Variables | OR (95% CI) | p |
|---|---|---|
| Loss of eGFR from baseline (%) | 1.054 (1.027–1.081) | <0.001 |
| Baseline eGFR by CKD-EPI (per mL/min/m)2 | 0.963 (0.936–0.992) | 0.012 |
eGFR: estimated glomerular filtration rate; CKD-EPI: Chronic Kidney Disease Epidemiology Collaboration; OR (95% CI): odds ratio (95% confidence interval).
Our study evaluates the impact of AKI on the prognosis of infective endocarditis, the results reveal two relevant findings. First, there is a high incidence of AKI among hospitalizations for infective endocarditis (up to 70%), which is consistent with the most pessimistic data published.4 Second, there is a high mortality associated with the development of AKI and it correlates with the severity of AKI (as measured by the AKIN scale and by eGFR loss) that correlates with a worse prognosis. In fact, the need for RRT was associated with a 12-fold increased likelihood of death as compared to those who did not require RRT. This is not surprising since the inherent immunodeficiency of AKI is compounded by the complications of RRT such as the use of central lines, the need for anticoagulants and hemodynamic alterations.16
The development of infective endocarditis is a potentially lethal situation and, as observed in our study, is accompanied by important complications such as the development of bacteremia in 84% of patients and systemic embolisms in 44%, which leads to a high rate of AKI, admission to the ICU and mortality. The development and impact of AKI on the prognosis of endocarditis has been little studied to date. In this context, the most potentl study to date is a registry analyzing more than 7,000 patients diagnosed with endocarditis. Of these, 5.7% required RRT during admission, which had a significant impact on mortality.17 Beyond those patients requiring RRT, our data show that even AKIN-1 is associated with up to 18 times higher mortality, making it necessary to closely monitor all patients to detect as early as possible any degree of renal dysfunction.18 While creatinine is the universally used marker for managing AKI, we are aware of its extensive limitations, including delayed diagnosis and consequently the prognostic impact. To date, very few studies have included markers other than creatinine such as cystatin C or neutrophil gelatinase-associated lipocalin (NGAL), studying their association with the prognosis of endocarditis, but without delving into the early diagnosis of AKI.19,20 Perhaps the selected use of these biomarkers could enhance early diagnosis of AKI and eventually improve prognosis. Some measures would include the use of non-nephrotoxic antibiotics, adjusting medication to renal function, performing tests aimed at a precise etiological diagnosis, such as immunity studies or renal biopsy or optimizing the volume.6,21 In fact, in our sample, only one patient underwent a renal biopsy during the episode. This situation, although consistent with data from the literature and contextualized in the patient's clinical situation, should make healthcare providers think about the need to make a correct diagnosis using a procedure with a low risk/benefit ratio.22
Among the factors associated with AKI, our study shows that cardiovascular and renal comorbidities are the most relevant. The only independent predictor of AKI was baseline eGFR, which in routine practice is easy to determine and could be included as a severity parameter to facilitate the detection of patients at high risk of complications. Currently, very little has been done on prognostic prediction in patients with endocarditis, with only one study evaluating the Sepsis-related Organ Failure Assessment score (SOFA) (which includes diuresis and creatinine), and that study lacked specific modifications for endocarditis.23
During hospitalization endocarditis has a mortality rate of up to 25%.2 Factors classically associated with the development and severity of infective endocarditis include age, development of heart failure and baseline comorbidities.2,24 Our data show that beyond comorbidities, the development of AKI independently predicts mortality. In fact, the very factors related to infection (presence of bacteremia, affected valve, need for surgical intervention) hardly show a relationship with vital prognosis and only the need for admission to the ICU shows a striking association with mortality, which should be understood as a marker of severity of infection and a worse situation at baseline. Therefore, the baseline status of patients, including renal function prior to the episode, together with the evolution of the episode of endocarditis can help to establish the risk of mortality. Some authors have shown how individualization is useful for selecting patients who are candidates for valve surgery. With the recent availability of percutaneous techniques, many frail patients or patients with high comorbidity rates who were previously excluded from surgery can now undergo valve repair or replacement.25,26 Our results suggest that renal function should be used as a prognostic marker and, therefore, as a factor to be included in risk scales.
Our study has limitations. Firstly, its retrospective design limits the availability of some patient data, including urinary parameters that were not requested in many cases. This limitation is mainly explained by the large percentage of patients (80%) who did not develop AKI or had AKIN-1 and who were probably not assessed by a nephrologist and in whom renal function deterioration did not have clinical significance. Second, the sample size is not large, due to the single-center nature of the study. This limitation was partially compensated by the fulfilment of the study objectives, which aimed to demonstrate the impact of AKI on mortality from infective endocarditis. Third, little renal histopathological data is available, probably because AKI in endocarditis is systematically attributed to a functional, toxic or ischemic etiology. Although this should not be interpreted as a general limitation of the study, it is important in some specific cases that require more information about the kidney lesion in order to decide about certain treatments. Finally, 50% of the patients had AKIN-1, which probably meant that a nephrologist was not consulted. The possibility of nephrology being consulted when AKI occurs, even if it is mild, is logistically complicated, but should be understood as a limitation of healthcare systems. In fact, electronic alert systems for AKI detection have proven to be effective in the prognosis of patients hospitalized for any reason, suggesting the benefit of early management by a specialist.27
In conclusion, the development of AKI alongside infective endocarditis has an impact on mortality: the more severe the renal function deterioration, the higher the mortality rate. Renal function monitoring may help in the early detection of the endocarditis patients likeliest to have the worst outcomes.
EthicsThe present study has been approved by the Committee on the Ethics of Research with Medicines (CEim) of the Hospital Universitario de la Princesa (24-03-22, act CEIm 06/22).
FundingThe study has not been funded.
Conflict of interestThe authors declare that they have no conflicts of interest.