A 31-year-old woman diagnosed with SLE in 2012 with joint (symmetrical arthritis of hands, elbows, knees and feet), skin (photosensitivity and malar rash) and serological (positive ANAs, antiRNP and antiDNA) involvement.
Three years later, she presented a nephrotic syndrome with the presence of microhematuria, and a renal biopsy was performed. Renal histology showed class IV lupus nephropathy with a high activity index. Treatment was started with steroids at a dose of 1mg/kg and Mycophenolate Mofetil at a dose of 1.5g/day, allowing partial remission months later, with normal renal function and proteinuria of 1g/day.
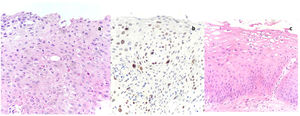
After two and a half years of immunosuppressive treatment, the patient developed condylomas in the genitourinary region, documenting infection by HPV serotype 6 and 51. A cervical biopsy was performed showing the presence of a high-grade cervical intraepithelial neoplasia (CIN), CIN grade 2 (Fig. 1a and b). We initially decided to treat conservatively and to evaluate other therapeutic approaches depending on the evolution of the lesions. The patient was at that time being treated with Mycophenolate Mofetil at a dose of 1g daily, hydroxychloroquine and rennin–angiotensin–aldosterone system blockade, mantaining normal renal function with proteinuria 0.6g/day and microhematuria (10 red blood cells per field). As a consequence of the possible relationship of the infection and tumor pathology with the degree of immunosuppression of the patient and the stability of her underlying pathology in a young patient, we decided to suspend mycophenolate mofetil and introduce everolimus, prioritizing the resolution of the intraepithelial neoplasia.
Uterine cervix histology.
More pronounced atypia in all layers, less maturation, greater differences in nuclear size (anisonucleosis), coarse chromatin and loss of cell polarity characterizes CIN2. This HSIL shows dyskeratotic cells (small cells with eosinophilic cytoplasm and pyknotic hyperchromatic nuclei) in the middle-third of the epithelium. CIN-2 with marked variability in nuclear size (anisonucleosis) (hematoxylin–eosin, 200×).
MIB-1 immunostaining of the cervix highlights positive cells into the superficial 2/3 of the epithelial thickness. Ki-67 staining of CIN-2 (MIB-1, 200×).
Lower epithelial cell layers are characterized by preservation of polarity and uniformly distributed chromatin. In the superficial layer, there is conspicuous cell atypia with binucleation, variable nuclear chromasia and perinuclear halos (koilocytosis). CIN-1 with minimal cytological atypia in lower third of the epithelium (hematoxylin–eosin, 200×).
Actually, after two years of treatment with everolimus at minimum dose (blood levels between 2 and 5ng/ml) the patient maintains complete remission of her lupus nephropathy (normal renal function, proteinuria 0.3g/day and without microhematuria) and achieving the eradication of the condylomas and one of the HPV serotypes in addition to the decrease in grade of the intraepithelial neoplasia (CIN-1 in the last determination) (Fig. 1c). It should be noted that during this period, the patient also presented SARS-CoV-2 infection, without developing pneumonia or respiratory failure, and it was not necessary hospitalization or suspend immunosuppression.
Systemic lupus erythematosus (SLE) is a chronic autoinflammatory disease with immunocomplex deposition that can affect multiple organs and tissues. Lupus nephritis is one of its most common manifestations, affecting approximately 40% of patients with SLE and representing the most important predictive factor for morbidity and mortality. Immunosuppressive therapy is reserved for cases with aggressive histological presentation in order to control inflammation and renal damage.1,2 Patients with lupus nephropathy are exposed to a high immunosuppressive load throughout their lives, which is of greater intensity during induction and of lesser magnitude during maintenance, although for a prolonged period, leading to an increase in adverse effects related to it, including the development of opportunistic infections and neoplasms. Although there is great controversy regarding the duration of immunosuppression in this type of patient, according to the various clinical guidelines, it is recommended that immunosuppression be suspended after three years of maintenance, including one year in complete clinical remission. This decision to withdraw is not without risk, given that a new relapse or recurrence of the disease would mean a worsening of both the renal prognosis and the morbidity and mortality related to the disease.3
For this reason, an intermediate option may be useful, consisting of using drugs that allow less intense immunosuppression once the disease has stabilized, conferring at the same time a lower risk of developing neoplasms, or a better response to the infection/neoplasia already established. The mTOR inhibitors may be a promising solution in these cases.
These drugs are potent inhibitors of the proliferation of both B and T lymphocytes and have an established role in the prevention of rejection in renal transplantation, with a lower rate of nephrotoxicity associated and a higher rate of reduction in the incidence of malignant neoplasms with respect to other immunosuppressants.4
There is little information about use of mTORi as immunosuppressive treatment in patients with lupus nephropathy. In the literature, most of them have been reported in experimental murine models and not in humans, suggesting that these drugs could be applied at least as maintenance treatment in lupus nephritis.5 Lui et al. have showed that the effect of sirolimus applied in murine models before the onset of proteinuria (with delayed development of nephritis) and after the onset of nephritis was proven, with a decrease in the deposit of immunocomplexes in the kidney, improving both the clinical manifestations of the disease and its survival.6,7 Pilot experiments in patients with class III/IV lupus nephritis showed an acceptable tolerability profile in long-term treatment and results that suggest therapeutic efficacy.8
In conclusion, the harmful effects of immunosuppression in lupus nephropathy may condition our therapeutic strategy. The use of mTORi may be an alternative in selected patients, allowing a double beneficial effect: control of the underlying pathology and improvement of adverse events.
Conflict of interestThe authors declare that they have no conflicts of interest.