Pruritus associated with chronic kidney disease is defined as the sensation of itching, in people with chronic kidney disease, in a one area or all over the body that causes the need to scratch, after having ruled out other dermatological or systemic causes. It is an old and known problem whose prevalence has been able to decrease with the improvement of dialytic techniques but which still persists and is underdiagnosed.
ObjectivesThe objective of this study was to analyse the current perception of nephrologists about this problem that influences the quality of life of people with chronic kidney disease through a survey.
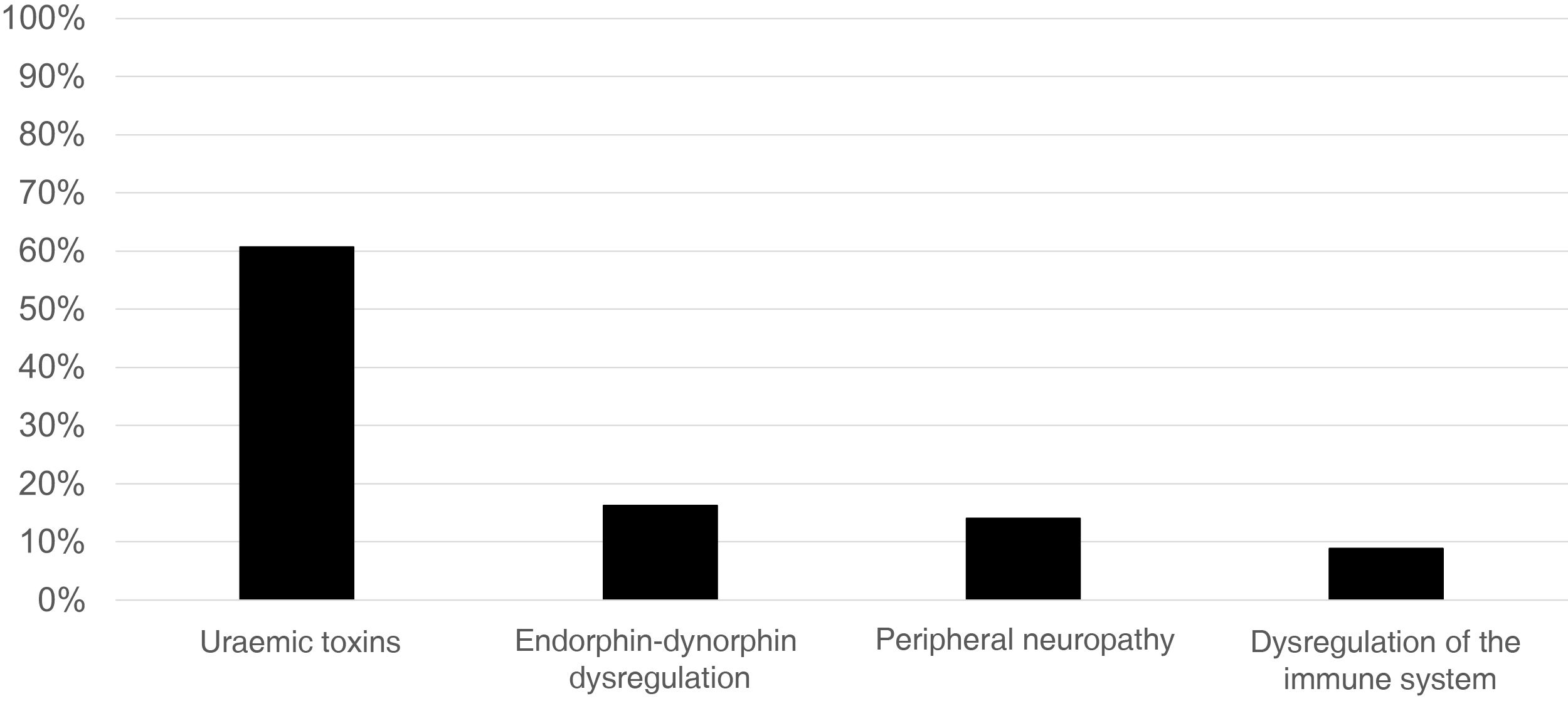
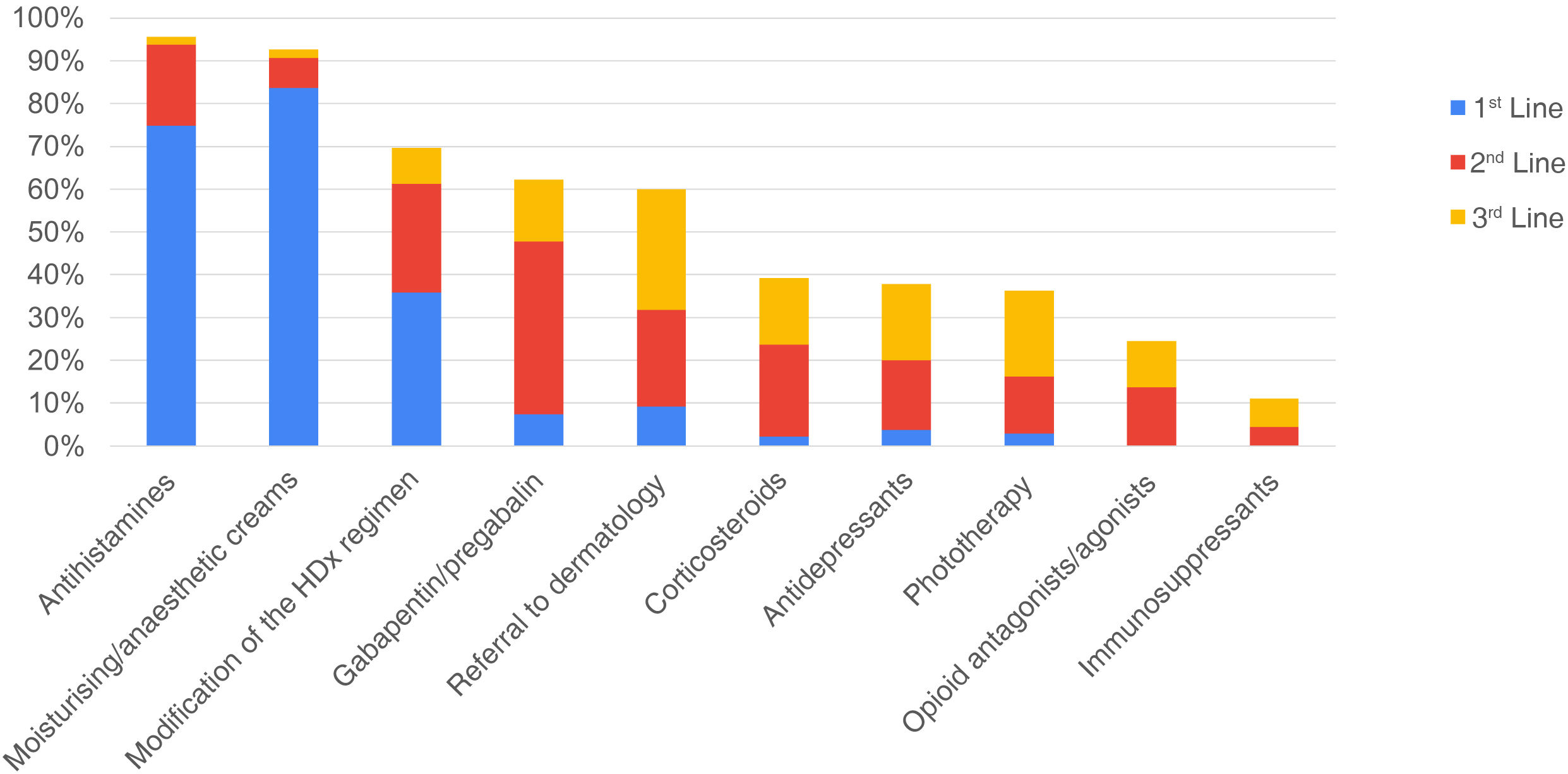
Results135 nephrologists, most of them engaged in haemodialysis, participated. 86% considered that pruritus associated with chronic kidney disease is still a problem today that affects the quality of life. Most nephrologists believe that the main pathophysiological cause is uremic toxins (60%) and only 16% believe that it is due to the dysregulation of the opioid system/endorphins-dynorphins. Only 16% comment that the prevalence of pruritus in their centre is greater than 20%. 40% believe that the diagnosis is made because it is manifested by the patient and only 27% because it is asked by the doctor. Moreover, it is not usual to use scales to measure it or the codification in the medical records. The main treatment used is antihistamines (96%), followed by moisturizers/anaesthetics (93%) and modification of the dialysis regimen (70%).
