Diabetes insipidus is an uncommon endocrinological phenomenon in postpartum period and is usually encountered in women with impaired hepatic degradation, multiple gestation, pre-eclampsia, eclampsia, hepatic steatosis and HELLP syndrome (haemolysis, elevated liver enzymes and low platelet count).1 Postpartum diabetes insipidus is a rare entity and is usually associated with Sheehan's syndrome1,2 with associated deficiency of anterior pituitary hormones. Here, we report a rare case of isolated acute-onset diabetes insipidus in a primi mother with good response to 1-deamino-8-D-AVP (DDAVP).
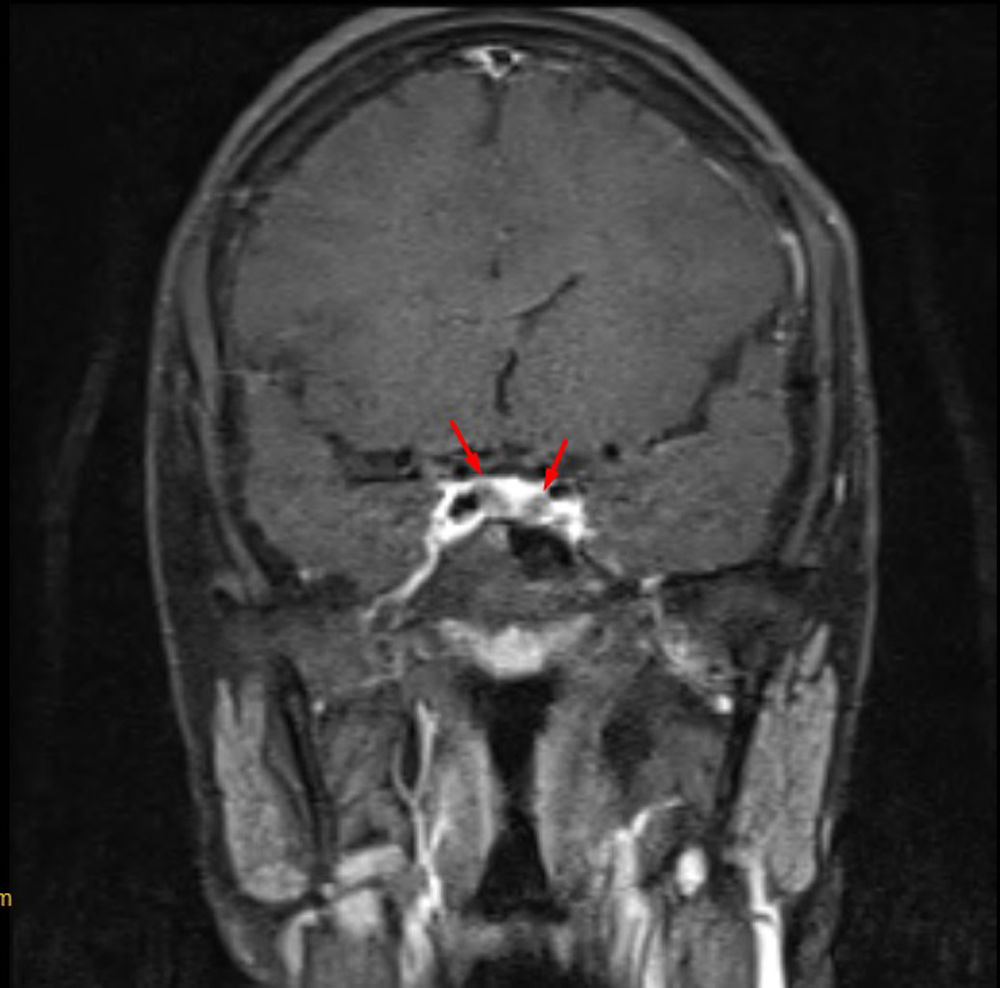
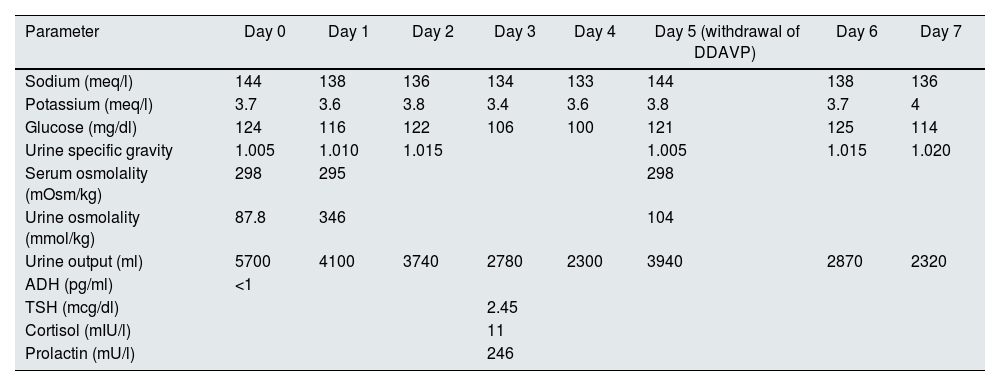
A 24 year old primi mother who underwent lower segment caesarean section (LSCS) at 39 weeks’ gestation due to maternal request and small for gestational age in February 2024, presented to the emergency department with complaints of headache, blurring of vision, polydipsia, and polyuria on the fourth postoperative day. She had no features of pre-eclampsia and she had normal lab parameters during her entire antenatal period. Her baby weighed 2400g and the placenta weighed approximately 400g. On examination, she had a blood pressure of 180/100mm Hg without any focal neurological deficits. She was administered labetalol and intravenous magnesium (4g bolus followed by 2g/h infusion) according to the gynaecological protocol for eclampsia. Her antihypertensives included oral sustained release nifedipine and labetalol. Fundoscopy revealed a normal fundus. Lab revealed serum sodium – 144meq/l, potassium – 3.7meq/l, creatinine – 0.6mg/dl, blood urea nitrogen – 7.4mg/dl, glucose – 124mg/dl, haemoglobin – 11.6g/dl, WBC – 7600/mm3, platelets – 258,000/mm3, glucose – 124mg/dl, bilirubin – 1.1mg/dl, SGOT – 52IU/l and SGPT – 48IU/l. Urine examination revealed sterile urine with a specific gravity of 1005 and proteinuria of 