SARS-CoV-2 pandemic has changed across the last two years. The development and approval of SARS-CoV-2 vaccines and the emergence of new variants has opened up a new scenario. On this regard, Spanish Society of Nephrology (S.E.N.) Council considers that an update of the previous recommendations should be performed. In the present statement, and taking into account the current epidemiological situation, are included updated recommendations of protection and isolation for patients on dialysis programs.
La pandemia por SARS-CoV-2 ha evolucionado a lo largo de los dos últimos años tanto por la aparición de nuevas variantes como por el desarrollo y administración de la vacunación. La Junta Directiva de la Sociedad Española de Nefrología (S.E.N.) considera necesario actualizar las recomendaciones vigentes de protección y aislamiento para los pacientes con necesidad de terapia renal sustitutiva en programas de diálisis, adecuándolas al contexto epidemiológico actual, situación que ha motivado la realización del siguiente documento con recomendaciones.
Since the start of the SARS-COV-2 ( severe acute respiratory syndrome coronavirus 2 ) pandemic in December 2019 in China, and its arrival to Europe and Spain in February 2020, the number of cases detected in Spain amounts to more than 13 million, with more than 110,000 deaths1. The evolution of the epidemic caused by the coronavirus disease of 2019 (COVID-19) throughout these 2 years in our country has had 7 peaks or waves, which have produced a heterogeneous impact, with a differentiated clinical spectrum that is due to multiple causes2.
Dialysis patients and kidney transplant recipients have been one of the most vulnerable groups during the SARS-CoV-2 pandemic, in which the mortality registered in Spain during the first wave have exceeded 20%2–4. According to data from the Spanish Society of Nephrology (SEN) COVID-19 Registry, there are currently more than 8700 registered patients infected with the SARS-CoV-2 coronavirus undergoing renal replacement therapy in Spain. All the autonomous communities and the autonomous city of Melilla have reported cases. The regions that have included the greatest number of patients in the Registry are the Community of Madrid, Catalonia and Andalusia, a logical circumstance, as they are the most populated.
Since the publication on March 25, 2020 of the Protocol for action in the face of the epidemic of coronavirus disease in patients on dialysis and kidney transplant recipients and the document prepared jointly by the Ministry of Health5,6, more than 2 years have passed, and the reality we face has changed significantly. The factors that have contributed to the change in management include mass vaccination in Spain and the appearance of new variants or strains of SARS-CoV-2 that, at least in the general population, have been more infective but less lethal7. Patients with chronic kidney disease, and especially those with a kidney transplant or those who require renal replacement therapy, have been considered a vulnerable population, so their vaccination has been a priority in all phases8. However, the SENCOVAC study has shown that patients on hemodialysis, peritoneal dialysis but also those with chronic kidney disease without dialysis have developed a robust early humoral response after the SARS-CoV-2 vaccine, especially in those who they had passed COVID-19, and that transplant patients are the most vulnerable population, due to having developed a suboptimal immunization9,10. This has led to the fact that, despite the high vaccination rates, patients with kidney transplants and those on dialysis who were not vaccinated have been the main group of psatients affected, with a high rate of complications, serious illness and even mortality, due to SARS. -CoV-22. Furthermore, the appearance of new strains, such as the omicron variant, has decreased the effectiveness of vaccination and immunization after infections, making reinfections more frequent in patients with chronic kidney disease, but also in the health personnel who care for them daily11,12. However, the current clinical spectrum of SARS-CoV-2 infections has changed, with a decrease in its lethality in all levels.
All these circumstances have turned action protocols into dynamic guidelines, which require continuous updating5,8,13. In this context, and addressing several of the issues raised by Spanish nephrologists, especially with regard to prevention and isolation measures against SARS-CoV-2 infection in dialysis units, the SEN presents this document with the intention of to update the recommendations, taking into account the current epidemiological context and the type of population to which it is addressed. The purpose of this update is to collect the current recommendations with the exhaustiveness required by patients on a dialysis program, including the assessment of the different active infection diagnostic tests (PDIA) available, the management of confirmed and suspected cases and a logistical proposal for isolation in the units.
General recommendations for dialysis patientsAt home and daily life- •
All patients must go to health centers, at least, with a surgical mask or, if available, with a FPP2.
- •
Wear a surgical mask in closed spaces or in crowds and avoid attending crowded places or places with excessive contact with other people.