ConclusionsPruritus associated with chronic kidney disease is still a current problem, it is underdiagnosed, not codified and with a lack of indicated, effective and safe treatments. Nephrologists do not know its real prevalence and the different pathophysiological mechanisms involved in its development. Many therapeutic options are used with very variable results, ignoring their efficacy and applicability at the present time. The new emerging kappa-opioid-receptor agonist agents offer us an opportunity to reevaluate this age-old problem and improve the quality of life for our patients with chronic kidney disease.
El prurito asociado a enfermedad renal crónica se define como la sensación desagradable que provoca la necesidad de rascarse en una parte del cuerpo o en todo en personas con enfermedad renal crónica, tras haberse descartado otras causas dermatológicas o sistémicas. Es un problema antiguo y conocido cuya prevalencia ha podido disminuir con la mejoría de la eficacia dialítica pero que todavía persiste y está infradiagnosticado.
ObjetivosEl objetivo de este estudio fue analizar la percepción y práctica actual de los nefrólogos sobre este problema que impacta en la calidad de vida de las personas con enfermedad renal crónica a través de una encuesta anónima.
ResultadosParticiparon 135 nefrólogos, la mayoría dedicados a hemodiálisis. Un 86% consideró que el prurito asociado a enfermedad renal crónica sigue siendo un problema en la actualidad que afecta a la calidad de vida. La mayoría de los nefrólogos opinan que la principal causa fisiopatológica son las toxinas urémicas (60%) y solo un 16% cree que se debe a la desregulación del sistema opioide/endorfinas-dinorfinas. Únicamente un 16% comenta que la prevalencia de prurito en su centro es mayor del 20%. Un 40% cree que el diagnóstico se realiza porque lo manifiesta el paciente y solo un 27% porque lo pregunta el facultativo. Además, no es habitual usar escalas ni codificarlo en la historia clínica. El tratamiento más común son los antihistamínicos (96%), seguido de las cremas hidratantes/anestésicas (93%) y la modificación de la pauta de diálisis (70%).
ConclusionesEl prurito asociado a enfermedad renal crónica sigue siendo un problema actual, está infradiagnosticado, no codificado y con falta de tratamientos indicados, eficaces y seguros. Los nefrólogos desconocemos su prevalencia real y los diferentes mecanismos fisiopatológicos implicados en su desarrollo. Se utilizan muchas opciones terapéuticas con resultados muy variables, desconociendo su eficacia y su aplicabilidad en el momento actual. Los nuevos agentes emergentes agonistas de los receptores opioides kappa nos ofrecen una oportunidad para reevaluar este antiguo problema y mejorar la calidad de vida de nuestros pacientes con enfermedad renal crónica.
Chronic pruritus can be defined as an unpleasant sensation that produces the urge to scratch, which affects part or all of the body and is present for more than six weeks.1 There are four important causes of pruritus: dermatologic, systemic, neuropathic, and psychogenic. To suspect a dermatologic cause, primary skin lesions must be evident. The other causes do not produce primary skin lesions, but there may be secondary skin lesions such as scratch lesions and prurigo nodularis.2 We should consider chronic kidney disease-associated pruritus (CKD-aP) if a patient has pruritus due to a systemic cause directly related to chronic kidney disease (CKD) after having ruled out the other three aetiologies.
It is a long-standing and well-known problem whose prevalence may have decreased with the improvement in dialysis efficacy, but which still persists and is underdiagnosed.3,4 CKD-aP significantly affects the quality of life of these patients, causing sleep disorders, anxiety and depression.5,6 It has also been associated with an increase in mortality and healthcare expenditure.7 Despite its high prevalence (60% in Spain if we include mild-severe pruritus, and 36% if we consider moderate-severe according to the DOPPS (Dialysis Outcomes and Practice Patterns Study) phase 5 study, from 2012 to 2015)8 and its impact on quality of life, understanding its multifactorial pathophysiological mechanism can be complex.9,10 Regarding its pathophysiology, multiple possible causes combine: dysregulation of the immune system, abnormalities associated with uraemia (phosphate, elevated iPTH, insufficient dialysis…), peripheral neuropathy, and the cause that has become most relevant in recent years: dysregulation of the opioid system.11–14
The objective of this study was to analyse the perception and current practice of nephrologists regarding this long-standing unresolved problem, which impacts the quality of life of our patients.
