Dear Editor,
We comment on a recent study on haemodialysis using high cut-off dialysers for treating acute renal failure in multiple myeloma, and we send our personal experience.
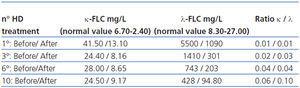
We read with interest the article of Dr. Martín-Reyes et al.1 We agree with the motivation of their study: 1. the survival of the patients suffering from Multiple Myeloma (MM) depend on whether or not they recover renal function, not only due to the complications derived from the renal failure itself, but also from the reduced possibility of access to more effective treatments; 2. the importance of rapid reduction of free light chains blood levels in order to facilitate the recovery of renal function.2,3 We wish to report our experience in this topic In April 2011 a 43-year-old man, with a previously normal renal function, was admitted to our hospital for severe acute renal failure (ARF) of an unknown cause. The review of the clinical history didn’t revealed any previous disease. For 2 months he was suffering from lumbar pain. We started haemodialysis treatment three times a week. Laboratory investigations and bone marrow biopsy detected a lambda IgG MM. We performed kidney biopsy and we observed glomerular deposition of lambda chains, without histological signs of chronic renal damage, and a negative Congo red stain test. In 2 weeks the patient received 10 haemodialysis (HD) treatment with high cut-off (HCO) dialyzer (Theralite®, Gambro Henchingen, Germany). We performed on alternating days HCO HD sessions with standard monitors; they lasted for 5 hours, involved a blood flow of 300ml/min and had an ultrapure dialysate flow rate of 500ml/min. Sodium Reviparine (Clivarina®) was applied at 2400IU in single dose priming. The values of Platelets (60.000/mmc) motivated the prescription on the duration of HCO HD and on the dose of heparin. At the end of each session we didn’t administer albumin. Ultrafiltration was programmed according to the clinical need. Before and after each session, mean free light chain levels were measured in terms of mg/l using nephelometry (N latex test, Siemens) Initially λ FLC concentration was 5500mg/L. At the end of HCO dialyzer HD cycle, the concentration was 94.80mg/L. The concentrations and ratios of light chain levels from the start to the end of treatment are summarised in Table 1.
We didn’t observe any adverse effects. We observed after the first HCO HD a percentage reduction in light chain levels of 74 with dialysis alone before the chemotherapy was initiated. After the third HCO HD the patient started PAD Orlowsky chemotherapy (Bortezomib-Doxorubicin-Dexamethasone) with successful haematological result, but with partial renal function recover. At this moment (10 months after high cut-off dialyzer treatment) the patient is on maintenance HD two times a week. Some reports show a recovery of renal function after several months. We will continue the mixed therapy (HCO HD-chemotherapy according to the protocols of the haematology department) in patients with ARF and MM.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Table 1. FLC concentrations and ratios before and after HCO-dialyzer HD