Transjugular renal biopsies (TRB) are an alternative when percutaneous ultrasound renal biopsy is contraindicated. Few sites are currently carrying out this procedure, with limited literature existing on the indications, complications and diagnostic yield thereof. The aim of the study is to analyze the indications, diagnostic yield, safety and complications of percutaneous transjugular renal biopsies in our site over the last 15 years.
Material and methodsRetrospective descriptive study of all transjugular renal biopsies performed in our site, the Hospital Vall d’Hebron, between 2003 and 2018. For this, an exhaustive review of the clinical records of patients subjected to this procedure during the study period was conducted.
Results56 TRBs were performed during the study period. Out of the patients, 31 were men (55.4%) and 25 were women (44.6%), with a median age of 62 years (IQ range 25–75 [52.5–69.5]). More than half presented with haematuria at the time of biopsy, with a median creatinine of 2.69mg/dL (IQ 25–75 [1.7–4.3]) and median proteinuria at 24h of 2000mg (IQ 25–75 [0.41–4.77]). The mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) were 140±26mmHg and 75±15mmHg, respectively. The biopsy was carried out owing to acute kidney failure in 19 patients, chronic kidney disease in 12 patients and nephrotic syndrome in 10 patients; in 15 patients it was carried out for other reasons. The most frequent TRB indication was technical impossibility in 16 of 56 cases (including infracostal kidneys, obesity and COPD), alterations in haemostasis (n=6), thrombocytopenia (n=5) and solitary kidney (n=7). 12.5% of the biopsies were hepato-renal. Histological diagnoses were obtained in two thirds of the renal biopsies. The average number of cylinders obtained was 2.5±1.3, with the average number of glomeruli being 6.6±6.2. The most frequent histological diagnoses were IgA nephropathy, membranoproliferative glomerulonephritis and thrombotic microangiopathy. Three major complications were observed: fornix rupture and two transfusion requirements due to bleeding and subcapsular hematoma.
ConclusionsIn our site, TRB allowed for a histological diagnosis in 2/3 of patients for whom percutaneous ultrasound renal biopsy is contraindicated. This allowed us to diagnose and subsequently treat said patients.
La biopsia renal transyugular (BTY) es una alternativa a la biopsia renal ecoguiada percutánea en caso de que existan contraindicaciones para su realización. En la actualidad, pocos centros realizan este procedimiento y la literatura acerca de las indicaciones, complicaciones y rentabilidad diagnóstica es limitada. El objetivo de este estudio es analizar las indicaciones, rendimiento diagnóstico, seguridad y complicaciones de la biopsia renal transyugular percutánea en los últimos 15 años en nuestro centro.
Material y métodosEstudio descriptivo retrospectivo que revisa las biopsias renales transyugulares (BTY) realizadas en el Hospital Vall d’Hebrón de 2003 a 2018 para lo cual se ha llevado a cabo una revisión exhaustiva de las historias clínicas de los pacientes sometidos a este procedimiento durante el periodo de estudio.
ResultadosDurante el periodo de estudio se realizaron 56 BTY. Los pacientes fueron 31 hombres (55,4%) y 25 mujeres (44,6%), con una mediana de edad de 62 años (rango intercuartil (IQ) 25-75 [52,5-69,5]). La mediana de creatinina fue 2,69 mg/dL (IQ 25-75 [1,7–4,3]) y la de proteinuria (en 24 horas) de 2.000mg (IQ 25-75 [0,41-4,77]. Más de la mitad presentaban hematuria en el momento de la biopsia. La presión arterial media sistólica fue de 140±26mmHg y diastólica 75±15mmHg. La biopsia se realizó por insuficiencia renal aguda en 19 pacientes, enfermedad renal crónica en 12 y síndrome nefrótico en 10 casos; en 15 pacientes se realizó por otros motivos. Se decidió realización del procedimiento por vía transyugular por imposibilidad técnica ecoguiada en 16 de 56 casos (incluyendo riñones infracostales, obesidad y enfermedad pulmonar obstructiva crónica), alteraciones en hemostasia (n=6), trombocitopenia (n=5) y riñón único (n=7). El 12,5% de las biopsias fueron hepato-renales. Se obtuvo diagnóstico histológico en dos tercios de las biopsias renales. La media de cilindros obtenidos fue de 2,5±1,3, y la media de glomérulos 6,6±6,2. Los diagnósticos histológicos más frecuentes fueron nefropatía IgA, glomerulonefritis membranoproliferativa y microangiopatía trombótica. Se observaron tres complicaciones mayores: rotura de fórnix y dos requerimientos transfusionales por sangrado y hematoma subcapsular.
ConclusionesEn nuestro centro, la realización de BTY permitió el diagnóstico histológico en dos tercios de los pacientes que presentaban contraindicación para la realización de biopsia renal ecoguiada, permitiendo el diagnóstico y posterior tratamiento dirigido en dichos pacientes.