Material and methodsWe conducted an anonymous survey in April 2021 with 14 multiple-choice questions that included sociodemographic data, work habits, and general aspects related to CKD-aP diagnosis, approach, pathophysiological mechanisms, and the most commonly used treatments by Spanish nephrologists. The survey was conducted through the Spanish Society of Nephrology’s (Sociedad Española de Nefrología; SEN) website (Appendix B Annex 1). Any nephrologist who was a member of the SEN could participate.
ResultsParticipant characteristicsOne hundred thirty-five nephrologists (47 men, 87 women) with a mean age of 46.5±10 years participated in this survey. Of these, 109 (81%) worked in hospitals, 15 (11%) in dialysis clinics, and 11 (8%) in both. Regarding their sub-specialties, 97 (72%) specialised in haemodialysis, 36 (27%) in peritoneal dialysis, 15 (11%) in CKD not on dialysis, and 16 (12%) in transplantation. Seventy-nine nephrologists (59%) had multidisciplinary responsibility and 56 (42%) had responsibilities on one discipline.
Impact on the patient, causes and diagnosisEighty-six percent of participants believed that CKD-aP continues to be a problem today, and the vast majority (98%) were convinced that it affects the quality of life of patients.
Regarding the main pathophysiological cause involved, 82 nephrologists (61%) responded uraemic toxins, 22 (16%) dysregulation of the opioid/endorphin-dynorphin system, 19 (14%) peripheral neuropathy, and 12 (9%) immune system dysregulation (Fig. 1).
Regarding diagnosis, 84% of the participants (114 nephrologists) believe that it is underdiagnosed. In total, 57 participants (42%) responded that in their centres, the rate of patients with diagnosed pruritus is 0%–10%, 56 participants (42%) mentioned a diagnosis rate of 10%–20%, while 18 participants (13 %) mentioned a rate of 20%–40% and only four participants (3%) a rate of 40%–60%.
The diagnosis is made because it is reported by the patient in 54 (40%) of the responses, because it is asked about by the physician in 36 (27%) of cases, or by both means, patient and physician, in 48 cases (36%). Only five (4%) nephrologists indicated that they used some kind of scale or questionnaire to diagnose the patient. Finally, only 8% of the participants (11 nephrologists) coded it as a diagnosis or health problem in the medical history.
TreatmentIn the survey, it was asked if each of the following options were used in the first line, second line and/or third line of treatment, or if they were not used at all.
Fig. 2 shows the results obtained about the treatment of CKD-aP, described below:
Antihistamines: this is the most widely used therapeutic option. One hundred and twenty-nine (96%) nephrologists reported using antihistamines as a treatment for patients with CKD-aP. A hundred nephrologists (74%) use them only as first line, 25 (19%) as second line, two (1%) as third line and again in two cases their use was reported as first and second or third line (1%).
Moisturising/anaesthetic creams: this is the second most commonly used option by 125 (93%) of the nephrologists. One hundred and twelve nephrologists (82%) use them only as first line, nine (7%) as second line, two as third line (1%) and also in two cases as first and second or third line (1%).
Modification of the dialysis regimen: this therapeutic option is the third most commonly used. Ninety-four (70%) modify the dialysis regimen as part of their therapeutic arsenal for CKD-aP. Forty-eight (36%) do so as first line treatment, while 34 (25%) and 11 (8%) consider it for second and third line options, respectively. One nephrologist reports using it as a first, second or third line option, depending on the case.
Gabapentin/pregabalin: is used by 84 (62%) nephrologists, 10 (7%) as first line, 54 (40%) as second line and 19 as third line (14%). One nephrologist responded that he/she uses it in both second and third line.
Referral to dermatology: 81 (60%) nephrologists tend to refer patients with CKD-aP to a dermatologist. Twelve (9%) refer their patient to dermatology as the first line of treatment, 30 (22%) consider it a second line option, and the majority, 37 (27%) nephrologists, consider it a third line option. In two cases it is considered first and third line (one nephrologist) or second or third line (one nephrologist).
Corticosteroids: 53 (39%) nephrologists reported using these as a treatment for patients with CKD-aP, only three (2%) used them as first line, 29 (21%) as second line and 21 as third line (16%).
Antidepressants: 51 (38%) nephrologists use these in patients with CKD-aP, five (4%) as first line, 22 (16%) as second line and 24 (18%) as third line.