190mg/day without active urinary sediments. The calculated serum osmolality was 298mOsm/kg, urine osmolality – 87.8mmol/kg and she had a urine output of 300–400ml/h. Due to low specific gravity, low urine osmolality, elevated serum sodium levels, and polyuria, she was diagnosed with diabetes insipidus and started on 10μg nasal puff in each nostril twice a day (cumulative dose: 40μg/day). Two hours after the desmopressin nasal puff, her urine osmolality increased to 305mmol/kg and her urine output gradually decreased to 100–150ml/h. Her urine output was 5700ml/day on the first day of admission. She was managed with different intravenous fluids (0.45% normal saline and Ringer's lactate) as per the serial electrolyte levels (Table 1) to ensure euvolemia. Her urine volume gradually decreased to 2.3l on Day 4. Withdrawal of nasal DDAVP on Day 5 of admission resulted again in polyuria with repeat urine osmolality – 104mOsm/kg thereby confirming the diagnosis of central diabetes insipidus. MRI of the pituitary gland revealed a normally sized pituitary midline pituitary stalk with differentially enhanced foci measuring 6mm×4mm and 5mm×4mm in the right and left lateral aspects, respectively (Fig. 1). Abdominal ultrasonography revealed a normal postpartum uterus. Her 8 am serum cortisol level was 11mcg/dl, serum TSH was 2.45mIU/l and serum prolactin level was 246mU/l indicative of an intact anterior pituitary hormonal axis. Her serum ADH was found to be less than 1pg/ml. Her antihypertensives were weaned off to one antihypertensive medication upon discharge. She was transitioned to oral DDAVP (0.1mg thrice a day) on Day 6 and discharged with complete resolution of polyuria and polydipsia. She has stable electrolytes without polyuria on review with complete tapering of DDAVP within 3 weeks. Repeat serum ADH levels was found to be 2.3pg/ml after stopping DDAVP on review after 1 month.
