A recent prospective study of thyroid functions among 35 patients with AKI found that 80% of them had thyroid dysfunction. The presence of thyroid dysfunction was not associated with prognostic implications among these patients.1 We attempted to prospectively assess thyroid functions at the time of diagnosis of AKI in a larger cohort and try to assess if initial thyroid dysfunction had any prognostic implications on outcomes.
Adult patients admitted with renal injury or those who developed AKI during hospitalization were prospectively recruited for this observational study after informed consent for over a period of one year. The study was approved by the Institutional Research and Ethics committee of Christian Medical College and Hospital, Ludhiana. The diagnosis of AKI was made as per AKIN working group.2 Pregnant women, patients with pre-existing thyroid disease including those on thyroxine supplements or anti-thyroid drugs, patients who received iodine contrast agents prior to recognition with AKI and patients on drugs which interfere with thyroid function were excluded.
Baseline clinical information was collected from the patient and from the charts. The type of AKI-pre-renal, renal, post renal-was then noted. Serum sample was taken for testing free T3(FT3), free T4(FT4) and TSH levels which were determined using the electrochemiluminescence immunoassay on Cobas e411/601 immunoassay analyzer. All recruited patients were first classified as having normal thyroid functions (euthyroid) or having thyroid dysfunction. Patients with thyroid dysfunction were classified into six different types; primary hyperthyroidism, subclinical hyperthyroidism, primary hypothyroidism, subclinical hypothyroidism, non-thyroidal Illness and central hypothyroidism. After baseline investigations, the patients were followed up till discharge from the hospital or in-hospital death.