- •
Wash your hands frequently with soap and water for at least 20 s, or with an alcohol-based hand rub (at least 60% alcohol), especially: after using the bathroom, before eating, after blowing your nose, coughing or sneezing and after direct contact with sick people or their environment.
- •
Perform regular cleaning of surfaces in the home and office regularly.
- •
Do not share toothbrushes, glasses or other utensils with the family or cohabitants.
- •
Avoid contact or maintain a distance of at least 2 m with people who have symptoms of respiratory infection (fever, cough, generalized muscle aches, sore throat or shortness of breath), and do not share personal belongings with them.
- •
Avoid greetings by hugging, kissing or shaking hands.
- •
Try to ventilate the rooms with fresh air, open the windows, without generating sudden changes in temperatures.
- •
All patients must wear a surgical mask before entering the health center and throughout their stay.
- •
Patients that are tested negative, who are not close or suspected contacts, can remove the mask and eat food for the shortest possible time.
- •
The systematic and correct use of masks and gloves for staff and masks for patients must be established, as well as adequate ventilation in the dialysis unit.
- •
Hydroalcoholic solution devices, preferably automatic, will be available to avoid excessive contact throughout the unit, including the patient waiting room, and instruction will be given in their use.
- •
All dialysis patients will be urged to receive full vaccination against SARS-CoV-2, in accordance with the recommendations of health organizations and given the proven efficacy in dialysis patients.
- •
In all dialysis centers, a preventive triage will be carried out upon the arrival of patients (symptoms, temperature, close contact with positive cases). In general, at the community level, close contact will be considered to be any person who has been in the same place of a case, at a distance of less than 2 m and for a total cumulative time of more than 15 min in 24 h without a mask. The period for the definition of close contact will be from 2 days before the onset of symptoms or diagnosis, if the case is asymptomatic, until the moment when the case is isolated14.
At present, 2 DTAI are available in clinical practice: a rapid antigen detection test (RADT) and a viral RNA detection test using a reverse transcriptase chain reaction (RT-PCR) test. The samples recommended for diagnosis by RT-PCR or RAT are performed through a nasopharyngeal exudate, preferably, or oropharyngeal, taken from the upper respiratory tract.
In those suspicious cases, samples of the respiratory tract will be taken for diagnosis, as specified in the protocol of each center:
- a
Upper, by nasopharyngeal/oropharyngeal swab in outpatients.
- b
Lower, preferably bronchoalveolar lavage, sputum (if possible) orendotracheal aspirate, especially in patients with severe respiratory disease and repeatedly negative Diagnostic Test for Active Infection (DTAI)
Regarding the priority method, there is no evidence to differentiate one from the other in terms of sensitivity and specificity in dialysis patients; both have certain advantages and disadvantages to ba taken into account at the time of your choice. RADT cheaper, offers a faster result, although it is less sensitive and requires more time to become positive in the presence of SARS-CoV-2 infection. Currently, RT-PCR is the test of choice. There are 3 types of assays with RT-PCR technology. The first is qualitative RT-PCR, which has high sensitivity, but is expensive, requires specialized personnel, and does not quantify the correlation with virulence; the second, quantitative RT-PCR, which quantifies the viral load, although the relationship between this and virulence is not exactly known; and, finally, the RT-PCR that determines the threshold of cycles and that is characterized by having an adequate correlation between virulence and amplification thermal cycles (Tc)15,16. According to the recommendations of the Ministry of Health, a Tc > 30–35 should be considered negligible in terms of infectivity17. A systematic review by the Center for Evidence-Based Medicine (CEBM) at the University of Oxford on viral cultures for the assessment of the infectivity of COVID-1918 found that it is unlikely that those individuals with high Tc have the capacity to infect and that the lower the Tc, the greater the contagious capacity. In fact, according to the results of 12 studies, the Tc was significantly lower in samples that were able to grow the virus in culture and in 2 studies it was shown that the chances of grow live virus in culture were reduced by approximately 33% for each increase of one unit of Tc.
Given that a large number of patients undergo dialysis in centers outside the hospital without the availability of RT-PCR, it is considered admissible to make the diagnosis of SARS-CoV-2 infection using RADT in hemodialysis units, taking into account that an RT-PCR should be performed whenever possible, especially in patients with symptoms of COVID-19 and with a negative RADT. In addition, patients must always be protected with the FFP2 mask while waiting for the results.
