We present the case of a 33-year-old patient, diagnosed in 2011 with inflammatory bowel disease (Crohn's disease). He presents ileocolitis with torpid evolution, corticodependence and failure of multiple treatments (azathioprine, methotrexate and adalimumab) due to side effects. It is associated to complex perianal requiring drainage of a perianal abscess and follow-up of general surgery.
In December 2014, he was admitted due to progressive swelling, proteinuria of 500mg/dl, hypoproteinemia of 6g/dl, and hypoalbuminaemia of 2.3g/dl. Initially he maintained normal renal function but it deteriorates gradually until Cr 1.7mg/dl. A kidney biopsy was performed with a diagnosis of secondary renal amyloidosis (AA), with intense tubulointerstitial fibrosis. Given these findings, he received 3 boluses of methylprednisolone (500mg) along with the start of monthly infliximab, but again he presented poor tolerance to treatment with biological therapy, and it has to be suspended. The patient remains asymptomatic from 2015 until the beginning of 2020 when he was admitted due to an exacerbation of his chronic kidney disease, with a negative autoimmune study and abdominal ultrasound compatible with chronic nephropathy. During admission the serum creatinine was of 11mg/dl (estimated GFR by CKD-EPI, 5mgml/min/1.73m2), nephrotic range proteinuria 4g/24h, along with hyperphosphatemia, hyperuricemia, metabolic acidosis, and anemia. With a previous diagnosis of secondary amyloidosis (AA), it was decided to start renal replacement therapy with hemodialysis (HD) through a right jugular tunneled CVC in February 2020.
Given the characteristics of his underlying disease, 2 months later it was decided to start HFR-supra with the idea of controlling the inflammatory state associated with the patient's underlying disease.
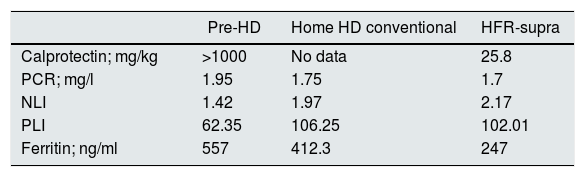
We decided to retrospectively evaluate the inflammatory status of the patient during 3 periods (before the start of HD, with conventional HD and after 2 months of HFR-supra) to assess the efficacy of the treatment both clinically and analytically. CRP, ferritin, INL and IPL were measured as markers of general inflammation and calprotectin as a marker of intestinal inflammatory activity (Table 1).
Inflammatory parameters during the three stages of the patient's treatment.
| Pre-HD | Home HD conventional | HFR-supra | |
|---|---|---|---|
| Calprotectin; mg/kg | >1000 | No data | 25.8 |
| PCR; mg/l | 1.95 | 1.75 | 1.7 |
| NLI | 1.42 | 1.97 | 2.17 |
| PLI | 62.35 | 106.25 | 102.01 |
| Ferritin; ng/ml | 557 | 412.3 | 247 |
HD: hemodialysis; NLI: neutrophil/lymphocyte index; IPL: platelet/lymphocyte index; CRP: C-reactive protein.
Since the change in technique, he has not presented a recurrence of his disease (currently under treatment with colchicine that has not changed), the frequency and characteristics of bowel movements and episodes of pain improved.
Inflammatory bowel disease includes Crohn's disease and ulcerative colitis. They are intestinal diseases characterized by being immune-mediated, with inflammatory activity and of a chronic evolution with flare-ups and alternating with recurrent periods of remission.
The HFR-supra technique combines convention, adsorption, and diffusion. Currently, there are multiple studies that show good results in multiple myeloma,1 in the control of inflammatory markers due to a decrease in pro-inflammatory cytokines, NOS, IL-6 and p-Cresol2–4 and has even shown to be useful in diseases such as porphyria cutaneous tarda.5
Our case explores the usefulness of the technique in systemic diseases with a predominance of inflammation at a local intestinal level. However, clinical trials are needed to confirm this effect. As in other isolated case publications,5 our hypothesis is based on the fact that this technique could eliminate the inflammatory molecules derived from the secondary oxidative stress of the disease itself, with the consequent improvement of the patient's symptoms.
Please cite this article as: Monzón T, Valga F, Henríquez F, Alonso F, Parodis Y, Hillebrand S, et al. Uso de HFR-supra en la enfermedad inflamatoria intestinal: a propósito de un caso en hemodiálisis crónica. Nefrologia. 2022;41:710–711.