In developing countries; traditional, herbal or alternative medicine has huge impacts on patients with chronic diseases. The easy and promised illusion of these products catches attention and drives patients using them. Henna is used traditionally for hair dying and temporary tattooing in Turkey, and many other countries; henna stone also known as German stone is a kind of solid material in which crushed powder form can be used as henna and contains a high amount of p-phenylenediamine (PPD)1 Toxicity of this compound has two phases in human; first allergic reaction with angioedema and the second systemic phenomena occurs with intravascular hemolysis, rhabdomyolysis, and acute kidney injury. Herein, we presented a case of an elderly woman who ingests henna stone in the hope of treating diabetes and had acute kidney failure requiring hemodialysis treatment without the initial allergic phase.
A 73-year-old woman was brought to the emergency room of Hakkari State Hospital with a one-day history of feeling bad, skeletal muscle pain, dizziness, and disorientation. Two days prior to admission, an herbalist advised her to drink crushed henna stone powder in water for her uncontrolled diabetes and to quit insulins. After she did this, symptoms appeared gradually.
Her examination revealed that she was afebrile, oriented and able to communicate. Her blood pressure was 150/80mmHg with a heart rate of 104bpm. There were no signs of allergic reactions or a shortage of breath with oxygen saturation of 95% in room air. In the investigations, hemoglobin was 10.8g/dL, no leukocytosis and a high C-reactive protein level were measured. The other biochemical tests were creatinine kinase 46903IU/L, AST 719IU/L, LDH 1315IU/L, blood glucose 334mg/dL, urea 38.4mg/dL and creatinine 0.75mg/dL. Although there was no chest pain (diabetes may hided), cardiac markers were high. Chest X-ray, electrocardiogram and echocardiography were totally normal. Urine analysis was mildly positive for protein and blood. Renal ultrasound revealed large kidneys with edema. The patient was hospitalized with the diagnosis of rhabdomyolysis. There were no schistocytes in the peripheral smear, serum total and direct bilirubin levels were normal, Coombs tests were negative; detailed serologies including Brucella and Leptospira and other virologic markers were also negative, an upper abdominal ultrasound revealed the only hepatosteatosis. Normoacidemia with limiting bicarbonate level was found in the arterial blood gas analysis. Cardiac markers were decreased in repeated measures.
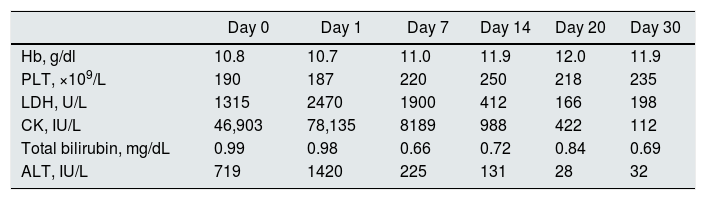
We started appropriate intravenous fluids with bicarbonate infusion just from the emergency room to alkalinize the urine. At first, she did not have an indication for hemodialysis with normal pH, no electrolyte disturbances or any other clinic situation. But reddish-brown urine and oliguria occurred within 24h; edema and renal failure increased gradually. We started hemodialysis treatment with a femoral catheter on the third day of hospitalization. 24-h proteinuria was 170mg/day and urinary sediment was showed one to two white blood cells, one to three red blood cells. Taken into account the most probable diagnosis of rhabdomyolysis, non-severe proteinuria (below 1g/day), age of patient and harmful side-effects of immunosuppressive treatment, we did not make a renal biopsy or give a corticosteroid. Alterna-day hemodialysis and ultrafiltration provided volume control and after the 7th session of dialysis/ultrafiltration, the patient started to have polyuria, a decrease in CK, LDH and transaminases and also clinical symptoms were relieved. On the 14th day of hospitalization, we withdrew the catheter and she was discharged on 20th day with normal urine output and kidney function. First-month control after discharge, the patient was in a good situation with clinical and laboratory parameters. Initial and follow-up laboratory parameters are shown in Table 1.
Laboratory data of the patient through follow-up.
| Day 0 | Day 1 | Day 7 | Day 14 | Day 20 | Day 30 | |
|---|---|---|---|---|---|---|
| Hb, g/dl | 10.8 | 10.7 | 11.0 | 11.9 | 12.0 | 11.9 |
| PLT, ×109/L | 190 | 187 | 220 | 250 | 218 | 235 |
| LDH, U/L | 1315 | 2470 | 1900 | 412 | 166 | 198 |
| CK, IU/L | 46,903 | 78,135 | 8189 | 988 | 422 | 112 |
| Total bilirubin, mg/dL | 0.99 | 0.98 | 0.66 | 0.72 | 0.84 | 0.69 |
| ALT, IU/L | 719 | 1420 | 225 | 131 | 28 | 32 |
In the literature, there are several case reports about PPD toxicity after topical use or suicide attempt. But toxicity occurring after using as a medicine to a specific disease is lesser. Khine YY was reported a man who drank boiled henna leaves for having an unhealthy feeling and Qurashi et al. notified a 32-year-old male had also boiled henna for dyspepsia.2,3 This is the first case using henna or henna leaf as a cure for diabetes.
The tirade for PPD intoxication includes exposure to PPD (local or systemic), early signs of angioneurotic edema and later acute renal failure. A cohort study from Sudan demonstrated that affected patients were more female, of 83.7% were a suicidal attempt and 53.3% had angioneurotic edema. The need for renal replacement therapy as hemodialysis was 86.7%, fortunately, all patients had full recovery.4 It should be kept in mind allergic reaction of the upper respiratory system is not a must as seen in our case but life-treating. It may be about the amount of ingested PPD dose. Higher amounts are associated with higher morbidity and mortality rates. The outcome of renal damage is good with early hemodialysis. There is no antidote for PPD, conservative treatment is only the choice in particularly for rhabdomyolysis.
Hemolysis may be a part of the disease and contribute the renal damage. Henna leaf as known Lawsonia alba may induce hemolytic crisis in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency.5 Hyperbilirubinemia, increased LDH and reticulocyte count should be listed in the differential diagnosis. In the case, the patient had dark brown urine and normal serum bilirubin levels led us to rhabdomyolysis rather than hemolysis. We do not have a chance to measure the G6PD level after recovery to certainly exclude.
To conclude, refined henna/henna leaf or a henna stone has a wide-spread usage area, and intoxication may occur in a topical or systemic implementation. Physicians should recognize the material, be aware of the lethality and prognosis. Public knowledge about traditional herbal medicine should be risen immediately to decrease this kind of herb-induced acute kidney injury.
Informed consentWritten informed consent was taken.
Conflict of interestAuthors declare no conflict of interest.