Dear Editor,
Polycythemia vera (PV) is a myeloproliferative disorder of unknown etiology. This condition is characterized by the abnormal proliferation of erythroid and myeloid series cells in the bone marrow.1 Focal segmental glomerulosclerosis (FSGS) is a glomerular disease characterized by the presence of nephrotic syndrome, hypertension, and the progressive deterioration of the renal function. Etiology is usually unknown, but it may be seen in secondary conditions.2-3 PV in association with FSGS is rare.4 As far as we know, only eight cases have been reported in the literature.4-10 In the report, we have presented a patient who development of FSGS associated with PV.
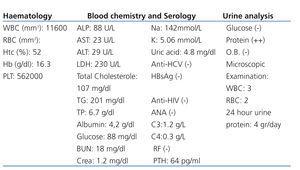
A 46-year-old male patient diagnosed with PV six years earlier was referred to the nephrology clinic due to the detection of proteinuria on routine controls. No important features were found on his history except for his use of the azathioprine for a month. Through a 24-hour urine analysis, 4g/day proteinuria was detected in the patient. The patient was admitted to the clinic. In physical examination is normal without arterial blood pressure of 140/90 and the spleen was 5cm palpable. Renal size and parenchyma were normal in abdominal ultrasonography. Laboratory tests results and examinations of glomerular disease have been showed at Table 1. Hence, causes of nephrotic syndrome were excluded. Renal biopsy was performed. In light microscope were shown 29 glomeruli. Global sclerosis and hyalinization were shown in five glomerule. There was intensive segmental sclerosis in more small segments of the other two to three glomeruli. The also remaining some glomeruli have mesengial cell proliferation and expansion. In Bowmans capsule of one to two glomeruli presence of synechiae noted. Tubulointerstitial area has been examined, focal interstitial mononuclear cell infiltration has been observed. In particular areas of inflammation have attenuation of some tubules epithelium and in the presence of eosinophilic material in the lumen characterized by atrophic changes were observed. In vascular stuctures were normal except for a slight thickening of the wall. Glomerulosclerosis, segmental sclerotic areas and slight thickening of the glomerular basement membrane have been detected through the use of Trichome stain. Furthermore, amiloid staining and immunofluorescence study showed a negative. All above these findings were indicative of FSGS. In arterial blood pressure monitoring, stage 1 hypertension was determined. Perindopril, azathioprine, and ASA were prescribed and the patient was discharged.
FSGS is a clinical and pathological disorder involving primarily the glomerulus.2-3 Progressive glomerular scarring is the most important feature in this disease. Early in the disease process, glomerulosclerosis is both focal, and segmental in nature. Furhermore, in later stages of the disease diffuse and global glomerulosclerosis develops. The loss of filtration barrier, depletion of podocytes and genetic susceptibility are the culprit factors in pathogenesis of FSGS. The condition can be idiopathic or occur secondary to obesity, intrarenal hemodynamic alterations, conditions with glomerulomegaly, the reduced number of nephron, and renal atheroembolic disease.2,3 The tendency to thromboses may occur in PV which one of the chronic myeloproliferative disorders.1 It has been suggested that the increase level of red blood cells, elevation of the platelet count, increase in tissue factor, polymorphonuclear leukocytes, coagulation reactions related to the platelet surface and the presence of microparticles were culprit factors.11
In the light of these data, we hypotezised that PV may cause of FSGS via recurrent thrombosis in microvascular level. Furthermore, it is well known that atheroembolic disease is a cause of FSGS. Thus, our case is important for present to develop of FSGS in the patient with PV. In the existing literature, a small number of cases of FSGS that are thought to be due to PV have been reported.4-10 In addition, 3.6% (only two PV) incidence of FSGS has been reported in patients with myeloproliferative disease.10 It has been expressed in these case reports that hyperviscosity from increased hematocrit, hypoperfusion, predisposition to thrombosis related to elevated platelet counts and the continuation of these conditions in recurrent attacks may have a role on the development of FSGS.9 The emergence of FSGS has been reported average three to seven years after the diagnosis of PV.4-10 In the case of the subject of our study, considering that FSGS has been diagnosed with PV six years later is consistent with the literature. The PV was thought to be the possible reason for FSGS. Additionally, FSGS may occur by occlusions due to the long term recurrent microvascular thrombosis and this also could disorder to glomerular hemodynamics.
Consequently, the co-existence of PV and FSGS seems to be a cause-effect relationship rather than a random combination. Further studies will be needed to demonstrate for a better understanding of this association.
Acknowledgement
None of the authors has a financial interest in any of the products or methods mentioned in this article.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Table 1. Haematological, chemistrical, serological and urinalysis findings of patient