Indication of diagnostic tests for active infection- •
Patient with a suspected infection: Any dialysis patient presenting acute respiratory symptoms consisting of a sudden onset in the last 10 days of any of the following symptoms will be considered suspicious: cough, dyspnea, sore throat or rhinorrhea, headache, nausea or gastrointestinal abnormalities, ageusia, anosmia with or without fever. Other symptoms such as asthenia and hoarseness may also a reason to suspect COVID-19 based on clinical criteria. People infected with the omicron variant may present symptoms similar to those of the previous variants, more frequently they will have a “mild infection”, which includes headache, cough, fever, generalized myalgia, and severe fatigue19. In a systematic review, the pooled percentage of asymptomatic infections was 32% among individuals positive for the omicron variant of SARS-CoV-220.
- •
Patient with close contact: A DTAI will be performed between 3 and 5 days after contact in all dialysis patients who present some serious risk factor, such as active immunosuppression, lack of vaccination or some type of acquired or congenital immunodeficiency. Special protective measures to avoid contact will be maintained for at least 7 days; a DTAI will be repeated during that period before the manifestation of any symptoms.
▪If a patient requires hospital admission for any reason other than COVID-19, there will be followed the preventive medicine protocol of the health center.
▪If a patient is going to be transferred to another dialysis center, action will be taken according to the center's protocol (any of the 2 diagnostic tests, RT-PCR or RADT can be requested) in the previous 48−72 h.
- •
A negative DTAI result will be interpreted as freedom from SARS-CoV-2 disease. However, if there is high clinical suspicion, it is recommended to perform a new DTAI within 3–5 days, since it could be included in the window period. The use, if available, of RT-PCR is preferred over RADT, especially in cases suggestive of being false negatives.
- •
Isolation measure in suspected cases will be, whenever possible, to delay the dialysis session until the result of the DTAI is received. If the center has the facilities available, the patient will be isolated to the best of its capacity. In the event of an emergency dialysis, the session will be held in the COVID-19 room or in a separated place in the room for negative patients (maintaining a safety distance of 2 m) and taking extreme protective measures: FPP2 mask on the suspected patient and on the rest of the patients and FPP2 masks, gown, glasses and gloves for the staff, with strict compliance with universal precautions (hand washing and hydroalcoholic gel).
- •