Serial laboratory investigations during the admission period.
| Parameter | Day 0 | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 (withdrawal of DDAVP) | Day 6 | Day 7 |
|---|---|---|---|---|---|---|---|---|
| Sodium (meq/l) | 144 | 138 | 136 | 134 | 133 | 144 | 138 | 136 |
| Potassium (meq/l) | 3.7 | 3.6 | 3.8 | 3.4 | 3.6 | 3.8 | 3.7 | 4 |
| Glucose (mg/dl) | 124 | 116 | 122 | 106 | 100 | 121 | 125 | 114 |
| Urine specific gravity | 1.005 | 1.010 | 1.015 | 1.005 | 1.015 | 1.020 | ||
| Serum osmolality (mOsm/kg) | 298 | 295 | 298 | |||||
| Urine osmolality (mmol/kg) | 87.8 | 346 | 104 | |||||
| Urine output (ml) | 5700 | 4100 | 3740 | 2780 | 2300 | 3940 | 2870 | 2320 |
| ADH (pg/ml) | <1 | |||||||
| TSH (mcg/dl) | 2.45 | |||||||
| Cortisol (mIU/l) | 11 | |||||||
| Prolactin (mU/l) | 246 |
Diabetes insipidus is a hereditary or acquired medical disorder characterized by polyuria, polydipsia, and urine with low specific gravity and osmolality.1,3 It is broadly classified as central diabetes insipidus(DI), which is characterized by deficiency or impaired secretion of arginine vasopressin (AVP) and nephrogenic DI which is characterized by resistance to the action of AVP.3
Postpartum diabetes insipidus can be a part of Sheehan's syndrome or transient gestational DI due to increased vasopressinase activity.1 The estimated prevalence of vasopressinase-induced DI is approximately 2–4 in 1 lakh pregnancies.4,5 The level of vasopressinase decreases to undetectable level approximately 5–6 weeks after delivery, thereby leading to a transient picture of DI.6 Sheehan's syndrome is a notable cause of postpartum hypopituitarism and is characterized by anterior and posterior pituitary hormone deficiency.7 It is usually a result of severe hypotension and shock due to postpartum haemorrhage, manifesting as lactation failure, asthenia, genital hair loss, hypopigmentation, psychiatric disturbances, cognitive dysfunction, and diabetes insipidus.1,7 Vasopressinase-induced DI usually remits by delivery,8 but isolated cases of postpartum DI complicated by placental abruption extending up to four weeks have been reported in the medical literature.1 Our case is unique in that the patient underwent uneventful LSCS without any obvious cause of unregulated vasopressinase release in circulation, presenting with DDAVP-responsive DI. We postulate that the baseline vasopressinase levels might have been high in this patient because of a low birth weight baby, mild intrauterine growth restriction (IUGR) and higher placental weight/birthweight ratio.9 Impaired hepatic clearance of vasopressinase may have contributed to DI, which is evident by concomitant hepatic enzyme derangement. Postpartum DI is commonly observed in multiple gestations, twin pregnancies, assisted In Vitro Fertilization, pre-eclampsia, eclampsia, and hepatic steatosis.1,8,9 DDAVP is resistant to degradation by vasopressinase1,9 and hence it produced an optimal clinical response. This patient came under the ambit of postpartum preeclampsia because the patient presented with new-onset headache, visual blurring, accelerated hypertension, and mild liver dysfunction, which may also have contributed to the pathogenesis of DI.1,9,10 Our patient had transient central diabetes insipidus which settled after 4 weeks which is evident by normalization of serum ADH.
This case highlights the importance of postpartum preeclampsia, higher placental/birth weight ratio, IUGR, and hepatic dysfunction as contributors to the pathogenesis of transient postpartum diabetes insipidus.
Statement of ethicsThis letter of editor was drafted after written informed consent of the patient in conformity with CARE clinical case reporting guidelines.
Financial disclosuresThis case did not receive any special grant or funding from public or private sources.
Authors’ contributionsGerry George Mathew was responsible for conceptualisation, design, writing original draft, editing, visualization, investigation, sourcing and editing of clinical images, investigation results, critical revision of important intellectual content and approving final manuscript. Sharmila Ganesan was responsible for visualization, sourcing and editing of clinical images, critical revision of important intellectual content and gave final approval of the manuscript.
Informed consentWritten informed consent of the patient was obtained prior to the submission of the article.
Conflicts of interestThe authors declare that they have no competing interests.
Data availability statementThe data for substantiating the findings of this manuscript are available with corresponding author and can be made available on request.
The authors acknowledge the wholehearted encouragement of Dr. Nandakumar Chandrasekar, Consultant physician, Kathir memorial hospital who helped in logistics of managing patient, and Dr. Shankaranand, consultant anaesthetist, Kathir memorial hospital for this case report.