We describe a 46-year-old man who presented to the emergency room complaining of pain and paresthesia of the left upper limb of 7 days of evolution. The day before the admission, the patient had also developed palmar and digital cyanosis (Fig. 1a).
The patient had a kidney transplantation six years prior. Before the transplantation, the patient had undergone hemodialysis through a proximal AVF of the left upper limb. The dialysis sessions were discontinued shortly after the transplant was carried out.
On physical examination cardiac sounds were normal, the radial and ulnar pulses were present and symmetrical. The AVF appeared occluded without bruits or thrills. An electrocardiogram was normal and a transthoracic echocardiogram did not reveal sources of embolism.
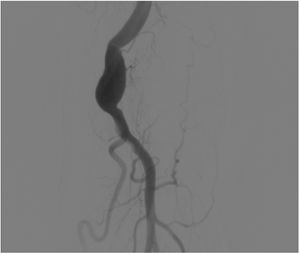
Doppler ultrasound of the left upper limb showed a partially thrombosed brachial artery aneurysm with a length of 25mm. An arteriogram showed a fusiform aneurysm in the brachial artery at the level of the elbow joint. The radial and ulnar arteries, as well as the deep palmar arch, were patent. The digital arteries of the thumb, index and middle fingers were patent, and occlusion, probably embolic, of the digital arteries corresponding to the 4th and 5th fingers was seen. Ligation and resection of the aneurysm was performed, and a brachial to radial bypass was carried out (Fig. 2).
After the surgery, the patient presented marked deterioration in the perfusion of the hand with an increase in pain and cyanosis of the palm and digits (Fig. 1b). An arterial Doppler ultrasound showed bypass patency. Anticoagulation with enoxaparin, aspirin, and statins was initiated with marked improvement with minimal tissue loss over the following 3 weeks (Fig. 1c).
DiscussionUpper limb ischemia due to embolization caused by thrombosed aneurysmal hemodialysis AVF has been reported scarcely in the medical literature mostly due to underreporting.1
The pathophysiological mechanisms leading to aneurysm formation in patients with AVF are controversial.2
We suspect that the patient had atherothrombotic embolization to the and palmar aspect and fingers. The spatial resolution of the angiogram does not allow visualization of skin small vessels thrombotic or embolic disease. The fact that the patient had almost a full recovery with minimal skin damage suggests that this was probably the case. We can only speculate why deterioration occurred following surgery. Embolism from thrombus inside the aneurysm is a possibility. Other sources of embolism were excluded and clinical course suggests that no other sources of embolism were present. We cannot rule out aggravation of hand ischemia during brachial artery cross-clamping. Unfortunately follow up angiogram was not performed since bypass patency was documented by Doppler ultrasound, the patient had improved clinically, and therefore it was decided no to expose the patient to a potentially nephrotoxic iodinated contrast.
When distal upper extremity ischemia resulting from emboli occurs, urgent intervention by thrombolysis or surgical embolectomy has been suggested to avoid a significant risk of limb loss or finger amputation. However, in our case a rather conservative approach with aneurysm ligation followed by anticoagulation with low-molecular weight heparin was successful in preserving hand function with minimal tissue loss.
Since 25–40% of patients undergoing renal transplantation will return to hemodialysis, vascular access is tipically left in place.3 Most AVF thrombose over time with minimal consequences, and therefore AVF ligation in asymptomatic patients with preserved renal function is controversial.4
We conclude that distal embolism from a thrombosed AVF or aneurysm should be considered in the differential diagnosis of acute upper limb ischemia in patients with an AVF. Treatment should be tailored to the degree of digital ischemia, risk of bleeding and other comorbidities, and should include anticoagulation, catheter-directed thrombolysis and surgery.
FundingThe authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interestsThe authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.