With a positive case, it is desirable to use the Tc for decision making. In the document of the Ministry of Health on the Strategy for early detection, surveillance and control of COVID-19, updated in December 202121, it is stated that “according to the available scientific evidence, it is assumed that a threshold of Tc > 30–35 would be equivalent to a viral load without infective capacity. However, in that same document it is added "it is not possible to draw conclusions about the level of contagiousness of a person from an isolated Tc value, without epidemiological data". For this reason, in the patient on dialysis, the result of the Tc should be contextualized together with the history and symptoms derived from the SARS-CoV-2 infection:
▪If the result is positive with low Tc (Tc < 30–35), the patient will be considered potentially infectious and close contacts will be monitored and extreme precautions will be taken in all of them.
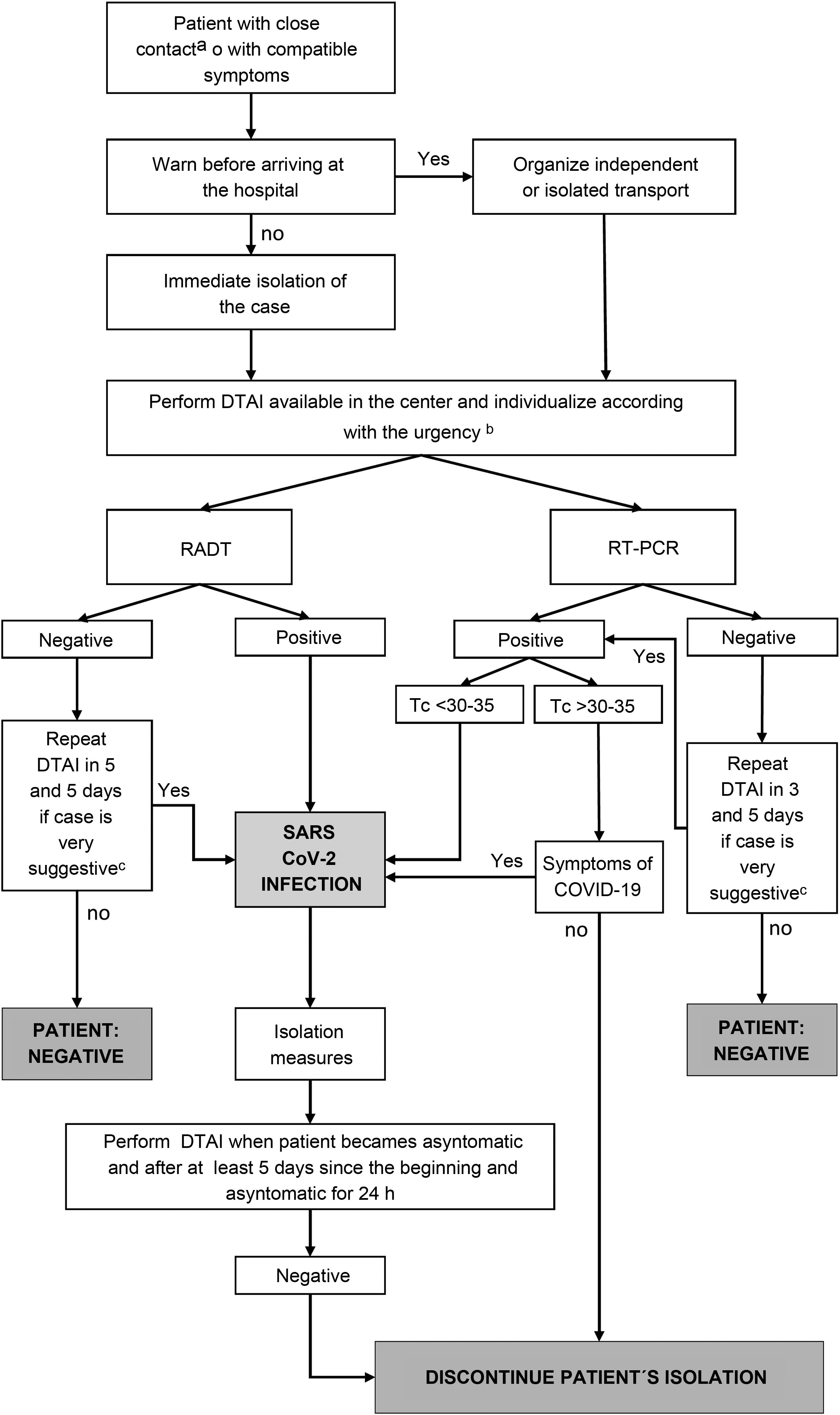
▪If the result is positive with high Tc (Tc > 30–35), it could be 2 scenarios: 1) history of recent infection and absence of symptoms: infection resolved, so it is not necessary to take special measures of caution or 2) no history of recent infection. In this context, 2 situations are considered: a) asymptomatic, in this case, it may be an incipient infection, so the RT-PCR must be repeated at 24 h or b) symptomatic: it may be an active infection in the initial or final stage, which requires, in both cases, special measures of protection (Fig. 1).
Figure 1.Management of SARS-CoV-2 infection in dialysis patients.
COVID-19: coronavirus disease-19; Ct: cycle threshold; DTAI: diagnostic test for active infection; RT-PCR: reverse transcriptase chain reaction test; RADT: rapid antigen test.
aClose contacts should be tested in case of vulnerable patients or high risk of complications of COVID-19.
bIf urgent dialysis criteria, perform RADT; If not, decide based on availability.
cPossible early infection or false negative.
- •
All patients will be urged to notify in advance to the healthcare personnel and follow their instructions if they present symptoms of SARS-CoV-2 infection. Likewise, they will remain at home and will only go out for dialysis sessions with the appropriate prevention measures.
- •
People who show symptoms of possible infection will wear an FPP2 mask during the entire transport journey, the time in the waiting room and during the hemodialysis session. The personnel taking care of these patients will wear gloves, a gown, glasses, and an FPP2 mask.
- •
In the event of a case with compatible symptoms or close contact, a FPP2 mask will be placed, if it was not worn previously, and be separated by more than 2 m from the rest of the patients, both in the waiting room and inside the common room.
- •
RADT will be performed on all suspected patients to proceed with isolation. Given the lower sensitivity of RADT, especially in asymptomatic cases or in vulnerable patients22, we recommend performing an RT-PCR to rule out SARS-CoV- 2 infection in those with suspected infection or in close contacts who test negative.
