CASE REPORT
Woman aged 58 years, with history of depressive syndrome and lumbar canal stenosis. Diagnosed with B27 positive ankylosing spondylitis in 2005 and treated with adalimumab since 2008. Before treatment was started, a positive Mantoux test made it necessary to perform prophylaxis with isoniazid for nine months. Her regular medication included nonsteroidal anti-inflammatory drugs, tramadol, antidepressants and proton pump inhibitors.
During a routine rheumatology review, a significant deterioration in renal function was discovered and she was referred to a nephrologist for assessment. The patient was asymptomatic. The initial physical examination did not reveal oedema, no lateral cervical or retroauricular adenopathy were palpable and cardiopulmonary auscultation was normal.
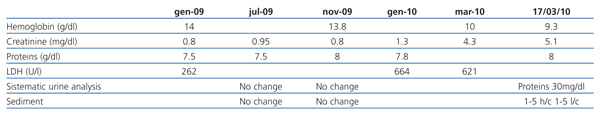
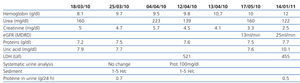
Given the laboratory findings (Table 1), a renal ultrasound was performed in which the kidneys were observed to be 10cm and 12cm, respectively, with good corticomedullary differentiation. There were no data on ureterolithiasis or pyelocaliceal dilation. Hypodense lesions in the spleen suggested possible lymphomatous involvement and the patient was admitted for further studies.
Thoracic-abdominopelvic computed tomography (CT) highlighted the presence of multiple pulmonary nodules (predominantly in the upper lobes in a peribronchovascular pattern) and mediastinal adenopathies. There were no splenic lesions.
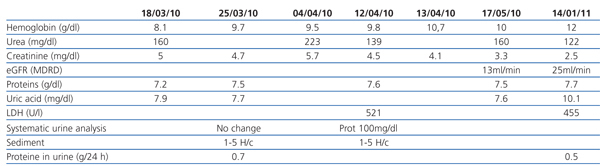
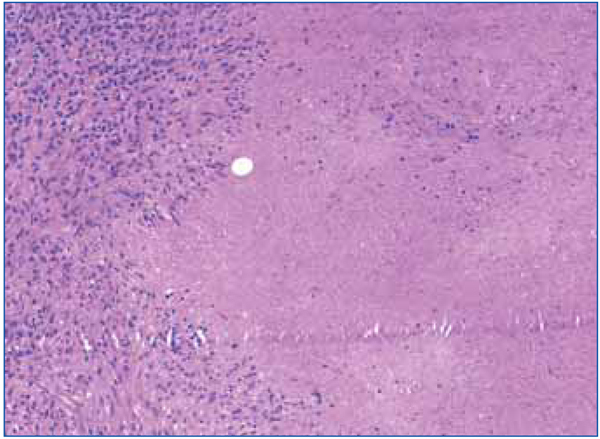
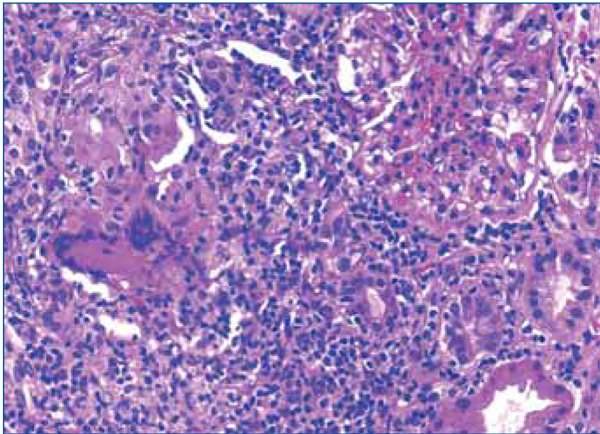
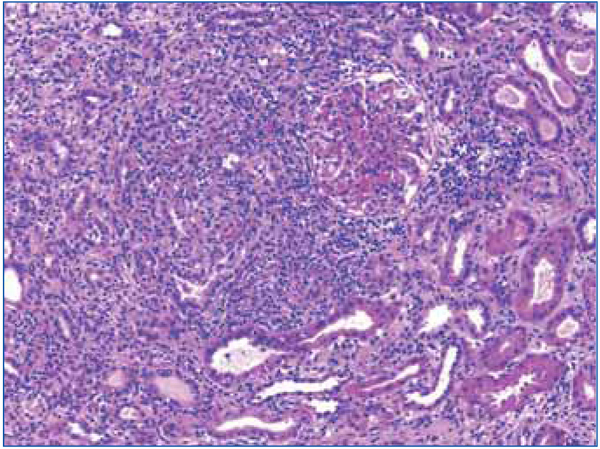
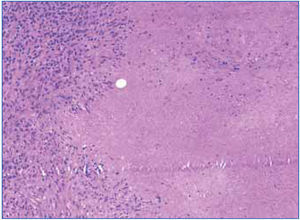
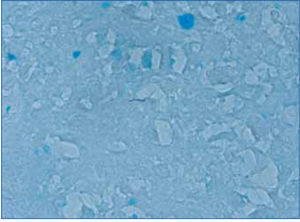
A cervical adenopathy biopsy was performed in which epithelioid granulomatous inflammation was observed with extensive caseous necrosis (Figure 1). A few bacilli were observed in the Ziehl-Nielsen stain (Figure 2).