Renal biopsy is the gold standard for the diagnosis of renal parenchymal diseases. Furthermore, it is an irreplaceable tool for establishing the prognosis and treatment of most glomerular, vascular and tubulo-interstitial nephropathies.1 Techniques for obtaining renal tissue for analysis and histologic diagnosis have been modified since the beginning of 20th century from open renal biopsy to percutaneous renal biopsy guided by ultrasound (PRB), which is the procedure most commonly used nowadays.2 The rate of complications is low, it goes from transfusion requirement (0.3–7.4%), to arterio-venous fistula (0.1–0.5%), bleeding requiring surgical intervention or embolization (0.1–0.5%) and even death (<0.1%).3
However, given that the greatest risk of PRB is bleeding, its performance is contraindicated in patients with bleeding diathesis, chronic coagulation disorders, morbid obesity, ascites, uncontrolled arterial hypertension, or small kidneys or a thin cortical.3,4 These clinical characteristics are becoming more frequent since the global trend is to be less restrictive with the group of patients who undergo a renal biopsy5; some nephrologists perform lateral percutaneous renal biopsy in high-risk patients.6 One of the alternatives to PRB is TRB, as it reduces the risk of bleeding,7 it can be performed in patients with technical difficulties (obesity, ectopic kidneys) and allows biopsies of several organs within the same procedure. In addition, using TRB diagnosis is achieved in 60%.8,9
The TRB, in contrast to the PRB, is available in only few centers as it requires greater technical support and experienced interventional radiologists. This is a limitation, probably the cause of the limited number of studies analyzing performance, complications and safety of TRB in patients with a bleeding tendency.8,10,11 The objective of the present study is to analyze the indications, diagnostic performance, safety and complications of percutaneous transjugular renal biopsy in the last 15 years in our center.
MethodsPatientsThis is a descriptive, retrospective, observational study that analyzes clinical, demographic and histopathological characteristics in patients undergoing TRB at the Vall d’Hebrón University Hospital from January 2003 to December 2018. The TRBs were performed by experienced angioradiologists from the Interventionist Radiology Service of the same center.
Method to perform transjugular biopsyFirst, under ultrasound control, the right internal jugular vein is punctured and catheterized after placement of a 9 French vascular catheter introducer. Under fluoroscopic control and with a multipurpose catheter and hydrophilic guide, the right renal vein is catheterized (due to its orientation and angulation, it is the most suitable for inserting the biopsy needle) and supra selectively the vein of the lower pole, performing at this point the transvenous biopsy with the Quick-Core® Biopsy Needle biopsy system (Cook, Inc., Bloomington, Indiana, United States). This biopsy needle consists of a lateral or side-cut needle that is able to obtain longer samples, avoiding fragmentation of the cylinder as compared to the needles by aspiration. The sample is evaluated by a nephrologist using a 20×–40× magnifying glass at the time of extraction and its suitability and the approximate number of glomeruli obtained before the catheter is removed. Then, the sample is maintained fresh and sent to the Pathology Lab.
Variables studiedA total of 21 variables were analyzed, of which 12 were clinical and 8 were lab results (Table 1). The demographic characteristics of the patients were reviewed, as well as clinical characteristics (renal function, presence of hematuria, proteinuria and/or nephrotic syndrome, hemogram and coagulation). At the time of renal biopsy, systolic (SBP) and diastolic (DBP) blood pressure were collected. Hemoglobin level was quantified after performing the procedure.
Clinical characteristics and Lab parameters analyzed.
| Clinical | Laboratory parameters |
|---|---|
| Age | Creatinine |
| Sex | Proteinuria (24h) |
| BMI | Haematuria pre biopsy |
| Systolic and diastolic blood pressure | Hemoglobin pre biopsy |
| Reason for performing renal biopsy | Platelets pre biopsy |
| Reasons for performing TRB | Haemoglobin post BxBiopsy multiple Liver-Kidney INR pre biopsy |
| Biopsy multiple liver–kidney | aPTT (ratio) pre biopsy |
| Number of cylinders | |
| Number of glomeruli | Haemoblobin post biopsy |
| Sclerosed glomeruli | |
| Histologic diagnosis | |
| Complications post biopsy |
TYB: transjugular biopsy; INR: international normalized ratio; a PTT: activated partial thromboplastin time.
Likewise, the clinical/lab data indications for the renal biopsy were reviewed, the reason to perform transjugular biopsy, why multiple liver-kidney biopsies, the morphological characteristics found in the sample obtained (number of cylinders, number of glomeruli, sclerosed glomeruli, implemented pathological anatomy techniques) and the final histologic diagnoses (see supplemental table in Appendix A). Finally, the complications of the procedure were reviewed.