- •
In those centers that, due to their physical availability and staff, have the possibility of isolating the case, they will be isolated until the result of the DTAI is obtained.
- •
The transfer of suspected patients will be organized I advance, always within the possibilities of the center, by individual or collective ambulance with other confirmed patients (provided that all occupants wear a FPP2 mask and with the greatest possible ventilation) or by their own means (avoiding public transport).
- •
In suspected or confirmed patients, their stay in the waiting room will be avoided, as much as possible, by adjusting the session time. If there is enough space in the waiting room, an area will be set up for patients with COVID-19 and, if not, they will be located at a distance of at least 2 m, also having adequate ventilation. Likewise, the use of FPP2 will be guaranteed for all patients. If there is more than one case, these patients will be scheduled on the same shift.
- •
Suspected or confirmed patients must take extreme precautions and reduce social interactions as much as possible, constantly using the FPP2 mask and maintaining adequate hand hygiene.
- •
The dialysis session of these patients will be performed preferably in rooms or boxes under contact and droplet isolation conditions. Since this resource is not available in most centers, dialysis will be carried out in the common room with the following measures in order of preference and always depending on the resources of spaces and people in the center:
▪Dialysis units that have physically isolated rooms with an independent entrance circuit will use these spaces for hemodialysis sessions for suspected or infected patients.
▪In the units that do not have physically isolated rooms with an independent entrance circuit, infected or suspected patients will undergo dialysis in a part of the general room, outside the passageways, with a minimum distance of 2 m between patients and ensuring good ventilation.
▪If several patients suspected or infected by SARS-CoV-2 are dialyzed, they will do so in nearby posts and attended by the same staff. Entries and manipulations will be limited to those strictly necessary.
▪Whenever possible, COVID-19 positive patients will be dialyzed at the end of the day and on the same shift. After the hemodialysis session for patients with COVID-19, the room will be cleaned and adequately ventilated. The waiting time to occupy the room between shifts will depend on the number of renewals/hour, as established by the Centers for Disease Control and Prevention in the document Guidelines for environmental infection control in health-care facilities (2003)23.
- •
If a home hemodialysis monitor with bags is available, dialysis can be performed in the hospital area designated for infected or suspected patients, maintaining isolation.
- •
For the hemodialysis sessions of patients with SARS-CoV-2 positive, the room for patients with hepatitis B virus infection will be used, ensuring that measures are adopted to avoid the transmission of both SARS-CoV-2 (airway) and the hepatitis B (blood route). To this end, we make the following recommendations:
▪Under no circumstances will patients with COVID-19 and those with hepatitis B surface antigens (HBsAg) be simultaneously in the same room.
▪After the HBsAg-positive patient session, the room will be cleaned and disinfected, including vertical and horizontal surfaces, tower and equipment. Special attention will be paid to the surfaces most frequently exposed to hand contact (knobs, switches, sink, controls, telephone, bedside table, armchair, bed, curtains).
▪All monitors and devices (carts, blood pressure monitors, infusion pumps…) will be changed to prevent materials from HBsAg-positive patients from being used for these patients.
- •
Suspected and confirmed patients will wear the FPP2 mask throughout the dialysis session and avoid food intake.
- •
If an outbreak occurs (defined as a group of 3 or more cases related to the dialysis unit), the hospital center's preventive medicine managers will be notified (and the nephrology service to which it depends, if it is a dialysis center outside the hospital) and proceed according to your indications.
- •
In the rooms dedicated to suspected or positive patients, all accessorymaterial that is not essential for the dialysis session will be removed. If necessary, it will be supplied to the medical or nursing staff in contact with the patient by the auxiliary staff, to avoid unnecessary displacements.
- •
The material that is expected to be necessary for the dialysis session will be prepared in advance and will remain next to the dialysis monitor.
- •
Disposable material will be used, as much as possible.
- •
Non-disposable material, such as blood pressure devices, saturimeters or infusion pumps, will be properly cleaned and disinfected after use.
- •
The suspected/confirmed case should not go to the AVF washing room or the changing rooms. The patient must carry out a prior washing of the AVF at home and complete the disinfection procedure with alcohol at the dialysis station.
- •
Environmental hygiene will be reinforced with disinfection before and after the dialysis session in the room, placing special emphasis on its ventilation.