Given these findings, a fibrobronchoscopy was performed, which did not reveal any macroscopic lesions in the airway. Bronchoalveolar lavage showed a moderate amount of lymphocytes. Bronchial lavage was negative and a transbronchial fine needle aspiration of a mediastinal adenopathy identified granulomas. Ziehl stain was initially reported as negative, but a second observation noted a single acid-alcohol resistant bacillus. After fibrobronchoscopy, a gamma interferon release assay for tuberculosis (QuantiFERON®) was performed, which was positive. Based on these tests, a decision was made to start treatment for tuberculosis.
As part of the nephrology study, antinuclear antibodies (ANA), anticytoplasmic neutrophil antibodies (ANCA), anti-ADN antibodies and anti-glomerular basement membrane antibodies were negative. Viral serology was negative for the human immunodeficiency and hepatitis B and C viruses. The complement was normal. Urine tests initially showed a microalbuminuria/creatininuria index of 261.9mg/g and proteinuria/creatininuria of 1.1 with no nephrotic syndrome. The only information of note in the proteinogram was the monoclonal IgM peak, with a serum level of 305mg/dl, and negative urinary light chains.
During her evolution in hospital, the patient presented sustained hypertension without evidence of fluid overload or other noteworthy symptoms.
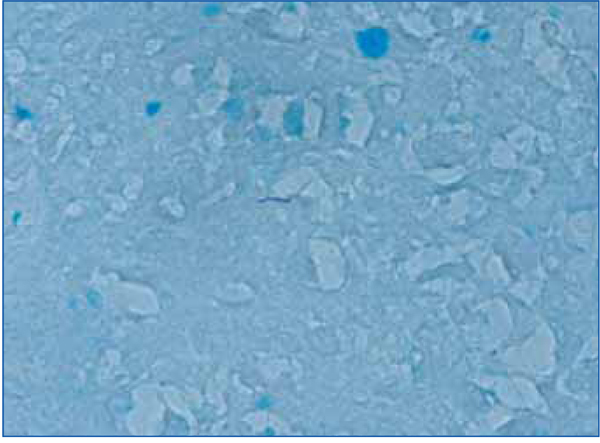
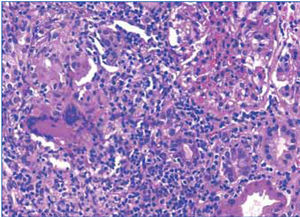
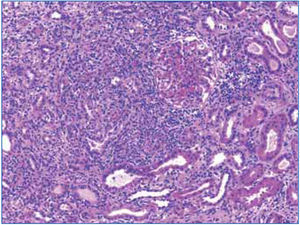
Given the clinical (severe renal failure), radiological (kidneys of normal size and echostructure) and laboratory findings (anaemia, proteinuria and microscopic haematuria), a renal biopsy was performed in which interstitial inflammation at the expense of lymphocytes was detected, accompanied by histiocytes, which formed granulomas at several points (Figure 2 and 3). One of these contained multinucleated Langhans giant cells. Glomeruli were normal. Granular material occupied the tubules and the epithelium was flattened. There were no microorganisms in the PAS or Ziehl-Nielsen stain.
After performing the renal biopsy, the patient was discharged with treatment of prednisone at a dosage of 40mg/day, erythropoietin and complete tuberculosis treatment (rifampicin, isoniazid, ethambutol and pyrazinamide).
The patient progressed slowly but showed continuous improvement in renal function (Table 2). Her anaemia persisted along with the high erythropoietin requirements, hypertension treated with two drugs, and hyperuricaemia, which resolved with allopurinol.