Statistical analysisThe IBM SPSS Statistics 25® computer program was used for statistical analysis. Quantitative variables are expressed as mean and standard deviation if they follow a normal distribution, and as median and interquartile range if they are non-parametric variables. Qualitative variables are presented as percentage. Comparison by univariate analysis between groups was performed by the test t of Student (parametric continuous variables) and by Mann–Whitney (quantitative nonparametric variables). A p<0.05 has been considered statistically significant.
Results of transjugular renal biopsiesBaseline characteristics of the populationDuring the study period there were 56 BTYs performed in our center, 55.4% in men (n=31) and 44.6% in women (n=25). The median age of the cohort was 62 year (IQ) 25–75 (52.5–69.5). In relation with the analytical data prior to the renal biopsy, a 28.57%, n=16 had hematuria. At the time of biopsy, the median creatinine was 2.69mg/dL (IQ) 25–75 (1.7–4.3) and the median 24-h proteinuria was 2g (IQ) 25–75 (0.41–4.77). The mean SBP and DBP pre-renal biopsy were 140 and 75mmHg, respectively. The mean hemoglobin before the biopsy was 10.9mg/dL, platelets 200,000/μL (IQ) 25–75 (81,000–306,000), with an international normalized ratio (INR) of 1.1 and an activated partial thromboplastin time (APTT) of 1.3 ratio. The mean post-biopsy hemoglobin was 10.4mg/dL, with a mean difference between the hemoglobin before and after the procedure of 0.5g/dL.
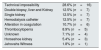
Indication for renal biopsyThe most frequent indication for renal biopsy was acute renal failure (33.9%), followed by chronic kidney disease (21.4%), and nephrotic syndrome (17.9%) (Table 2).
The most frequent indication for performing a transjugular instead of percutaneous biopsy was, after evaluation of all the options by the Radiology service, technical impossibility in 16 of 56 cases (which includes totally infracostal kidneys (n=2), obesity (n=3), chronic obstructive pulmonary disease with postural disability (n=2), presence of cysts (n=2), retroperitoneal tumor mass (n=1), alterations in hemostasis (n=6, 10.7% with a mean INR of 1.7), thrombocytopenia (n=5, 8.9%, with a mean value of platelets count of 45,500/microliter), patients with a single kidney (n=7, 12.5%) and other unspecified impossibilities for percutaneous puncture (n=6, 28.57%). 12.5% of the transjugular biopsies were included liver and kidney (Table 2).
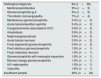
Sample viability and diagnosisUsing the TYB procedure, a mean of cylinders obtained was of 2.5±1.3 and the mean number of glomeruli per sample was of 6.6±6.2. Histological diagnosis was achieved in two thirds of kidney biopsies (Table 3).
Indication for transjugular renal biopsy.
| Technical impossibility | 28.6% (n=16) |
| Double biopsy, liver and Kidney | 12.5% (n=7) |
| Single kidney | 12.5% (n=7) |
| Hemodialysis catheter | 12.5% (n=7) |
| Alteration in coagulation | 10.7% (n=6) |
| Thrombocytopenia | 8.9% (n=5) |
| Unknown | 7.1% (n=4) |
| Horseshoe kidney | 5.4% (n=3) |
| Jehovahs Witness | 1.8% (n=1) |
Histological diagnoses are detailed in Table 4; most frequent were IgA nephropathy, membranoproliferative glomerulonephritis and thrombotic microangiopathy.
Histological diagnosis.
| Histological diagnosis | 64 (n=36) |
| Membranoproliferative | 9% (n=5) |
| Glomerulonephritis Ig A | 9% (n=5) |
| Thrombotic microangiopathy | 7% (n=4) |
| Membranous glomerulonephritis | 5.4% (n=3) |
| Acute tubulointerstitial nephritis | 5.4% (n=3) |
| Cryoglobulinemia associated to HCV | 3.6% (n=2) |
| Amyloidosis | 3.6% (n=2) |
| Nephroangioesclerosis | 3.6% (n=2) |
| Acute tubular necrosis | 3.6% (n=2) |
| Focal segmental glomerulonephritis | 3.6% (n=2) |
| Post infectious glomerulonephritis | 1.8% (n=1) |
| Focal medullary necrosis | 1.8% (n=1) |
| Glomerulonephritis with mesangial expansion | 1.8% (n=1) |
| Minimal change glomerulonephritis | 1.8% (n=1) |
| HIV nephropathy | 1.8% (n=1) |
| Vasculitis | 1.8% (n=1) |
| Insufficient sample | 36% (n=20) |
Eleven patients (19.64%) presented minor complications that did not require invasive treatment. These were: pain (n=2, 3.57%), microscopic hematuria (n=5, 8.92%), jugular peripuncture bleeding (n=2, 3.57%) and asymptomatic perirenal hematoma (n=7, 14.28%).
