Dear Editor,
We read with great interest the short reviews by José V. Torregrosa et Xoana Barros,1 where the authors discussed the problem of withdrawal the calcimimetic at the time of renal transplantation (RT) which seems to be of high predictive importance in a higher prevalence of hypercalcemia and hyperparathyroidism in these patients. The authors also propose a very practical and clear algorithm for managing hypercalcemia after RT.
Cinacalcet is the only available calcimimetic agent. It was approved for the treatment of secondary hyperparathyroidism (SHPT) in dialysis patients and parathyroid carcinoma. However, cinacalcet isn’t approved for RT recipients and has to be withheld at the time of transplantation.
A rebound hyperparathyroidism (HPT) may be hypothesized to occur, which may increase the risk for persistent HPT and related morbidity.2,3
Surprisingly, the literature on evaluating the effects of discontinuing cinacalcet at the time of RT is very scanty and limited by low patients numbers, retrospective design and data concerning clinical outcomes.4,5
In context of this observation, we would like to present the results of an as yet unpublished preliminary study.
The aim of our communication was to evaluate the impact of cinacalcet therapy on mineral metabolism after RT, up to 12 months.
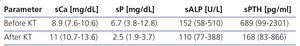
We identified 12 renal transplant recipients (3 females and 9 males), age 38 years (27-56) with hypercalcemia diagnosed after RT, who received cinacalcet before transplantation, dose 45mg/day (30-90) for 6 months (3-12) during hemodialysis (HD); time on HD-38 months (14-71). Multiple assessment of parameters of mineral metabolism was done before and after RT: serum calcium (sCa), phosphorus (sP), alkaline phosphatases (sALP) and intact parathyroid hormone (iPTH). Other causes of hypercalcemia were excluded. Data were presented as median and range.
Elevated sCa was found in all by the end of third month. Significant symptoms of hypercalcemia occurred in 3 pts (walking difficulties, paresthesia, depression, bone pain).
We observed significant differences in all measurements before and after RT. There was the increase in sCa, and decrease in sP, sALP, iPTH; iPTH level still remained above normal range.
Vitamin D (25(OH)D) was within the normal range.
It is worth noting that although tendency toward lowering of iPTH was noticed, increase in sCa was observed.
In conclusion, based on results of our small study, withdrawal of cinacalcet therapy at the time of RT may be a risk factor for hypercalcemia in the early post-transplant period, despite the improvement in iPTH level. In cases of severe SHPT in HD patients decisions on parathyroidectomy rather than cinacalcet therapy should be considered.
Conflict of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1.