DISCUSSION
We were faced with grade III nonoliguric renal failure as per the AKIN classification (Acute Kidney Injury Network) and loss of RIFLE classification (Risk, Injury, Failure, Loss and End stage renal disease).
1. Based on the clinical picture, initial differential diagnosis was established between the most common renopulmonary syndromes: ANCA-associated systemic vasculitis (Wegener's granulomatosis, Churg-Strauss syndrome and microscopic polyangiitis), Goodpasture's syndrome, systemic lupus erythematosus, sarcoidosis and systemic infections.
2. The following differential diagnosis was established based on the renal biopsy:
a) Acute tubulointerstitial nephritis secondary to drugs related to the dense lymphocytic infiltrate. The patient took NSAIDs from the start, but did not have cutaneous exanthema, fever, eosinophilia or eosinophiluria.
b) Renal sarcoidosis and sarcoidosis-like syndrome, due to the presence of non-caseous granulomas in the biopsy. Although it has been reported in patients treated with adalimumab, it cannot be definitively ruled out since, in our case, a PCR of the Koch’s bacillus DNA was not performed in the renal biopsy, nor were there any acid-alcohol resistant bacilli. In addition, there were no clinical data for other organs that justified a diagnosis of sarcoidosis with parotid, ocular or bilateral parahilar mediastinal adenopathy involvement.1
c) Tuberculosis with granulomatous interstitial involvement (our primary hypothesis). Included in the histological data of the biopsy supporting this hypothesis is the presence of Langhans cell granulomas, although caseous necrosis was not observed. The absence of acid-alcohol resistant bacilli in the renal biopsy and the lack of PCR of the sample prevents us from concluding that granulomatous interstitial nephritis due to tuberculosis was the definite diagnosis.2 However, the clinical picture of pulmonary tuberculosis and caseous necrosis in the cervical adenopathy biopsy almost certainly confirm the diagnosis.
Clinically, patients with this condition have problems characteristic of urinary tract infection, sterile pyuria and renal failure. The presence of tubulointerstitial nephritis is common in renal biopsies.3 The existence of mycobacteria in the kidney can be seen by auramine stain (mycobacteria stains), although its sensitivity is low (32%-43%). PCR for detecting Koch’s bacillus in urine has high sensitivity (from 84% to 95%) and specificity (from 85% to 98%). In contrast, renal biopsy PCR, due to inclusion in paraffin, has low sensitivity and specificity. These tests do not preclude culture in Lowenstein-Jensen medium for evaluating antibiotic sensitivity.4
Tuberculous interstitial nephritis has a poor prognosis. In a review of a follow-up study of 25 patients over 10 years, 17 had an estimated glomerular filtration rate (eGFR) of less than 15ml/min at the time of presentation, and 11 of the patients required renal replacement therapy for the first 12 months of follow-up. In the eight patients with eGFR greater than 15ml/min, renal function stabilisation was observed in the first two years of follow-up after initiating tuberculosis treatment. At two years, they had progressive deterioration related to tubular and glomerular atrophy. Despite these data, there was no significant relationship between the degree of improvement and renal function and the initial proteinuria of each patient.5
CONCLUSIONS
Systemic infections, in particular those caused by mycobacteria and fungi, should be considered in the differential diagnosis of pulmonary and renal involvement in immunocompromised patients. The second most frequent extrapulmonary location for tuberculosis is the genitourinary system. Tuberculosis may involve the kidney as the localised organ or as a component of the haematogenous spread of mycobacteria. We believe that anti-tumour necrosis factor alpha (anti-TNF-α) immunosuppression favoured the reactivation of tuberculosis. An increase in lethal infection rates and the possibility of developing lymphomas and extrapulmonary tuberculosis have been reported among the side effects of adalimumab.6
Granulomatous interstitial nephritis is an infrequent cause of renal failure. It has a non-specific presentation and clinical diagnosis is not easy.7 Nephritis is attributable to the involvement of tubercle bacillus, although sarcoidosis-like syndrome secondary to the use of anti-TNF-α antibodies cannot be ruled out.
Combination therapy using antituberculosis drugs and steroids with a decreasing dosing regimen has shown clinical improvement in patient outcomes.
Despite this positive outcome and given the history in the literature,8 it is not possible to predict the prognosis for patient renal survival in the medium to long term before requiring renal replacement therapy.
QUESTIONS
Dr. Julia Blanco (Madrid). The observation of a single Ziehl positive bacillus in the lymph node biopsy and the appearance of caseous necrosis are sufficiently conclusive with the tuberculous etiology. However, did you consider PCR analysis for tuberculosis bacilli in paraffin material to confirm it beyond doubt?