Three (5.35%) major complications were observed, which were fornix rupture and two transfusion requirements due to contrast extravasation and subcapsular hematoma. There was no need for nephrectomy or death secondary to the procedure.
DiscussionIn the present study we have analyzed the safety and diagnostic capacity of the TRB in our center. From January 2003 to December 2018, there were 56 TRBs performed in patients with a clinical contraindication to percutaneous renal biopsy, and the clinical diagnosis was obtained in more than 60% of the patients.
The transjugular renal biopsy was started in 1900; it was result of an error when performing a transjugular liver biopsy in which, without having foreseen it, renal tissue was also obtained.2 Before TRB, if percutaneous biopsy was not possible to be performed, it was necessary to carry out an open renal biopsy, with the known surgical and anesthetic risk. Cluzel et al. published the study including the largest number of patients; 400 patients undergoing TRB were compared with 400 patients undergoing percutaneous renal biopsy (PRB).8 The main objective of the work was to compare the safety of the TRB with the PBR, the results showed that the TRB is a safe and effective technique. Only one complication is reported in the form of a transfusion requirement, and the histological diagnosis is obtained in 94% of TRB, a figure similar to that of PRB. It is striking that in this work the diagnostic yield is much higher than in our series (94% vs. 64%). This result is probably due to the fact that the mean number of glomeruli obtained was higher (9.8 vs. 6.6). We can infer that this number is higher because the population who underwent TRB in this study presents similar clinical characteristics to those who underwent PRB and, therefore with lower risk of bleeding. By contrast, in our study the patients who underwent TRB had a contraindication for PRB and had a higher risk of bleeding and complications, which is why fewer passes are probably performed and the number of cylinders obtained was lower. Bashir et al. in a series of 27 TRB made in patients with cirrhotic, a population more similar to ours, they obtained an average of 6.7 glomeruli per biopsy.9
The most frequent histopathological diagnosis in our series were IgA nephropathy and membranoproliferative glomerulonephritis. The results are similar to those reported in other studies and concordant with those obtained in the PBR in our center. In the work of Bashir et al. of 27 patients, 40.7% were diagnosed with primary glomerulonephritis and in the series by Cluzel et al. 34.5% of the cases were diagnosed with primary glomerulonephritis.8,9 Thus, it is observed that the most common diagnosis both in our series and in other published ones is primary glomerulonephritis, a potentially treatable and curable entity, so that TRB is a useful diagnostic procedure for patients with contraindications for PRB and in which, otherwise, no diagnosis would have been obtained and, therefore, no specific treatment would have been available.
In our study, there were only three major complications that required medical treatment: two blood transfusions due to anemia without hemodynamic instability, and one case of fornix rupture requiring urgent surgery. However, in the case of patients at high risk of complications, in no case was embolization or nephrectomy necessary. Other complications described in other series are renal vein thrombosis and urinary fistula requiring embolization using coils12 or ureteral stent,13 which did not occur in our patients. In agreement with our study, the series by Rychlik et al., in 67 patients, also reported two cases of transfusion requirement.14 No patient died as a result of the procedure.
In general, the incidence of major complications after TRB reported in the literature ranges between 1% and 20%, the latter percentage published by Abbot et al. in a series of 10 cases.15 Previous studies have shown that a greater number of passes of the needle increases the risk of capsular perforation.10 It is recommended not to exceed six passes in standard-risk patients and not to exceed three passes in patients with high risk of bleeding,8 as those in our series. There is controversy about the relationship between contrast extravasation by venography after TRB and bleeding observed in other imaging tests. While the usual practice of our center is not to perform more needle passes once extravasation begins in significant amount, as assessed by the experienced angioradiologist, Misra et al. postulate that there is not such a relationship.16 Additionally, the relationship between the occurrence of complications depending on the type of needle used is not well established.7,9
Amongst the limitations of our study, we want to highlight that the sample size is small and that it is a retrospective, observational study. Further studies are needed in this field to establish the safety, indications, and performance of the TRB. Nevertheless, our series is the largest published in Spain.
ConclusionsTRB performed by an experienced team is a safe technique in patients with high-risk of bleeding and contraindication for PRB. The TRB allows histological diagnosis in two thirds of the patients in a group of patients with no other alternative method to achieve a diagnosis.
Authorship/collaboratorsMB and CGC share first authorship, while DS and MJS share senior authorship.
FundingPart of this work has received funds from the ISCIII, PI17/00257, and the ISCIII-RETICS REDINREN, RD16/0009/0030.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Bolufer M, García-Carro C, Agraz I, Díez Miranda I, Jaramillo J, Arredondo K, et al. Biopsia renal transyugular. La alternativa a la biopsia percutánea en pacientes de alto riesgo. Nefrologia. 2020;40:634–639.