Phototherapy: is used by 49 (36%) nephrologists, four (3%) as first line, 18 (13%) as second line and 27 (20%) as third line.
Opioid receptor antagonists/agonists: 33 (24%) nephrologists use these, 18 (13%) as second line and 14 as third line (10%). One nephrologist reported using them in both second and third line, and none of the participants used them in first line.
Immunosuppressants: 15 (11%) nephrologists use these, six (4%) as second line and nine (7%) as third line. No participant reported using them as first line.
In summary, of the treatments used as the first line, the most common are moisturising/anaesthetic creams, antihistamines, or modification of the dialysis schedule, reported in this line by 114 (84%), 102 (75%) and 49 (36%) of the nephrologists respectively.
Of the treatments used as second line, the most common is the use of gabapentin/pregabalin (55 nephrologists, 41%) followed by modification of the dialysis regimen (35 nephrologists, 26%) and referral to dermatology (31 nephrologists, 23 %).
Of the treatments considered in the third line, the most common would be referral to dermatology (38 nephrologists, 28%) followed by phototherapy (27 nephrologists, 20%) and antidepressants (24 nephrologists, 18%).
Despite this arsenal of treatments, 123 (91%) nephrologists responded that pruritus is a problem that is yet to be solved. Despite the use of different therapeutic options, since there are currently no other additional therapeutic options, nephrologists are not satisfied with the results due to their low efficacy (107 nephrologists, 79%), followed by low adherence (22 nephrologists, 16%) and undesirable side effects (22 nephrologists, 16%).
DiscussionCKD-aP is a long-standing, unresolved problem that affects patients with advanced CKD. Beyond its direct impact on quality of life, CKD-aP is an independent predictor of mortality. In the DOPPS, a higher rate of all-cause mortality was found in patients with severe pruritus compared with those without pruritus (HR: 1.24), a higher rate of cardiovascular disease-related mortality (HR: 1.29) and of death related to infection (HR 1.44). Other studies also link CKD-aP and cardiovascular mortality.15,16 In all studies, mortality was independent of age, comorbidities, dialysis dose, and vascular access.
Various circumstances exist that have caused CKD-aP to be partially forgotten by the nephrology community in recent years. In the first place, the improvement in the technique and efficacy of dialysis has undoubtedly decreased the prevalence of this symptom, although it is still high. Secondly, there is still a lack of knowledge on the part of nephrologists about the pathophysiological factors involved in the appearance of pruritus. Finally, the lack of specific and adequate treatment has led to nephrologists to have a passive attitude towards this pathology and not being included among the medical history questions, and so the nephrologist's perception of the prevalence of this symptomatology is lower.
It is curious, however, that, despite this perception, this survey shows that nephrologists think that pruritus is an important problem that affects the patient's quality of life, that it is currently not solved and effective therapeutic options are lacking. It is evident that in general there is lack of knowledge about the pathophysiological mechanisms involved, and there is also and the lack of coding and diagnosis of pruritus and without available clinical tools.17
Perception of CKD-aP by the patient and nephrologistCKD-aP is a common symptom in patients with CKD, its prevalence is highly variable depending on the reports, ranging from 20% to as high as 90%.18,19 Serial analyses by the DOPPS performed on dialysis patients in 12 countries reveal a decrease in the prevalence of pruritus (moderate-severe) from 45% in the early phases of the study to 28% in the last.6 In a more recent publication of this same study, it was shown that the prevalence of moderate-severe CKD-aP in Spain is one in three patients (36%) and if patients with mild pruritus are included, it would be almost 70%.8 The nephrologists who participated in our survey think that CKD-aP is a much less prevalent problem than the figures presented in the published articles, only 16% believe that the prevalence is greater than 20%. On many occasions, renal patients are unaware that pruritus is a symptom associated with their disease, so they do not even mention it to the nephrologist. This issue, along with the absence of an effective treatment, has meant that this long-standing problem has been forgotten, and that we do not truly know its current prevalence and the impact on quality of life.
