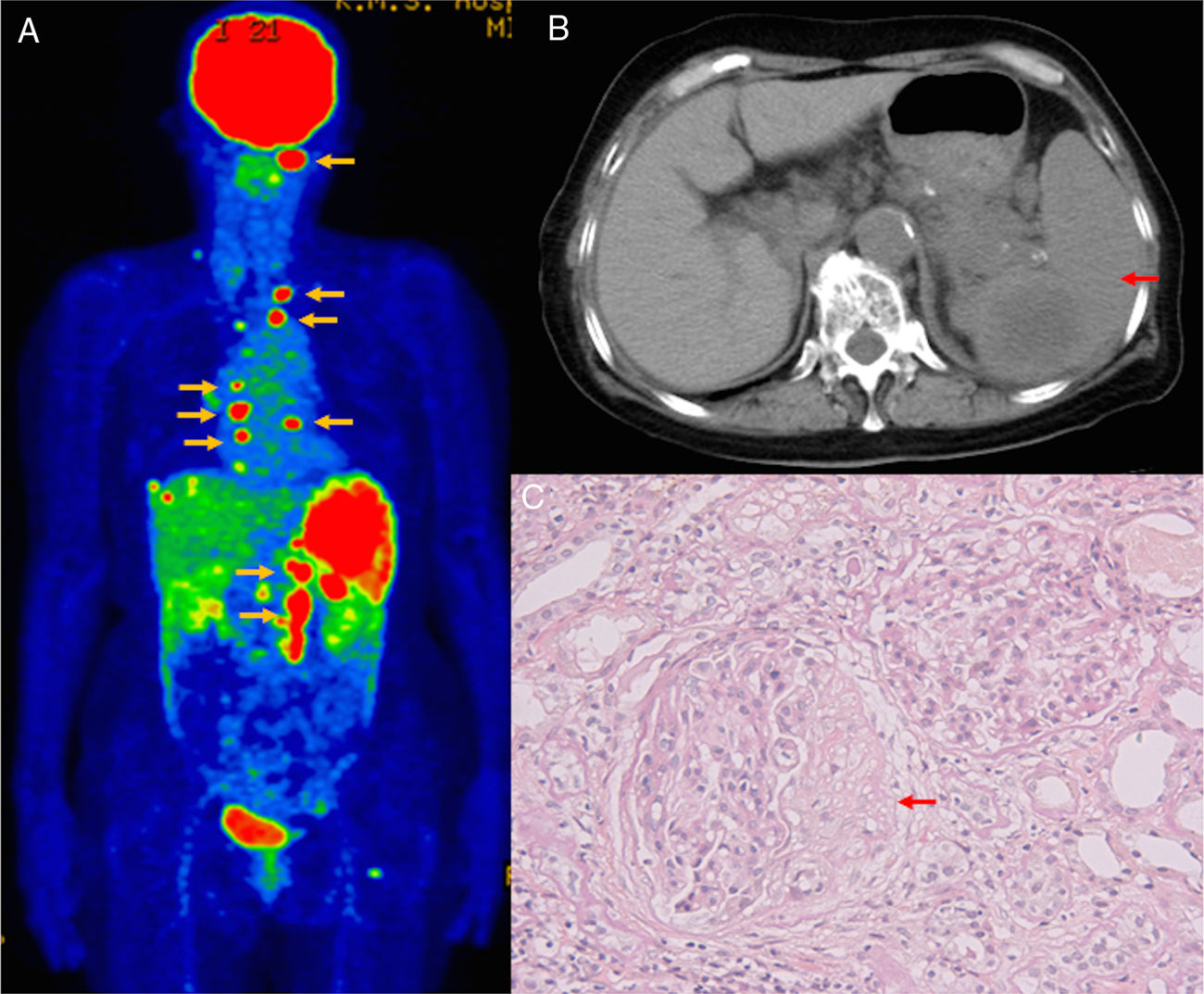
A 70-year-old Japanese woman with a 57-year history of hepatitis C virus presented with nausea, abdominal pain, and renal dysfunction. Physical examination revealed splenomegaly. Blood examination revealed elevated levels of C reactive protein (2.7mg/dL), serum creatinine (2.46mg/dL), blood urea nitrogen (22mg/dL), and uric acid (7.8mg/dL). Test for myeloperoxidase-antineutrophil cytoplasmic antibody (MPO-ANCA) was positive (71.2U/mL). Urinalysis showed proteinuria (0.56g/gCr) and microhematuria (>100 red blood cells/high-power field). 18F-fluorodeoxyglucose-positron emission tomography/computed tomography (FDG-PET-CT) revealed FDG accumulation in the cervical, thoracic, and abdominal lymph nodes and spleen (Fig. 1A). Abdominal computed tomography revealed splenomegaly with a low-density area (Fig. 1B). Renal biopsy specimen showed crescentic glomerulonephritis (Fig. 1C). Abdominal paraaortic lymph node biopsy revealed diffuse large B cell lymphoma (DLBCL). Based on these findings, the patient was diagnosed with ANCA-associated vasculitis (AAV) and DLBCL with suspected splenic DLBCL. Treatment with R-CHOP regimen was initiated, and her renal function improved. However, no remission was noted for the DLBCL. The patient died 4 months later.
Findings of 18F-fluorodeoxyglucose-positron emission tomography/computed tomography (FDG-PET-CT), abdominal enhanced CT, and renal biopsy. (A) FDG-PET-CT shows FDG accumulation in the cervical, thoracic, and abdominal lymph nodes (yellow arrows) and spleen, indicating widespread lymphadenopathy and splenomegaly. (B) Abdominal enhanced CT shows splenomegaly (red arrow) with a low-density area. (C) Renal biopsy specimen reveals crescentic glomerulonephritis with fibrocellular crescent (arrow, Periodic acid-Schiff stain).
Although malignant lymphomas are occasionally complicated by autoimmune diseases,1 complication with AAV is notably rare.2 There have been recent reports of ANCA-positive cases with B-cell lymphomas, especially intravascular lymphoma.3–6 These cases, have included proven3,4 or unproven5–7 AAV. Moreover, an ANCA-positive case with splenic malignant lymphoma without proven AAV, as in this case, has been reported.7 Like the above cases with intravascular lymphoma and/or embolic damage,5 vascular damage caused by B cell lymphomas appeared to predispose the patient to ANCA. There have been reports of successful R-CHOP therapy, including rituximab, for both lymphoma and AAV.3–5 Recently, the RAVE8 and RITUXVAS9 trials demonstrated that rituximab is effective for AAV, especially renal AAV. This is the first case of DLBCL-related AAV with biopsy-proven crescentic glomerulonephritis, and although R-CHOP did not provide lymphoma remission, renal function improved. Thus, rituximab could be effective for improving renal function in AAV. Clinicians should consider the possibility of AAV occurring as a complication in DLBCL.
Informed consent was obtained from the patient for the publication of this article.