One hundred and forty-seven patients with a mean age of 57.8±16.8 (range 20–95) years were consented. There were 93 males (63.27%) males and 54 females (36.73%). 49 patients (33.33%) were with stage 1 AKI, 8 patients (5.44%) with stage 2 AKI, 90 patients (61.22%) with stage 3 AKI as per AKIN classification.6 Of 147 enrolled patients, pre-renal causes of AKI were seen in 35(25.80%) patients, renal causes in 13(8.84%) patients, a combination of pre-renal and renal causes in 98(66.67%) patients and combination of post-renal and renal causes in 1(0.68%) patient.
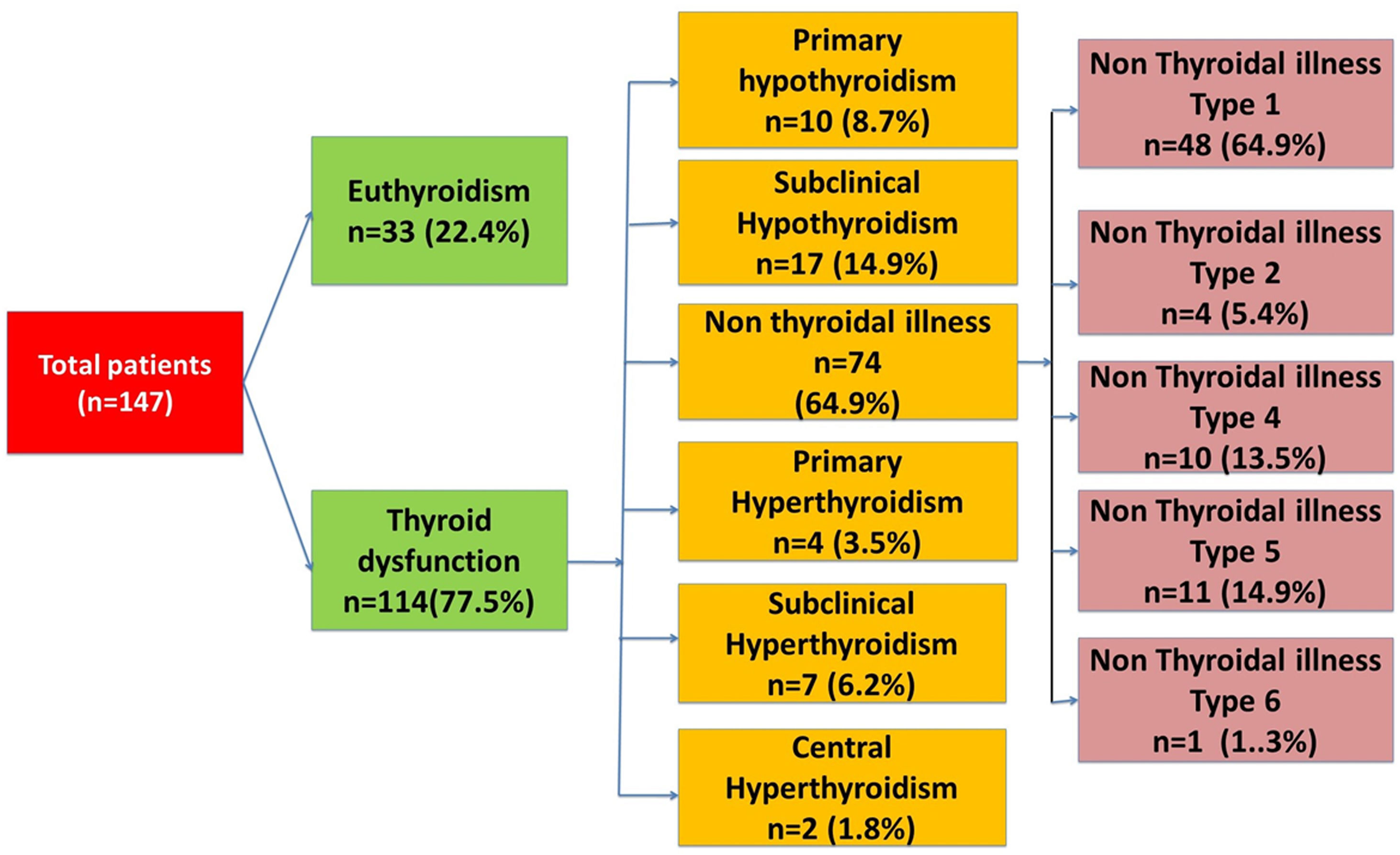
Thyroid dysfunction was seen in 114 (77.5%) patients with acute kidney injury. The spectrum of thyroid dysfunction is given in Fig. 1. Baseline characteristics in the patients with AKI with and without thyroid dysfunction were comparable.
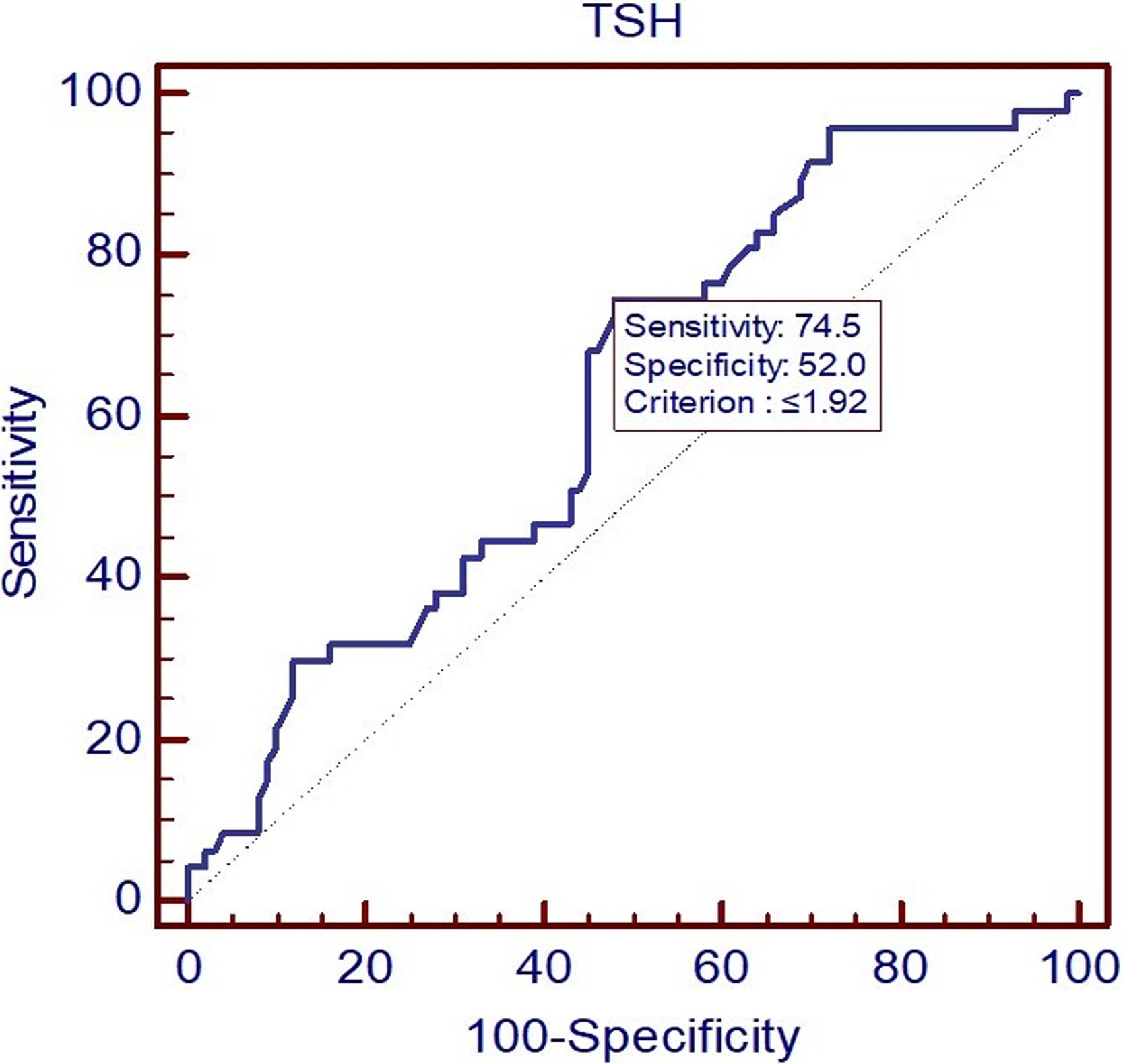
Regarding outcome, 47 (31.97%) patients died in hospital. No significant association was found between the presence of thyroid dysfunction and mortality among patients with AKI (p-value=0.84). However, when we studied the association of type of thyroid dysfunction and in-hospital mortality, it was found that there was trend of increased in-hospital mortality in patients with AKI having primary hyperthyroidism, subclinical hyperthyroidism and non-thyroidal illness as compared to those having euthyroidism, primary hypothyroidism and