Scales and methods of identificationOnly 6% of the nephrologists who responded to this survey use scales to measure the intensity of pruritus, and most of them do not have it coded in the electronic record, commenting that the diagnosis is made due to the patient's manifestation. Consequently, if the patient does not tell them about pruritus, they do not make diagnose it. In fact, it is possible that many of the patients tell their dermatologist or other specialists that they have itching, rather than the nephrologist. DOPPS 4–6 identifies a profile of patients with a higher risk of pruritus: advanced age, greater comorbidity and central venous catheter as vascular access. Patients with comorbidities such as diabetes mellitus, lung disease, smoking, hypertension, high body mass index, leukocytosis and lower haemoglobin and albumin have a higher incidence of pruritus. Identifying this at-risk patient profile may facilitate the performance of pruritus measurement scales.20 The evaluation of the intensity of pruritus is complex as it is a fairly subjective symptom, and the most widely used tool to evaluate it is the itch visual analogue scale (itch severity scale) (ISS).21 Other scales evaluate, in addition to intensity, the emotional, social, work or quality of life impact, such as the modified Pauli-Magnus scale,22 the 5-D itching scale or the Skindex-10.23 However, the coding of this symptom and the assessment of its intensity are not included in the clinical history of the ACKD-dialysis patient. Although in the ICD-10 (10th revision of the International Classification of Diseases and Disorders related to Mental Health) there is no specific coding, a classification of pruritus by body area or non-specific pruritus can be found that could be considered for the coding of CKD-aP.
Physiopathological mechanisms involved in CKD-aPThe pathophysiology of CKD-aP has been described as multifactorial and caused by toxin deposition, dysregulation of the opioid system, immune system dysfunction, and peripheral neuropathy.17 Most of the nephrologists who participated in the survey still believe that the main mechanism involved in the pathophysiology is uraemic toxins, but some believe that it is dysregulation of the opioid system (16%), or peripheral neuropathy (14%), while a few (9%) attribute it to dysregulation of the immune system. Historically, hyperphosphataemia has been implicated as a cause of pruritus. However, studies in dialysis patients have not found a relationship between pruritus and bone metabolism parameters such as calcium, PTH, and phosphorus.5 In addition, it is possible that we currently do not have patients with persistent severe hyperphosphataemia as we did two decades ago thanks to the new treatments, and therefore it has lost prominence as a cause of pruritus.
Microinflammation, both at the cutaneous and systemic levels, has been proposed in recent years as one of the main factors responsible for CKD-aP. At the systemic level, various observational studies have demonstrated that dialysis patients with pruritus have a significantly higher proportion of various inflammatory markers, including Th1 cells, C-reactive protein, IL-6 and IL-2 levels, as compared to patients without pruritus.24 Other inflammatory markers such as leukocytosis, elevated ferritin, or decreased albumin have also been associated with the appearance of pruritus.25 Recently, it has been postulated that pruritus is associated with elevated levels of prostaglandin E2 and treatment with omega-3 acids could improve it.26
At present, the dysregulation of the opioid system is perhaps the most relevant hypothesis. CKD is hypothesised to involve an imbalance between mu (μ) and kappa (κ) opioid receptors, that are antagonistic to each other, with an imbalance in favour of the μ-receptors. Therefore, pruritus is increased by μ receptor activation or blocking of the κ receptor and decreases by κ receptor activation or blocking of the μ receptor. Pruritus is a common adverse effect after administration of μ agonists, and could be mediated by modulation of serotonergic transmission and activation of the dorsal horn and itch centre in the central nervous system.27
CKD-aP and quality of lifeAlmost all the nephrologists who participated in the survey agree that CKD-aP significantly affects the quality of life of our patients. In fact, it affects the quality of sleep, increasing depression and, in turn, implying higher dialysis abandonment rates and unemployment rates.28 In addition, bacteraemia and sepsis are more common in patients with moderate-severe pruritus than in patients without pruritus.5 All of this results in an increased risk of hospitalisation and death.
CKD-aP treatmentIt has been reported that 50% of CKD-aP cases are treated by nephrologists, 24% by dermatologists, and 19% by primary care physicians.4 As there are many factors involved in the pathophysiology of CKD-aP, and these factors vary significantly between patients, there is no universal treatment that can be applied to all of them. Furthermore, in many cases CKD-aP does not respond to any of the available treatments. All these circumstances are reflected in the variability of treatments employed by the nephrologists who participated in the survey, as shown in Fig. 2.