- •
The dialysis machine used in a suspected or confirmed case of COVID-19 may then be used for another patient, carrying out the usual internal disinfection and adequate external disinfection with sodium hypochlorite or any approved viricidal disinfectant for external use.
- •
Nebulizations will not be carried out during the dialysis session.
The median incubation time for SARS-CoV-2 is 5–6 days, with a range of 1–14 days. Transmission of the infection is currently considered to begin 2 days before the onset of symptoms. The level of transmissibility depends on several factors, but above all it is based on the stage of the disease and the severity of the symptoms.
The infective period of mild cases would occur mainly in the first week of the presentation of symptoms, from 2 to 3 days before to 7–8 days later. In the most severe cases this transmission would be more intense and lasting.
The first DTAI to assess the infectivity of the infected patient, with a view to ending isolation, will be performed, if the patient is asymptomatic, from the 5th day of infection, as recommended for the general population24.
- •
There is considerable agreement on establishing the end of isolation due to COVID-19 on asymptomatic hemodialysis patients if there is a negative DTAI result (either RADT or RT-PCR) or if RT-PCR is positive at high cycles (Tc > 30–35), taking into account that the patient will continue to undergo dialysis with a mask, like all patients in the unit (Fig. 1 ).
- •
In cases with mild/moderate symptoms, a negative DTAI is recommended 5 days after the onset of symptoms, provided that at least 24 h have elapsed since their resolution.
- •
In severe cases or in immunosuppressed patients (for example, in those patients receiving immunosuppressive treatment, solid organ or bone marrow transplant recipients, hereditary immunodeficiency, poorly controlled HIV…) it is recommended to perform an RT-PCR and be negative 48 h before the end of the isolation.
The following patients will be considered particularly vulnerable cases and with a higher risk of contagion in the dialysis unit:
- •
Patients who have not received full vaccination or with a negative humoral response to the vaccine.
- •
Patients returning to dialysis after a kidney transplant.
- •
Especially immunosuppressed patients (see previous section).
Extreme precautions will be taken with these patients, they will always wear an FPP2 mask (if available in the center) and they will avoid close contact with suspected or confirmed patients who are undergoing dialysis in the unit, both in the waiting room and in the dialysis room.
Suspicious and confirmed cases in the peritoneal dialysis unit- •
Each case will be evaluated individually and, if the patient does not require medical care, the clinical revision or the evaluation of the procedure will be postponed and the pertinent instructions will be given so that they remain at home.
- •
If medical assistance is required, the transfer of suspected patients by individual ambulance or by their own means (avoiding public transport) will be arranged in advance, if possible.
- •
Will avoid to stay in the waiting room so that, upon arrival, the patient will be transferred directly to the out patient clinic designed for the care of these patients, or to the hospital emergency room, according to the protocol of each center.
- •
Patients who come outside of the established hours must follow the usual circuit of each center.
- •
"Contact and droplet isolation" will be indicated for the duration of clinical care for the patient in the dialysis unit, according to the measures indicated by the preventive medicine service of the responsible hospital.
- •
Environmental hygiene will be reinforced with disinfection of the room before and after the care of the patient.
- •
An attempt will be made to reduce the time spent in the hospital, avoiding non-urgent tests, such as peritoneal balance tests, training, peritoneal exchanges, etc.
- •
While the infection lasts, teleconsultation or virtual consultation will be offered as the first option.
- •
These patients will be cared for by exclusive personnel and with the corresponding protection measures.
The protection and isolation measures for patients with SARS-CoV-2 infection must be accompanied by the surveillance and protection of the health personnel who care for them, individualizing the need for DTAI in accordance with the recommendations of the center's occupational health services.
All recommendations offered in this document may vary and must be understood within the epidemiological framework of the date of publication. In addition, the updated recommendations of the competent health bodies must be known and followed, since these recommendations are general and are not intended to replace the specific protocols of each hospital.
Conflict of interestThe authors declare that they have no conflicts of interest related to the manuscript.
The authors express their gratitude to the nephrologists who have commented on this document during the public review period.
Formada por: Patricia de Sequera, Gabriel de Arriba, Borja Quiroga, Miquel Blasco, Gema Fernández Fresnedo, Marian Goicoechea, Sagrario Soriano, Emilio Sánchez-Álvarez, Francisco Javier Pérez Contreras, Auxiliadora Mazuecos, Marian Goicoechea, Manuel Gorostidi, María José Soler, and Mariano Rodríguez Portillo.