Answer. PCR analyses of Koch’s bacillus were established as a confirmatory test for the presence of bacillus in the renal biopsy. Despite this, the PCR of samples included in paraffin significantly reduces its sensitivity and specificity. Therefore, in the end, we decided against performing the test.
Dr. Xavier Fulladosa (Barcelona). In this type of tuberculous interstitial nephritis after reactivation in an immunocompromised patient, why did you not consider treating the tuberculosis with only antituberculosis agents without steroids?
Answer. It was not considered due to the significant interstitial inflammatory component and the severe deterioration in renal function. With renal inflammatory involvement, the use of antituberculosis agents as the only treatment seemed to us insufficient at the start. Therefore, we started steroid therapy at 1mg/kg of body weight, which resulted in significant initial improvement, so we maintained a decreasing dose regimen.
Dr. Adoración Martín-Gómez (Almería). About the isoniazid prophylaxis, why was it maintained for only two months instead of the minimum six? My second observation is that the finding of a second negative Mantoux is of little use regarding the intention to treat.
Answer. Looking back on the medical history and confirming it with rheumatology, the patient received a total of nine months of prophylactic treatment. The prophylaxis commonly used in immunosuppressed patients is six to nine months of isoniazid or four months of rifampicin. The Mantoux variation in this clinical case has no importance given the radiological, pathological and clinical findings. Nevertheless, we only wanted to highlight this as a potential confounding factor.
Dr. Ana Alexandra (Madrid). In terms of the sarcoidosis-like management in the differential diagnosis, what were the difficulties in choosing between tuberculosis and sarcoidosis?
Answer. Actually the patient's symptoms were very indicative of tuberculosis; however the non-caseous granulomas in the biopsy and the mediastinal adenopathies may have resulted in a possible diagnostic error. The patient's extrarenal symptoms (she did not present uveitis or parotid involvement) partially provided us with the final diagnosis with microbiological confirmation.
Dr. Manuel Praga (Madrid). It seems that the importance of early treatment in tubulointerstitial nephritis has been established to achieve good results in renal function recovery. Why the almost two month delay in this patient?
Answer. The initial renal function impairment that was observed in January 2010 (Table 1) was attributed to possible functional factors in the context of community-acquired pneumonia, which was treated with broad-spectrum antibiotics. This datum was the main reason for the delay in diagnosis, which favoured significant renal function impairment.
Dr. Miguel Ángel Frutos (Malaga). Was the poor expression of urinary sediment at the time of diagnosis of urinary tuberculosis not surprising in this patient?
Answer. Yes, this patient's sediment was fairly unremarkable. We found it interesting that the patient did not present eosinophiluria, which was justified upon treatment of chronic interstitial nephritis. The absence of leukocyte cylinders also surprised us. Similarly, the quantity of erythrocytes and leukocytes in urine, which are expected with such a significant renal involvement, would be much greater (Table 1).
Dr. Mario Espinosa (Cordoba). What role did paraproteinaemia play in this patient?
Answer. Paraproteinaemia was exclusively serendipitous in this clinical case. She was diagnosed with monoclonal gammopathy of undetermined significance without any renal expression.
Dr. Francisco Rivera (Ciudad Real). When was treatment with adalimumab suspended? How much time elapsed between the suspension of adalimumab and the renal biopsy?
Answer. Treatment with adalimumab was suspended once renal function impairment was observed. The time elapsed between the last dose of adalimumab (Humira 40mg) received and the renal biopsy was 24 days.
Acknowledgements
This case was selected in the IV Reunión del Grupo de Enfermedades Glomerulares (IV Meeting of the Glomerular Diseases Group) of the Sociedad Española de Nefrología (Spanish Society of Nephrology, S.E.N.) (GLOSEN) for publication in Nefrología (Nephrology) (Madrid, March 31 to April 2, 2011), thanks to the special sponsorship of Novartis.
Table 1. Evolution of renal function prior to hospital admission
Table 2. Evolution of renal function during hospitalisation and at consultation
Figure 1. Extensive caseous necrosis foci in the right supraclavicular lymph node biopsy
Figure 2. Detection of a bacillus in the Ziehl-Nielsen stain of the lymph node biopsy
Figure 3. Interstitial lymphocytic infiltrate and epithelioid granuloma in the renal biopsy
Figure 4. Detail of the interstitial infiltrate