Antihistamines are the most widely used therapeutic option, mainly as the first line of treatment, by 96% of nephrologists according to the survey. Histamine release can be inhibited by two methods: using histamine receptor antagonists such as hydroxyzine or fexofenadine, or by inhibiting histamine release with the use of mast cell stabilisers such as sodium cromoglicate or montelukast.9 However, different studies show that the use of histamine receptor antagonists is not effective in reducing itching.12 Mast cell stabilisers have mixed results, some such as zinc sulphate, montelukast or cromoglicate show positive results; others such as nicotinamide have not achieved positive effects.1,2 Therefore, it is striking that so many nephrologists consider antihistamines, which do not have an indication for pruritus, as first line treatment. It should be remembered that CKD-aP does not manifest with hives, typical of urticaria, and it is possible that the only effect antihistamines provide is sedation, which on some occasions could promote sleep, but for some patients is an annoying side effect.
Moisturising and anaesthetic creams are another of the most often used treatments (93%, also mostly first line) to reduce itching. Although it is clear that the treatment of xerosis must be a priority to prevent itching, there are no clinical trials on which is the best cream for dialysis patients and there are small studies in which the treatment of dry skin improves mild itching.29,30
Regarding topical treatments that act through C fibres, in a few small studies capsaicin has been shown to be able to locally decrease substance P release in the skin, but in a systematic review the results were not convincing regarding its utility in CKD-aP.31 Pramoxine is a topical local anaesthetic that reduced the intensity of pruritus compared with placebo in a small randomised double-blind study.32 Corticosteroids were used by 39% of the surveyed nephrologists. Topical corticosteroids are widely used for dermatological lesions associated with pruritus, but they have not shown any efficacy in CKD-aP.12
Modifying the dialysis regimen to increase efficacy is another of the most often used therapeutic options in almost 70% of those surveyed, being used in the first line by 36% of nephrologists. KT/V has been inversely associated with CKD-aP, and greater dialysis efficacy improves pruritus intensity in haemodialysis patients.33 In the DOPPS 1 study there were differences observed in the prevalence of pruritus according to the Kt/V, but not in the DOPPS 24. However, there are refractory cases, in which there is no relationship between dialysis efficacy and the degree of CKD-aP, and despite the clear improvement in dialysis efficacy with online haemodiafiltration or expanded dialysis, CKD-aP continues to exist. Polymethylmethacrylate filters have shown one to two point decreases on the visual analogue scale of pruritus. They have adsorptive capacity for middle-sized and high molecular weight particles34 and decreased TN, although in one study polymethylmethacrylate dialysers demonstrated reduction of pruritus independently of concentrations of TNF-α.35
Nerve transmission through C fibres is blocked by drugs such as gabapentin, pregabalin, capsaicin, and pramoxine. These drugs act by inhibiting the release of neurotransmitters from presynaptic nerve terminals, modulating itching. They were used by 62% of the participating nephrologists, mainly as a second (40%) and third (14%) line option (used off-label). In a systematic review that included seven studies with gabapentin, it was shown in six of the seven studies that it was able to reduce the intensity of pruritus. However, there are no systematic studies in patients older than 65 years, the typical profile of dialysis patients, nor are there long-term studies. With this type of drug, care must always be taken with side effects (neurological symptoms, increased risk of falls and fractures), and treatment started at low doses that can be increased according to tolerance.36 Gabapentin-intolerant patients can be treated with pregabalin, which is superior in pharmacokinetics and pharmacodynamics.37
Phototherapy has been a widely used technique since the 1970s for the treatment of intractable CKD-aP. In published studies, Ultraviolet B radiation has been shown to be effective in the majority of patients treated. The main problem is the duration of treatment because the disappearance of pruritus is associated with long-term treatments, even more than two years, and recurrences after discontinuation of therapy are very common, apart from the increased time of dialysis.38 UVA light has not shown positive results in the treatment of CKD-aP.39 Phototherapy after referral to the dermatologist continues to be a therapeutic option chosen in the second line by 13% of nephrologists and in the third line by 20%. However, it is worth mentioning that its prolonged use could foster the appearance of skin cancer.26 In addition, not all hospitals have this technique and it requires travel and patient time, an issue that already affects haemodialysis patients.