subclinical hypothyroidism. Patients with AKI having TSH value<2mIU/L were found to have higher mortality as compared to those having TSH value≥2mIU/L (40.70% vs 19.67%) (p-value=0.007). Using a receiver operator curve (ROC) determination, we found that using a TSH cut off of <1.92mIU/L provided the best sensitivity and specificity for in hospital mortality estimation in patients admitted with AKI and this maybe a cut off useful for prognostication in patients with AKI (Fig. 2). No significant association was found between thyroid dysfunction and duration of hospital stay, requirement of renal replacement therapy and number of RRTs in patients with AKI.
Our study confirmed that three out of four patients with AKI have some thyroid dysfunction. Patients with TSH values<2μIU/ml at diagnosis of AKI have double the risk of in hospital death compared to patients with values≥2mIU/L. No large studies have looked at using thyroid dysfunction as a prognostic marker for AKI.
The strengths of our study are the use a more robust definition of AKI and a larger sample with over 60% of patients with stage 3 AKI. However, we did only a single thyroid function test at diagnosis of AKI and did not repeat the sampling during hospital stay or at discharge. The mortality outcomes were also only noted for patients till first discharge and follow up after discharge from hospital was not done.
In conclusion a low TSH value (<2mIU/L) at diagnosis of AKI is indicative of a poorer prognosis and thyroid function tests should be done in all patients with AKI.
FundingIntramural Departmental funds. No other funding.
Conflict of interestNone for all four authors.