Antidepressants are chosen by 38% of nephrologists, the majority in second or third line of treatment. Mirtazapine is a serotonergic antagonist that also has antihistamine action. In a clinical trial, 77 patients initially treated with gabapentin and subsequently with mirtazapine were included, with a reduction in the intensity of pruritus.40 Sertraline is used to reduce pruritus of cholestatic origin, and its efficacy has been demonstrated in uraemic pruritus at a dose of 50mg/day.41
Opioid antagonists/agonists are only used by 13% of nephrologists in the second line and 10% in the third line (Fig. 2). While κ receptor agonists have an antipruritic effect, μ receptor agonists can increase it and vice versa. Taking into account that several of the new κ agonists which we will discuss later are not yet available at the present time in Spain, we assume that 24% of the nephrologists who use opioid agonists/antagonists in the second and third line were referring to naltrexone, which is a μreceptor antagonist. However, the results obtained with this drug are inconsistent and in general it is not recommended due to its potential side effects,42 which constitutes a problem in those patients with chronic pain who require opioids.
Difelikefalin is a specific and highly selective agonist of peripheral κ opioid receptors located in peripheral sensory neurons (suppressing the pain signal and regulating the response of C fibres to pruritogens) and immune cells (with the capacity to reduce the secretion of proinflammatory cytokines), both implicated in the pathophysiology of CKD-aP.43 In a phase three clinical trial, haemodialysis patients with CKD-aP showed significant improvement in symptoms and quality of life.44 Fifty-two per cent of patients treated with difelikefalin reduced pruritus by at least three points on the itch visual analogue scale, a clinically significant change, while only 31% in the placebo arm achieved it. Some side effects such as diarrhoea, dizziness and vomiting were somewhat more common in patients receiving difelikefalin than in those receiving placebo and they decreased with time. Furthermore, they were not accompanied by euphoria, dysphoria, or hallucinations. Upon discontinuation, there were no cases of physical dependence on opioids. In August 2021 it received FDA approval for use in CKD-aP, but it is not yet available in Europe.
Nalfurafine is a peripheral κ receptor agonist, but it also has effects at the central level. It has been shown that it can reduce itching compared to placebo in a randomised clinical trial.45 Its effect on CKD-aP in randomised trials was less than that of gabapentin, and its most common side effect is insomnia. It is currently indicated in refractory CKD-aP in haemodialysis patients in Japan,46 however, the European phase three study did not demonstrate a significant difference versus placebo in the primary endpoint.47
Nalbuphine, a μ opioid receptor antagonist and a κ opioid receptor agonist, has improved pruritus in haemodialysis patients with no difference in serious adverse events between groups, although we do not have long-term data.48
Topical creams containing cannabinoids have been used as a treatment for CKD-aP in the USA and Canada, showing potential benefits. The mechanism of action of cannabinoids to treat pruritus seems to be their ability to neutralize inflammation and pain. Cannabidiol and tetrahydrocannabinol bind to ionotropic transient receptor potential (TRP) ion channels (TRPV1−4, TRPA1 and TRPM8), which have been shown to play a role in the complex cutaneous intercellular communication network between epidermal keratinocytes, immune cells and sensory nerves, leading to the itching sensation. Although the possibility of antagonising or desensitising these TRP channels is promising, it is not yet possible to draw conclusions.49
Clinical trials with monoclonal antibodies are beginning to be conducted, for example, with nevolizumab,50 an anti-IL-31 (inflammatory cytokine) antibody, but without satisfactory results for the time being.
This study has some limitations, such as the possible participation bias in the survey, limited for the most part to nephrologists working in the hospital setting, so the results may not be able to be extrapolated to patients included in other modalities of renal replacement therapy and the participation of nephrologists, who are probably more involved in the issue of pruritus. However, we consider that it is the first survey carried out at a national level offering a current and real vision of a forgotten and frequent problem in our patients, as pruritus is.
In conclusion, CKD-aP continues to be a current problem; it is underestimated, underdiagnosed, and not coded as a diagnosis or health problem. There is a lack of indicated, effective, and safe treatments. A better understanding of its pathophysiology and an improvement in therapeutic strategy is required. Although no treatment indication is available in Spain for CKD-aP, several treatments have been recently studied with this indication for specific CKD-aP population, with promising results. It is possible that the advent of new effective treatments will increase the interest of the nephrology community in CKD-aP.
Finally, the SEN has recently launched a new initiative called La Semana del Prurito [Pruritus Week] that will assist us in increasing knowledge about the prevalence of pruritus in Spain and indications about how it can affect the quality of life of patients with CKD-aP.
FundingThis study received no specific funding from public, private or non-profit organisations.
Conflicts of interestM.G., J.B., E.S. and P.M. have received conference and consulting fees from VIFOR PHARMA. N.A. has participated in training sessions financed by VIFOR PHARMA. The other authors have no conflicts of interest.